Reprogramming leukaemia
Interview with
Leukaemias are cancers of the white blood cells that we rely upon to fight infection. One of the most common forms of childhood leukaemia is called ALL - acute lymphoblastic leukaemia. Normally, doctors treat the disease by giving drugs to destroy the stem cells 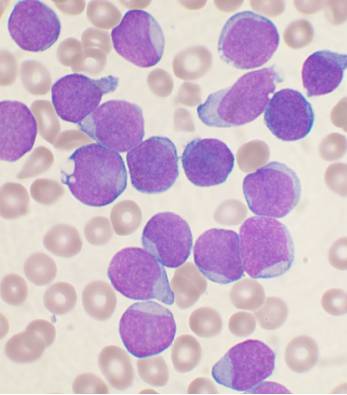 that are producing the leukaemia cells, and sometimes this is followed by a transplant with healthy bone marrow cells to restore the patient's immune system. But this is a complicated and risky procedure. Now scientists at Stanford University, in the US, have discovered that, by administering a certain cocktail of growth factors, they can trigger cultured leukaemia cells to switch from cancer cells into healthy immune cells called macrophages, as Ginny Smith heard from the study author, Ravi Majeti...
that are producing the leukaemia cells, and sometimes this is followed by a transplant with healthy bone marrow cells to restore the patient's immune system. But this is a complicated and risky procedure. Now scientists at Stanford University, in the US, have discovered that, by administering a certain cocktail of growth factors, they can trigger cultured leukaemia cells to switch from cancer cells into healthy immune cells called macrophages, as Ginny Smith heard from the study author, Ravi Majeti...
Ravi - When we took leukaemia cells, we were able to turn them into macrophages. Most importantly, those macrophages no longer caused leukaemia when we tested for that in the laboratory. It was a very surprising and unexpected finding because we didn't anticipate that the cells could change from one to the other.
Ginny - So, how have they done that?
Ravi - The details of that biology are things that we're still working out, but we were able to do that by using growth factors.
Ginny - So, these are chemicals that are found in the bone marrow normally, that affect normal development of cells.
Ravi - That's correct.
Ginny - And you were applying these to the leukaemia cells and managing to make them turn into something else.
Ravi - Exactly. We were trying to apply them to the leukaemia cells to see what would happen, essentially.
Ginny - Effectively, leukaemia cells are cells that have never grown up, that have kind of got stuck in childhood and you're now managing to make them grow up. But not just grow up and become the cells they would've become but actually, become a different type of cell. Why is it beneficial to have them turn into these macrophages? What do they do?
Ravi - Well, macrophages are important cells of the immune system. Their name actually comes from the Greek origin. So, the "macro" means big and the "phage" means eater. They're big eaters. They're very large cells. Their normal function is to ingest and digest bacteria or other foreign particles that shouldn't be in the body. But they also have a second function besides just eliminating things. The second function is then to simulate the T-cells and the other lymphoid cells to develop immune responses against those bacteria. So, not only do these macrophages not have the leukemic properties of cancer, but they may also be able to stimulate the immune system to fight the cancer directly.
Ginny - So, you would not only be getting rid of the cancer but perhaps giving the patient the means to fight back even better.
Ravi - Well, that's what we hope. It could be a two-pronged approach to fighting the cancer.
Ginny - Where are you in the sort of research stage? Are we looking at possible drugs in the near future?
Ravi - I would say that we are at the very preliminary stages of this type of investigation. This is the first record on this mechanism of turning cancer from one cell lineage into another and then potentially, stimulating the immune system to respond. We have only been able to accomplish these in the Petri dish in the laboratory. We're working now on two primary fronts. Number one is to try to identify drugs that might be able to cause this cell transition in an animal and then hopefully then in a human. But we're also working to try to develop methods in which we can make this transition happen, not just in the Petri dish but in an actual animal model.
Ginny - So, that's your next step to try and do this actually in an animal and cure it of leukaemia.
Ravi - That's exactly right. Now, we may use a variety of different methods including drug screening and other types of animal studies. But that's the real next step of translating this into a finding that it could have some impact on patients.
Ginny - Are there any risks with this type of therapy? Could you end up making their immune system overactive and perhaps giving an autoimmune disease?
Ravi - That is a very interesting question and I think it's a possibility because when you're trying to stimulate immune responses, you can both get responses against things that shouldn't be there as well as responses against the normal host. But we won't know that until we move into animal studies and that's definitely the type of safety in animal testing that will be necessary prior to thinking about any approaches to the patients.









Comments
Add a comment