Ras, Raf, Mek, Erk: cell signalling and the future for cancer treatment?
Interview with
Chris - We're now in the stage in our understanding of cancer where we won't be treating a specific cancer such as bowel cancer just because it's bowel cancer. But it will be bowel cancer associated with particular genetic changes and what one person's bowel cancer may have in genetic changes could be different from another's. And what we know now from 30 years or more of research is that many of those genetic changes affect what we call cell signalling. And so, signalling controls when a cell is going to grow, multiply, whether it's going to die or survive or whether it's going to move and these are the three principles at what goes wrong in cancer cells - grow where they shouldn't do, they multiple when they shouldn't, and they survive when they should die.
Kat - And so, what actually are these signals that are going on in cells. We think about signals, maybe like semaphore or Morse code or a mobile phone signal now. How do cells signal?
Chris - Of course, it's molecules which are signalling and what happens is, cells respond as we all do to signal us to do something for a cell to proliferate and multiply it will be a growth factor signal which will drive the cell into cell division. But for that signal to act on the cell, it has to be relayed into the cell's nucleus and it does that by a sort of molecular relay, almost like a relay race where one molecule passes a piece of information to another, and eventually, the message ends up in the nucleus.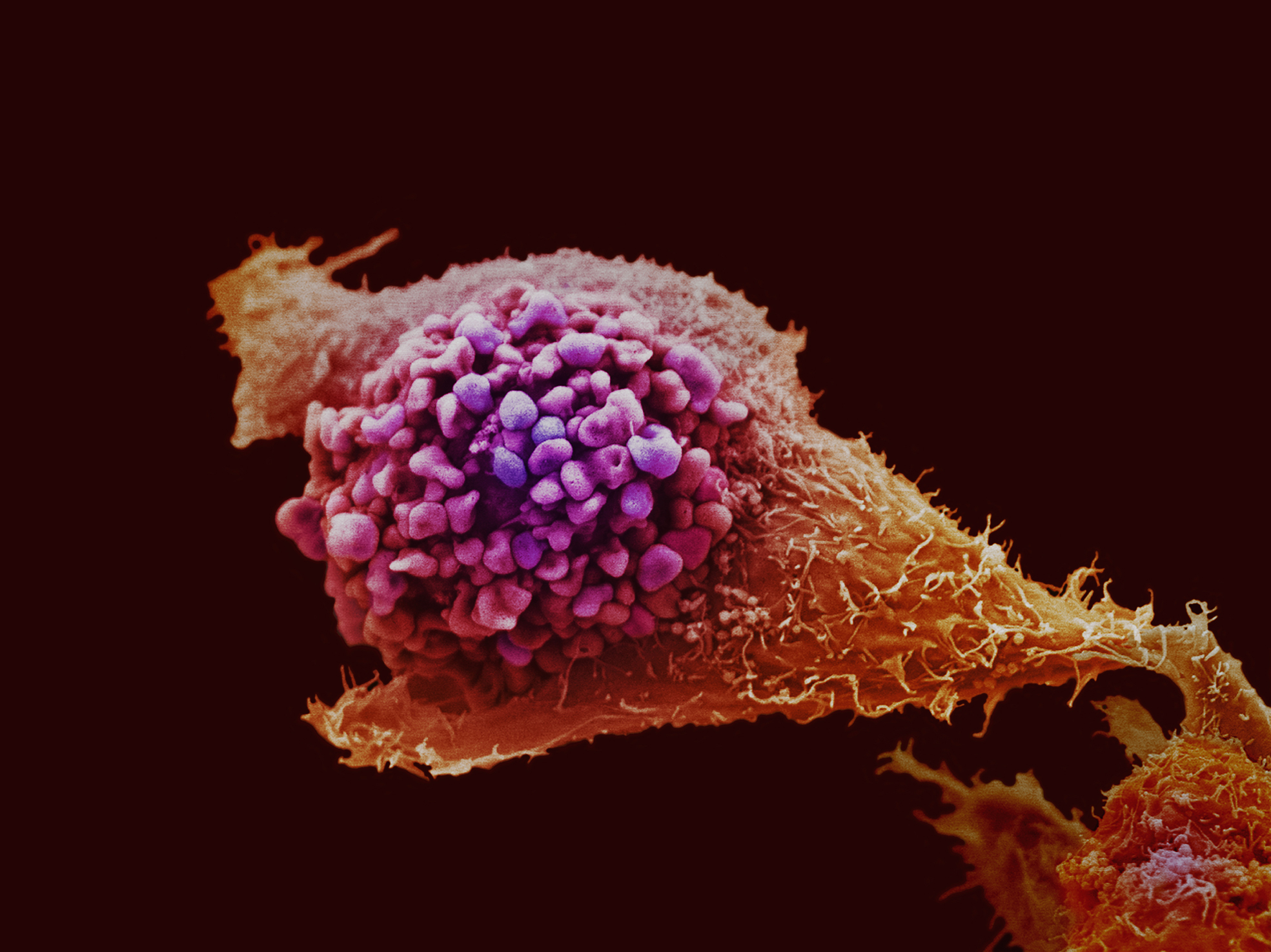
Kat - So you've got these molecules that are passing information on. You can see quite easily how that might go wrong in cancer. What sort of things do go wrong to the signalling?
