The Benefits of Breast Cancer Screening
Interview with
Is breast cancer screening beneficial? A paper in the Lancet this week examines the pros and cons...
Professor David Cameron at Edinburgh University is one of the authors on that paper.
David - There has been for some time, a controversy in the area of whether women should undergo regular mammographic screening to try and pick up cancers before they are obvious to the patient or the doctor. The controversy has really ended up with two polarised views. One saying, this process works. It prevents women dying earlier of breast cancer and another view that says, it picks up lots of cancers that never needed to be found, doesn't make much difference to whether women survive breast cancer and therefore, should be stopped.
Chris - So you were then consigned the unenviable task of looking at this data to try to answer that question. Not an easy job to do. How did you do it?
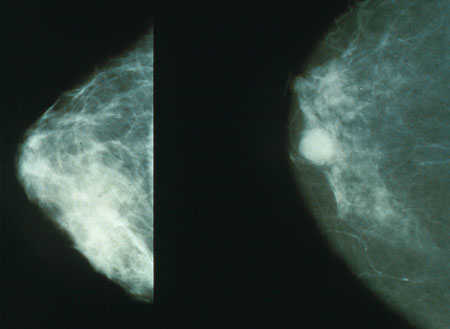 David - We focused on two key points. What were the mortality benefits and what were the harms? Particularly the harm of what's called 'over diagnosis' and that is a technical term. What it means is a cancer that is found through screening, that is a real cancer, but it's a diagnosis of a cancer that would not have otherwise come to light or cause clinical problems in a woman's lifetime.
David - We focused on two key points. What were the mortality benefits and what were the harms? Particularly the harm of what's called 'over diagnosis' and that is a technical term. What it means is a cancer that is found through screening, that is a real cancer, but it's a diagnosis of a cancer that would not have otherwise come to light or cause clinical problems in a woman's lifetime.
Chris - How do we know that a cancer detected at stage X would not have killed that person?
David - For an individual woman and then for her individual cancer, we cannot. And so, you can only deduce the existence of this group of cancers through the analysis of pooled data, either from randomised trials or from observational studies.
Chris - And how did you do that?
David - The approach we took was to first go back to randomised controlled clinical trials. The big advantage of a randomised trial is that provided it's reasonably well-designed. The only difference between the two groups of women is whether or not they have mammographic screening.
Chris - Because what one doesn't want to do and this has been a certain criticism levelled that some of the data from America for example with things like prostate cancer, where America is extremely proactive about screening people and then diagnosing, and treating people with prostate cancer, people have said there's a lead time bias. You diagnose people and actually, you look like you're achieving an incredible response rate, but were those cancers not picked up until later and then treated anyway, the people would have ended up with the same outcome.
David - Exactly and we did look at quite a lot of observational data and some of the observation studies have been very well conducted in a sense that the authors have tried everything they can to control for things like lead time and underlying differences in breast cancer incidents. But they all tend to rely on some key assumptions including what would have happened in that population, had breast screening not been conducted. We did an interesting modelling exercise changing various assumptions, but working on the same dataset, and showed you could draw quite different conclusions.
Chris - How did you draw the conclusions that you did?
 David - Let me address the question of how we came to the conclusion that breast cancer screening does reduce the mortality for breast cancer. We took the hazard ratios for breast cancer screenings from these trials where we had 13 years of patient follow up after the end of the trial. Because if you're going to catch a cancer early in order to reduce a chance of a woman's dying, you need to measure her risk of dying from breast cancer. Not just during the trial, but for many years after. Now, our conclusion was that there was a 20% reduction in breast cancer mortality in these trials.
David - Let me address the question of how we came to the conclusion that breast cancer screening does reduce the mortality for breast cancer. We took the hazard ratios for breast cancer screenings from these trials where we had 13 years of patient follow up after the end of the trial. Because if you're going to catch a cancer early in order to reduce a chance of a woman's dying, you need to measure her risk of dying from breast cancer. Not just during the trial, but for many years after. Now, our conclusion was that there was a 20% reduction in breast cancer mortality in these trials.
Chris - How many lives saved does that turn into?
David - Well, what we then did was to say, let's look and see what happens in the UK where we have a 20-year breast cancer screening programme for women, age 50 onwards. We took their risk of dying of breast cancer between the ages of 55 and 79, and so, we back-extrapolate it to work out what the mortality would be without that 20% reduction, which works out at about 1300 women a year not dying from breast cancer because of breast cancer screening.
Chris - What about the converse which is, people have picked on the number which has appeared in the paper in the Lancet saying, "Look, there are thousands of people who are now having interventions that they needn't have done." What can we say about that group?
David - We took the same approach. We started with our randomised trials, but critically, if you're going to measure over diagnosis, you need to have a control group who are never screened, and many of the studies offered or systematically screened the women in the control arm at the end of the trial. So we took the only trials where there was no exit screening. So that left us just 3 trials to look at for our estimate of over diagnosis. So we took these 3 trials and we estimated the risk of an over diagnosed cancer and our conclusion was that in the UK approach to screening, that about 19% of the cancers found during the time of screening would be an over diagnosis. That translates to a figure of about 4,000 women a year, but the precision of that figure is less than the precision for our mortality benefit. But nevertheless, it is a real number of patients who have a cancer that they didn't need to know about.
Chris - And what are the implications of these numbers?
David - The significance of the over diagnosis number is firstly that women need to be aware that this is a risk or a price that they have to pay if they're going to undergo screening. They may have something found that wasn't necessary to be found. However, we can never work out who they are, so they need to continue to be treated exactly the same way. But it offers an opportunity for research to further explore how we could identify these cancers that we didn't need to discover. From the mortality point of view, our primary conclusion was that the breast cancer screening programme should continue because we felt 1,300 lives a year was well justifying the continuation of the breast cancer screening programme. But the women, when they're invited, should therefore be given a bit more information about the down sides, the harms, and more open discussion about the treatment options when something is found.









Comments
Add a comment