Naked Engineering - Ultrasound
Interview with
Chris - Now, it's time to join Meera and Dave, and they've gone to a noisy car park to explore the engineering basis of ultrasound. Something of course, which is very useful in the diagnosis of, and screening for cancer.
Meera - This week on Naked Engineering, Dave and I are going to be looking into how ultrasound works. Now Dave, you do always take me to glamorous locations. We're lingering on the street, outside of a multi-storey car park. Now what has this got to do with ultrasound?
Dave - Well, to understand how ultrasound works, it's easy to start off with conventional sound. Sound is basically a vibration in the air which travels through the air. So when I'm talking here basically, I'm making the air vibrate in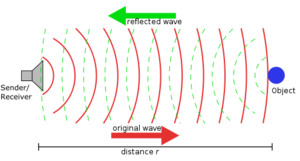 my throat, that's causing the air in front of it to vibrate, the air in front of that to vibrate, until it makes your ear vibrate, so you can hear me. Now, what's interesting and the reason why I brought you to this beautiful location is if I make a very loud noise, about 40 metres away, there's a great big wall. And so, if I make that loud noise, there's going to be large amounts of sound vibration going out to that wall. It's going to hit that wall. It can't carry on. All it can do is bounce back and we should get an echo.
my throat, that's causing the air in front of it to vibrate, the air in front of that to vibrate, until it makes your ear vibrate, so you can hear me. Now, what's interesting and the reason why I brought you to this beautiful location is if I make a very loud noise, about 40 metres away, there's a great big wall. And so, if I make that loud noise, there's going to be large amounts of sound vibration going out to that wall. It's going to hit that wall. It can't carry on. All it can do is bounce back and we should get an echo.
Meera - Okay, so we've got a lot of cars around us though, so I guess the noise you make is going to have to be quite loud.
Dave - Yeah, you're right. It could work with a clap. The problem is, my hands now hurt after clapping far too much and so, I'm going to try and make a very loud beepy noise.
Meera - Okay. Let's hear the echo then.
(Beep sound)
Meera - Yeah. I really heard that echo actually and it only took about half a second to come back.
Dave - Something like that, yes. Sound travels at 300 meters a second, so it's got to travel there and come back again, and so, probably half or a third of a second. If you get a bit closer, it should be a bit quicker. So, if you hear a whole series of echoes of a whole series of objects, you work out how far away they are by how long it takes the echo to get back.
Meera - Is this the principle used to try and image things or see where something is using sound?
Dave - That's right. If you know the direction the sound has gone out in and come back in, and how long it took, you know exactly where it is. So you can build up a 3-dimensional image. It's also how sonar works, so how you find submarines underwater.
Meera - Another form of sound that can be used for imaging is ultrasound and somebody that uses this for medical imaging is Graham Treece, based at the engineering department here at the University of Cambridge...
---
Graham - Ultrasound is a higher frequency than normal sound, so it's not stuff that you can actually hear with your ears, but it is still a vibration. It's just at a much higher frequency. High frequency sound actually travels into skin. It won't travel past bone, but it travels in soft tissue. So, using sound, you can see into anything which is soft tissue so that includes imaging babies in the womb. That's what most people have heard of, but includes imaging say, liver or kidneys or muscles, or anything which is soft tissue really.
Dave - I guess, normal sound would do the same thing, but it's got really long wavelengths, so you wouldn't be able to see any good detail.
Graham - You're quite right. The wavelength is much longer and that means that the resolution with which you can see is no good for actually looking at the detail inside people. Yes, that's right.
Meera - And so, you've got a setup here of an ultrasound machine. How does this all work together to provide an image?
Graham - Most ultrasound probes are a 1D array of little crystals, say, 200 odd crystals in a row. Those crystals, when you fire them with a little bit of electricity, vibrate and that vibration generates the ultrasound. The frequency with which you used the electricity to fire them generates a particular frequency of ultrasound.
Meera - You usually have to apply a gel onto the skin before actually using this probe. Why is that necessary to help image?
