Every year in the UK more than 330,000 people are diagnosed with cancer. The good news is that more and more are surviving, and there's hope that the new generation of genetic research and targeted therapies will bring more cures in the future. But is cancer a cleverer enemy than we thought? Plus sealion genital cancers, and an over-excited gene of the month.
In this episode
01:06 - Elaine Mardis - Cancer genetics
Elaine Mardis - Cancer genetics
with Elaine Mardis - Washington University
Kat - This month's I've been at the 10th annual National Cancer Research Institute, or NCRI Cancer Conference up in Liverpool, hearing from some of the brightest stars in the cancer research community. And, as might be expected, many of the talks touched on the faulty genes that drive cancer, and how we might target these to find new treatments.
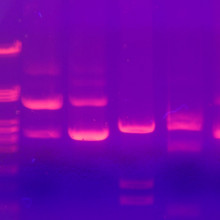
The advent of DNA reading, or sequencing, technology has changed our understanding of cancer, particularly over recent years. Today we know that at its heart, cancer is a disease driven by genetic faults in cells, and that these can be inherited in some cases, but mostly arise throughout our lifetime.
One of the keynote speakers at the NCRI Conference was Dr Elaine Mardis, co-director of the Genome Institute at Washington University in Missouri. She's one of the thousands of researchers working on understanding these gene faults, and how they can be targeted with new 'smart' drugs designed to attack specific faulty genes and molecules in cancer cells. I asked her how things have changed in recent years, and where this brave new genetic world is taking us.
Elaine - There's been an incredible transformation of cancer genetics and genomics over just the past short 5 years, and that's really been accelerated primarily by the advent of next generation sequencing. So, these are new sequencing technologies, as of about 2007, that allow us to nowadays generate the data for an entire human genome - be that a cancer genome or a normal genome or both - overnight. Of course, the analysis of that data is much longer than overnight. But really, I think it has set the stage over the past 5 years for really teasing out the genetic underpinnings of cancer. What is it about the cancer genome that that's much different than the normal genome in an individual? And then expand that question by tens of thousands of individuals to really begin to understand across the board the similarities and differences in cancers. This really now, I think from the discovery phase of the last 5 years or so, is setting the stage for what we call 'clinical translation' of the cancer genome. So, how do we start as genomics folk to use what we've learned, to add to the diagnostic information that each doctor who's in the cancer cure sphere uses to help better treat each individual patient.
Kat - Kind of lifting the bonnet on cancer now and seeing its workings, its genetic innards if you like. What have some of these experiments told us about what is going on under the hood of cancer?
Elaine - Right. The basic discovery phase that we and others across the world have been in for these past five years has really revealed a lot, a lot that I think we didn't expect. So, what are some examples? So, I think one of the things that we traditionally have thought about cancer is that it has a lot of disease site specificity. So, you'll see oncology specialists often divided into breast cancer, brain cancer, lung cancer. And that's still the case, but what genetics and genomics has told us is that all those kinds of cancers and others share many of the same genetic alterations, whether it's in the cancer cells themselves or genetic alterations that are inherited or occur spontaneously. So, that I think has been probably the biggest eye-opener, is that there's a lot more shared drivers of cancer development, if you will, at the level of the genome.
I think the other surprise in all of this is that the more you ask, the more you find out. And we've really as a result of that broader look, expanded our understanding of the functions of proteins that are mutated in cancer cells. So, by studying the genes, we can extrapolate forward, if you will, to the impact of many of those mutations on the resulting protein. That's really what plays out in the tumour cell and does all the work. In that regard, some of the proteins that are now emerging that look like they are also causing cancer to develop are proteins that for example, add methylation or take methylation away from DNA.
Kat - These are the marks that tells cells what to do with their genes.
Elaine - Yeah. They sort of tells which genes are on ,if you will, and are going to be turned into proteins and which ones are turned off. Also, the proteins that organise the structure of DNA within cells are now being found to be frequently mutated. We don't fully understand what that means in terms of the driving of cancer, but that's an area of active investigation. I think this is a very exciting area that again was completely unanticipated by previous focused studies of the cancer genome. So, all of these are kind of exciting to scientists as well as patients, as well as pharmaceutical companies. Let's face it, because it really opens up a new area where we might be able to develop very effective and very targeted drugs against cancers.
Kat - So, we found all these things that are faulty in cancer cells, maybe things we didn't expect, but obviously, what patients want to know is, how is this going to benefit me and if not now, then when? So, how are we turning some of this genetic knowledge into actual treatments of patient benefits?
Elaine - Right. So, patients I think ultimately and even today are benefiting from the added information that genomics provides. So, I talked earlier about how we were surprised that some genes that we thought were unique to certain cancer types are actually mutated in multiple cancer types, often unexpectedly. What this means is that if that mutation is identified in your cancer, there may well be a targeted therapy that helps to address that cancer. It could be added into the conventional chemotherapy regimen, you could qualify to be on a clinical trial and now clinical trials are considering a subset of patients that may be outside of these expected tumour types that can also get access to that drug if they have that mutation.
