Cancer and Immunity
Interview with
The majority of cancers are not transmitted but arise spontaneously in the body. So, why doesn't the immune system deal with that? This is the question that PhD student Richard Wells is looking into at Cancer Research UK's Cambridge Research Institute.
Richard - So, our lab is trying to work out why it is that the immune system can't stop cancers from growing in people. It's been known for a very long time that tumour cells, these rouge cells that grow very fast and in a totally inappropriate way. They're so unusual and they're so strange that immune cells that normally are looking for bacteria and viruses, and that sort of thing actually realise that these cells are broken in some way and that they shouldn't be there. But, obviously, the unfortunate thing is, that people with a very healthy immune system still get cancers. So, there must be a way that tumours are trying to escape that?
Chris - Why should the immune system attack the tumour because they are after all your own cells?
Richard - That's a really puzzling thing about it. When this was first suggested in the '50s, people thought those who'd raise the idea that they were mad because you know, these are human cells. But it looks like the cells are so stressed and so damaged that they might start producing molecules that act as a trigger. In the same way that if you were to cut 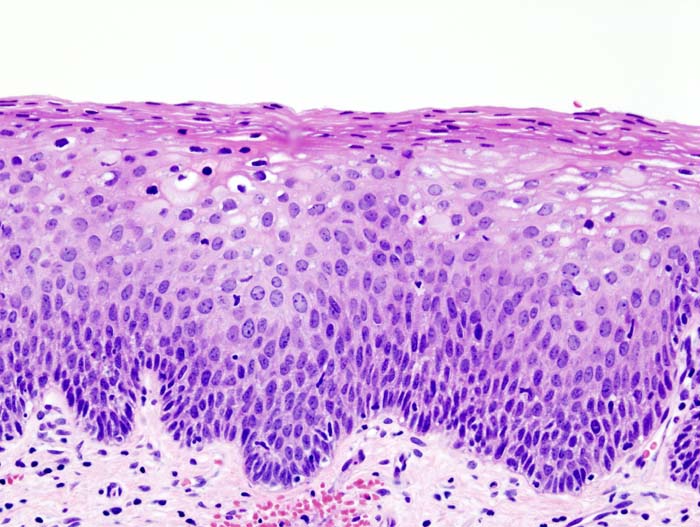 your arm, it goes red and hot, and that's immune cells going in. And the reason that they go in there is because that they're dead and dying cells, and that also is something we see in cancers. There are cells that are very, very stressed and they're working really hard to fix themselves, but when they do that, they're putting out all sorts of signals that say that they're not right and may not be working properly, and that also goes in immune cells. Some people have called a tumour 'a wound that never heals'.
your arm, it goes red and hot, and that's immune cells going in. And the reason that they go in there is because that they're dead and dying cells, and that also is something we see in cancers. There are cells that are very, very stressed and they're working really hard to fix themselves, but when they do that, they're putting out all sorts of signals that say that they're not right and may not be working properly, and that also goes in immune cells. Some people have called a tumour 'a wound that never heals'.
Chris - So, you should have the equivalent of the red arm that you're wounded in your cancer, but you don't. So, something unusual is going on. The cancer is in some way preventing that from happening?
Richard - Yes, so what we get is, we get the sort of the red flare at the very beginning that says there's something wrong, but what we never get is that they will fix it and we get rid of what's wrong. And that's the bit where - there are sort of two bits to your immune system and the first bit is the cells that come in and makes it red, and makes it inflamed, and says, "Look, there's something broken here. There's something not right." Those guys coming into cancers and they're doing their job really well. Unfortunately, the second set of cells that's supposed to come in and kill off anything that's broken, they aren't actually doing their job.
Chris - It's not that a cancer is a mixed bag. There are lots of cells, some more damaged than others, and some of them do get deleted in this way, a bit like you're saying, the immune system comes and then whacks those out. But then there are other cells, a little bit more normal at least to start with, maybe the cancer gets away with having those cells, the immune system is prepared to let them go. Is that possible?