Graham - What you're seeing in the image is the amount of sound reflected back from tissue, and sound reflects when there's a big change. So for instance, if you clap or ping next to a wall, the sound reflects off the wall because the air is not very dense at all and the wall is very dense, so you get the sound reflecting back. It's the same in tissue. You're seeing reflections of, mainly, different densities in the tissue. Now the problem is, if you just hold a normal ultrasound probe in air, the air is not dense at all, so all the sound basically just reflects straight back without ever going into the body at all. So you have to have what's called a coupling gel - or in fact, water does a reasonably good job as well - between the probe and the tissue to remove all the air so that the sound actually gets into the tissue, rather than just coming straight back at soon as it hits air.
Dave - So the probe is producing a beam of sound into your body and it steers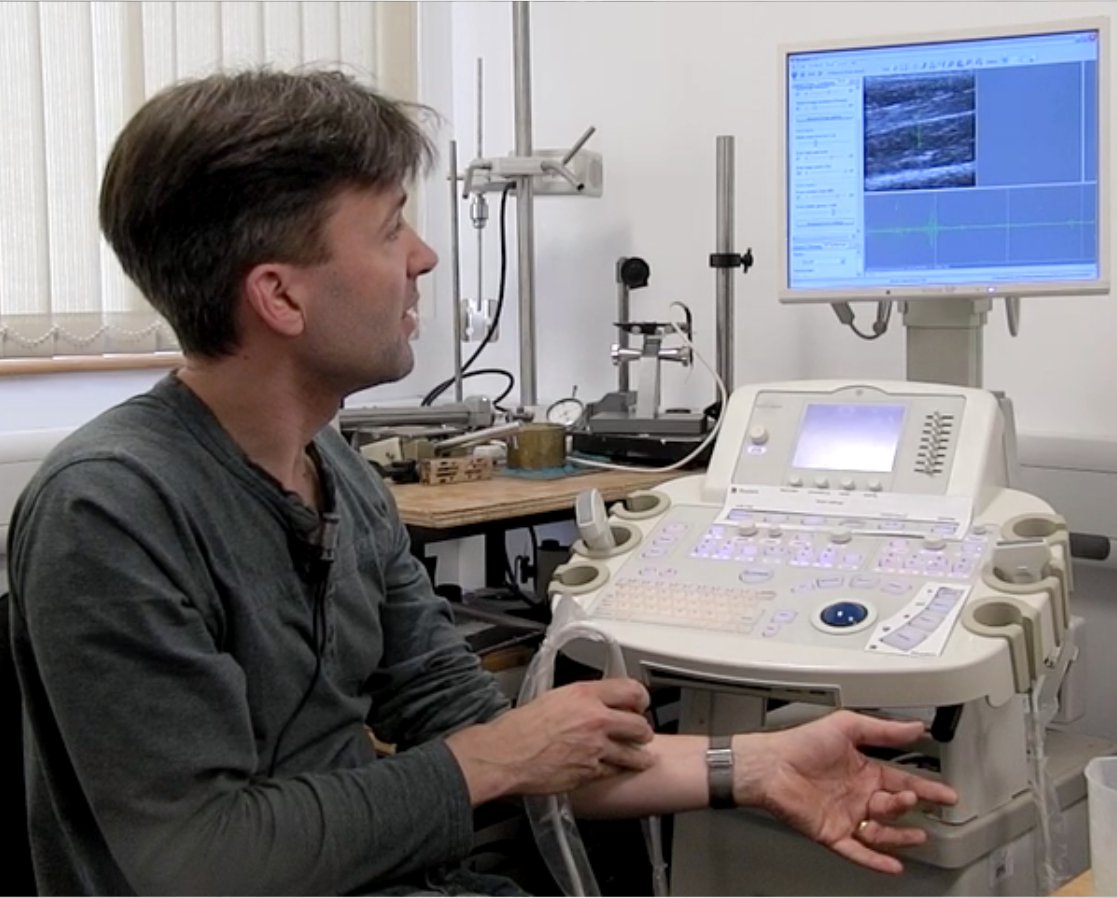 that around and listens for reflections coming back.
that around and listens for reflections coming back.
Graham - That's actually quite an important point. Yes, of course. If you only had one element producing sound, it will produce sound in all directions and you wouldn't know where the reflections were coming back from. And there's actually a little lens on the surface on the probe which focuses the sound in a plane. So effectively, you get a sort of thin beam of sound coming out.
Meera - Okay, well you do have some of the gel and also some water next to you. So could we perhaps see this in action? There's no chance of you being pregnant, so I guess you're just going to be putting it on your arm?