So, I think this is, even right now today, a realised and realisable benefit for patients. We don't want to suggest that genomics means that we need to leave all the conventional assays or investigations of cancers aside. But just that it adds some additional information for the oncologist who is considering how best to treat the individual patient. Ultimately, I suppose in the fullness of time, what we hope is that certainly, this added information will affect a larger number of patients who are alleviated from their tumour burden, as we learn better about how these therapies work, when they don't work, and so on and so forth. So, it's early days, but there are some immediate benefits that are being seen by patients.
Kat - That was Elaine Mardis, from Washington University in Missouri.
08:42 - Bill Sellers - Targeting cancer
Bill Sellers - Targeting cancer
with Bill Sellers, Novartis
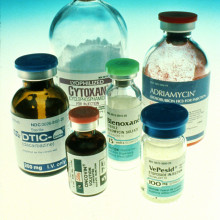
Kat - As we just heard from Elaine, DNA sequencing technology is enabling us to uncover the genetic faults driving an individual person's cancer, and target them with specific drugs. Many of these drugs are showing impressive effects in clinical trials, and some have been licensed for use for patients on a wider scale. But all too often - after months or even years - the cancer comes back, because the cancer cells have evolved resistance to the therapy.
Bill Sellers, lead for oncology drug discovery at the company Novartis believes - like many in the field of cancer research - that the way to overcome this resistance is to use combinations of drugs. I spoke to him after his lecture at the NCRI Cancer Conference, to discover more about these targeted therapies, and the best way to mix and match them to bring forward meaningful cures.
Bill - The paradigm that began with Gleevec, which is a drug that treats a disease known as chronic myelogenous leukaemia or CML. The discovery there of a chromosomal abnormality or genetic alteration that activated a gene in that disease happened several decades ago and that eventually led to the discovery of a drug that could turn off that gene. That gene is called Abl, the genetic alteration turns Abl on, you get cancer. The drug turns it off. You give that drug to people, the cancer goes into remission and people have really been now sort of experiencing normal life expectancies on Gleevec.
Kat - That sounds fantastic that from treating this disease, we have a drug that has really saved many thousands of people's lives around the world. Why can't we do this for all other cancers?
Bill - Yes, that's a great question. This disease I described - CML - turns out to be less complicated than your more common tumours like lung cancer or breast cancer or colon cancer. In those instances, the genes in those cancers are more disregulated or more mutant than in the first disease, chronic myelogenous leukaemia. So, resistance to the drugs can happen much, much faster. So, that's one of the big problems. And then the second is, we still don't know all the genes we need to turn on or off in these other cancer types.
Kat - So, we've seen in recent years a new breed of targeted therapy starting to come into the clinic. We may refer to them as smart drugs or drugs that are designed, like Gleevec, to target a specific genetic or molecular fault in a tumour. Where are we with these drugs and what are the problems with some of them?
Bill - So for example in lung cancer, there's a drug that treats a gene known as the EGFR gene or EGFR mutation. There's another couple of drugs that treat a form of lung cancer that has a gene called ALK. In each case, those drugs work, but they only work for a limited period of time and then patients relapse. And patients relapse because they develop new mutations that create resistance to the first drug.
Kat - This is the idea of cancers almost evolving to get away from the therapy.
Bill - Yeah, it clearly evolves and we see that evolution in real time. So, the key there now is to try to find second or third drugs that also pin the cancer down to a point where they can't escape through a simple evolutionary path, and make the evolution to a resistant state basically impossible for the cancer.
Kat - So, tell me a little bit about what you're trying to do in tackling resistance to this drug, Gleevec, or drugs that work in a similar way to it?
Bill - The first is that, we believe we now have better and better tools to study resistance in the laboratory and really predict resistance mechanisms that will be seen in humans. In the past, with chemotherapy, attempts to study chemotherapy resistance in the lab really never yielded anything that was of much benefit in humans. But now, especially in the case of Gleevec, we've seen we can really model experimentally the resistance in the lab and it will replicate in the human. So, that gives us the ability now to say, "Well, how can we, in the lab prevent that from happening?" So, we're using various large scale genomic methods to tackle that problem in the lab and then study patient samples to see if those mechanisms are taking place in the patients.
Kat - One of the ways I like to think about almost is, it's like a river and you dam it in one place with a treatment and it finds a way to get around. But if we can work out how to dam the path that it would take, is that the kind of approach you're talking about, finding two, maybe even three drugs that will just stop it in its tracks?
Bill - Yeah, that's exactly the idea. Some people have drawn an analogy to the treatment of AIDS where the virus was evolving, and it wasn't until they had three drug regimens that they had a regimen that stopped the viral evolution. Now, AIDS patients are very well treated with the combination approach. So, we also know in tumours that we have been successfully treating diseases like lymphoma, usually, you need more than one drug, often, two or three drug regimens are required. So, we think in these cases that we were talking about earlier, EGFR in lung cancer, we need to go beyond the single drug treatments and find the two or three that are going to - as you said, completely block the river.