Chris - Well frequently, what happens is that you get mutations in some of these relay components which turn them on all the time. They can't be turned off.
Kat - So you've always got this thing going, "keep going, keep going, and let's keep dividing."
Chris - You've only got an accelerator, and you haven't got a brake. Other types of genetic change, you just remove the brake. So it's like having a car that's parked on a hill and it's got no brake, so it goes to the bottom.
Kat - And also, you presented in your talk today some really nice data about cell movement as well and how faulty cell signalling might make cells go off on the move which is obviously very important when cancer spreads?
Chris - Yes, this is one of the most difficult things to understand in cancer. What is/are the mechanisms which make cells move from their normal place in the body and disseminate somewhere else? And it's that process, metastasis, which is actually the major clinical problem in cancer. And now, by having the methods to molecularly dissect the movement of tumour cells, we're beginning to identify targets of potential drug therapy to stop tumour cells moving.
Kat - Now presumably, this kind of signalling processes that makes cells grow, and make cells move, and make cells die is normally needed for normal health when we need to make new cells if we damage our cells. So, how can we target the processes that are faulty in cancer without switching off the signalling that we need to make new cells when we really need to?
Chris - Well this is a very interesting question and it turns out that many of the genes which are altered in cancer, their primary role is actually in embryonic development. So we're not so dependent on those genes and the proteins they encode for their signalling in adult life.
Kat - So this is when you're developing as a baby in the womb and then they get switched off when you're an adult, you don't need them.
Chris - Yes.
Kat - So then, you should be able to develop drugs that target them when they got switched back on in cancer.
Chris - That's true and the other thing which happens is that some of these proteins, because genetic mutations make them so active, you have a threshold, a window of opportunity where you can inhibit the cancer form, but you're not inhibiting so much, the normal form.
where you can inhibit the cancer form, but you're not inhibiting so much, the normal form.
Kat - So that's when the one that involved in cancer is particularly strange or it has a different shape or something like that.
Chris - Particularly, if it is mutated. If it's particularly active.
Kat - So, where have we got to with developing these kinds of drugs and testing them? Are things available in the clinic now or are things just coming through in the pipeline?
Chris - It's a bit of both. On the pathway which I've spent most of my time working is what we called the Ras Raf Mek Erk pathway.
Kat - Say that again?
Chris - Ras Raf Mek Erk.
Kat - Ras Raf Mek Erk. Lots of abbreviation too.
Chris - The two best targets for drug therapy in that pathway are Raf and Mek, and there's over 20 drugs now in early stage clinical trials that hit Raf and Mek, and one of them, a drug against the BRaf protein which is altered in about half of melanomas. That is now licensed for treatment of cancer patients.
Kat - Is this the drug vemurafenib.
Chris - That is vemurafenib.
Kat - Almost as hard to say as Ras Raf Mek Erk. So we're starting to see these drugs actually getting through trials and to the clinic. Because they're only going to work for a certain proportion of cancer patients, how can we tell who they'll work for?
Chris - We'll have to determine what sort of genetic mutations the patients have in their tumours before we treat them and this now is going to be quite an easy technology. It is not going to be difficult to do this at all.
Kat - You can imagine a situation where you'd take a sample of a patient's tumour, you might test it and see what's gone wrong in it, and then give them a drug or a combination of drugs. Is that how it might work?
Chris - Exactly how it might work. This is what we call personalised or stratified medicine. You get the drug depending on what your mutations are in the tumour. I think these treatments based on these sort of ideas are going to come on-stream very quickly over the next 5 to 10 years.
Kat - So an exciting vision of the future. That's Professor Chris Marshall from the Institute of Cancer Research in London.









Comments
Add a comment