Graham - Yes, that's right. In fact, the probe I'm using is a higher frequency probe. You'd use a lower frequency probe for pregnant women because the lower frequencies see further into the body and higher frequencies don't see as far, but with better resolution.
Meera - Okay, so you've just dipped the probe into some water and it's now on your arm, just below your wrist, and an image has come up. It's actually quite clear. It's a grayscale image, but you can quite clearly see the muscles.
Graham - Yeah. You can see all the tendons and the muscles in the image. In fact, if I wiggle my fingers, you can see different bits of my muscles moving as they're wiggled. What's happening is that little pulses of sound are being sent into the tissue and then they're received back. The next element along in the transducer is then fired and that sends a pulse into the tissue and that's received back, and that's repeated lots of times, so you have 1 to 200 different echoes and responses. Now each of those is a vertical line in the image that you're seeing. And so, when you put them all together, you get what looks like essentially a 2D cross section through my muscles.
Meera - This explains just how the process works to allow us to see inside our bodies. But you're using ultrasound in a slightly different way in your research, Graham...
Graham - Normally, with ultrasound images, you see just the amount of sound that's being reflected back from tissue boundaries, and that's very good for looking at lots of things. But what we're looking at is using the same signal, so the same ultrasound, but to look at tissue stiffness. This is really interesting because there are quite a lot of physiological conditions where stiffer tissue means something. So for instance, if you have a lump or a bump, in a sense, we're trying to produce a way of imaging that lump, a bit like manual palpation. You know, clinicians prod a lot and what they're feeling for is essentially stiff bits under the surface. Well if you can image them instead, you can see how stiff they are and exactly what shape they are, and how deep they are, and you can get it with a much better resolution than just feeling with your fingers.
Dave - And I guess, if you're using an ultrasound probe, you can go a lot deeper than you can do with poking your fingers.
Graham - Yeah. In general, that's true. So, with this technique, you can see a stiff thing which is only say, a millimetre across, 4 or 5 centimetres deep and you probably wouldn't feel that if you prodded.
Meera - How does this actually work then? So why are you able to see differences in stiffness, and to what scale?
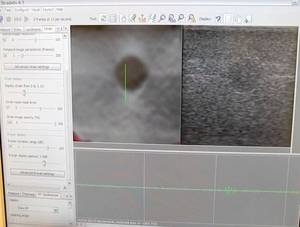 Graham - In normal ultrasound, what you actually see on the image is the amount of sound being reflected, as I've said. Now, we can use exactly the same signal, but what we do is acquire lots of ultrasound images and then we compare them, and by looking at the way that the tissue moves between each of these images, we can work out how it's deforming as you press slightly with the probe. And that can give us information about how stiff the tissue is. So, if you imagine a very stiff thing embedded in some very soft material, if you pushed it, what would happen is the soft material would squish together, and the stiff bit would just move without squishing, and that's what we're detecting. Essentially, we're measuring the deformation and then you take the gradient of that, which gives you something called strain, and we can relate that to the stiffness of the tissue.
Graham - In normal ultrasound, what you actually see on the image is the amount of sound being reflected, as I've said. Now, we can use exactly the same signal, but what we do is acquire lots of ultrasound images and then we compare them, and by looking at the way that the tissue moves between each of these images, we can work out how it's deforming as you press slightly with the probe. And that can give us information about how stiff the tissue is. So, if you imagine a very stiff thing embedded in some very soft material, if you pushed it, what would happen is the soft material would squish together, and the stiff bit would just move without squishing, and that's what we're detecting. Essentially, we're measuring the deformation and then you take the gradient of that, which gives you something called strain, and we can relate that to the stiffness of the tissue.
Meera - What makes it better or why is it beneficial to use this over current methods of looking for, or finding, tumours?
Graham - Well you're seeing something completely different. So, normal ultrasound is quite good at looking at soft tissue tumours, but it doesn't show you stiffness. So, there are already reasons to believe that this will improve either diagnosis of tumours, so we have a pilot study looking at breast tumours at the moment, or at least help to decide whether to go ahead and have a biopsy which is what normally happens if someone is suspected of having a tumour. So it may help, for instance, in reducing the number of biopsies that need to happen.
Meera - Okay, well I look forward to seeing these in our hospitals soon. Thank you very much, Graham and thank you, Dave. That's it for Naked Engineering this week.









Comments
Add a comment