Richard - So there's two big theories as to how these tumours might be getting away with what they're getting away with. Some people think the tumour cells manage to make themselves look quite normal and the ones that look the most normal don't get killed. But actually, although we all think of the tumour cell, the rouge cell, it's dividing; actually, they pull in loads of other different types of supporting cells.
Chris - What? They attract those cells to come in to the cancer from elsewhere?
Richard - Yeah, so it's exactly the same again as like a wound. In a wound, it pull in all of these networks of cells, they form a mesh around and help the wound to fix itself. And what we found is that one of them, it's very, very potent in its manner of stopping immune cells from working.
Chris - Wow! So, the cancer is recruiting a totally different non-cancer, a healthy cell to come into the cancer, and that cell is in turn, turning off the immune response?
Richard - That's absolutely right.
Chris - So, you get these local immune control or suppression really where the cancer is, allowing it to escape under the immune radar, and the immune system ignores it?
Richard - Absolutely, yes. And there's only one type of all of these types of cell and it seems to be, one of them is enough to stop the second type of immune response that's very, very specific, and the cell it longs to kill.
Chris - Why doesn't my sore arm recruit those same cells and turn off the immune response? Why is it only in cancer that this happens?
Richard - So, it seems to be that if you're trying to fix a wound, there's a certain amount of sort angry immune cells coming in which is a good thing because it cleans it up. It gets rid of everything, but there has to be a flipping point where you start to say, "Okay, I've had enough sort of angry cells coming in and I have to try and calm this all down. I have to try and make everything go back to normal and it can fix itself." And what we get in the tumour is that you get the angry bit, but it then lives for many, many years in a state where everything is calming down and sits there, growing within a network that's supposed to just be there for a few days, weeks, something like that.
Chris - Can you get rid of these cells?
Richard - So, we can in animal models at the moment and that's proven to be very, very effective and we can actually completely control tumour growth of pancreatic tumours in mice. And these tumours are very, very difficult to control with drugs and in human patients, the survival of pancreatic cancer is very, very poor. It's harder to translate that into a human patient because what we've since worked out is that, as I said, these are totally normal cells doing a normal thing. And they seem to have really important roles in all tissue. So, the approach that would be the obvious one was to say, "Let's just get rid of these cells." Actually, unfortunately, it's very hard to do and will cause real problems for a patient. But what we're trying to work out is precisely what in the tumour makes them different. Can we find a drug that's really specific to stop what they're doing in the tumour?
Chris - Or stop them going into the tumour in the first place?
Richard - Indeed, so that's the second sort of way that we're also looking at saying, where do they come from and how are they getting there. It's possible that there's a mixture. Some get pulled in from the bone marrow, so the bone marrow tends to be this big factory that produces all sorts of different types of cell that go around the body. And we think some of them go from as far as the bone marrow, all the way through your blood and into your tissue.
Chris - What are these cells called?
Richard - So in general, the cells that support a tumour are called stromal cells. They're sort of a network. So, what we call this cell is the FAP positive stromal cell because we found that the protein that marks it very specifically is FAP (fibroblast activation protein).
Chris - And if you look at a lung cancer, is it equally likely to have these cells in it as a bowel cancer, a pancreatic cancer, or even a brain tumour?
Richard - So, there's different subtypes of tumour and the one that we're looking at is adenocarcinoma. It's this one type of carcinoma that comes from glandular tissues and if you look in human adenocarcinomas, the FAP positive cell is present in almost all of them.
Chris - An amazing thing to be working on during your PhD which could culminate actually a really effective treatment for cancer. Is that not awe you a bit? Or sort of blow your mind to be thinking you're working on something that is really that cutting edge therapeutically?
Richard - Yeah, it's very exciting. I mean, particularly as I'm training to be a doctor as well. It's really great to see work that's coming through that can operate both at the basic science of it, but to see where it's going and to see that it could help patients is fantastic.
PhD student Richard Wells.









Comments
Add a comment