Kat - We know that the drugs we have, have extended life as you say and that the idea of the 'magic bullet' cure for cancer is probably fictional. But do you hope maybe even in your lifetime that there'll be some cancers that with the right combination of drugs, we can cure?
Bill - I'm sure of that. I don't have any doubt about that. First, because of the sort of things I've been talking about. But if you look over the last year, there's been progress on more than one front against cancer. So, there's the part I talked about which was drug discovery against the genetics of cancer. But then there's immunotherapy, which really has been validated over the last year or so as having a significant therapeutic benefit. And then there's things like antibody drug conjugates and just biologics in general. All of these now are validated ways of having significant therapeutic effect. Yet, none of those have begun to be really put in combination yet. So, I think with that kind of sort of weaponry based against cancer, I think - I have a lot of hope that we're going to make huge progress over the next 5 or so years.
Kat - That was Bill Sellers from the company Novartis.
Kat - That was Bill Sellers from the company Novartis.

15:13 - John Hammond - Sea lion cancers
John Hammond - Sea lion cancers
with John Hammond - Pirbright Institute
Kat - In the 1980s, Frances Gulland and her team at the Marine Mammal Center in Sausalito on the California coast noticed an increasing number of wild sealions getting stranded or washing up dead on the beaches with urogenital cancers. In fact, these cancers are a major cause of death in the sealion population. Because it's unusual for wild animals to be affected by cancer to this extent, Dr John Hammond at the BBSRC Pirbright Institute in Surrey wanted to find out more about what might be causing them, and if there was a genetic link.
John - Several people before I was involved in this have found that it's quite a complex cancer in that, like a lot of cancers, there are a lot of factors that are going to causing this cancer in an individual. So, it's not an obvious association with one particular gene or one particular environmental variable. A colleague of mine, she was doing some population genetics with the California sealions and she was looking at inbreeding in the populations around California and the west coast of the states and if there's any association with infectious diseases. What she found is there's one particular microsatellite locus that seems to be associated with this cancer.
Kat - So this means, the animals that have this type of cancer, they have this particular genetic variation in their DNA.
John - Or a significant number did. So, these microsatellites are hypervariable regions. They're not necessarily functional. They're just markers in an animal's genome. They've been used over many years now in many, many different species to look at the population structures because these are regions that differ subtly between individuals within a population.
Kat - How did you home in on a gene that might be involved in these cancers?
John - We took that region and Elsa Hall and her colleagues at the Sea Mammal Research Centre, they did a very neat case control study involving quite an impressive number of animals, considering that this is a wildlife species. They found that there was a significant association of homozygosity at this one microsatellite marker and prevalence of the carcinoma.
Kat - That means that this marker is on both of the chromosomes - the one they've got from mum and the one they've got from dad.
John - Yes, so if both copies of your genome have the same microsatellite sequence then there was an association that you were more likely to get cancer than if you had two different versions of this microsatellite. So, it's just used as a marker.
Kat - So homing in then, what do we know about what might be going on then at a genetic level that's causing these animals to become sick?
John - There is no genome for a sealion as yet and so, the nearest genome that we had was, or we still have is the dog, which separated from the sea or sealion lineage about 45 million years ago. So quite a while, but nevertheless, they're still carnivores. They're all carnivores. We sequence this very short region and I was able to use some comparative genomic work and find a region of the extended microsatellite sequence that had significant identity within the dog genome.
Kat - So, it's basically a match between the region in sealions and the region in dogs.
John - Yes. Once I had a region in the dog genome, I was able to then extend the region that we assumed that the microsatellite was in in the sealion, get some more sequence data from the dog and then go in and look in more detail at the sealion. So, when we compared it with other mammalian species we found that its region of the genome is conserved across mammals.
Kat - So, what's lurking in there? Have you got any good suspects?
John - So, the region is actually within a gene called Heparanase 2. Heparanase 2 is actually quite an understudied gene, but it has been implicated in many cancers particularly in humans. It's obviously a very neat association that we find that a microsatellite associated with carcinoma in sealions happens to lie within what would be considered a good candidate gene to be involved in that process. We haven't established a direct link but it is intriguing.
Kat - So, what next for this? I mean obviously, it's very sad for the sealions that they're being affected by this cancer. But how is this information going to potentially help them in the future?
John - Clearly, a lot of animals are suffering from this disease and at some point, it is untreatable and the animals has to be euthanized. As I said earlier, it's actually a very complex cancer. So, it's not just the genetics that are involved in being more susceptible or less susceptible to this cancer. There are lots of other things that have been implicated including environmental contaminants, which I think are important, potentially some other genetic markers and also herpes viral infection. So, when it comes to helping the sealions, if we can begin to establish how these factors interplay with each other, we might be able to reduce the prevalence of this cancer. And also, it will help in the treatment of the animals if we can understand from their genotype, how likely they are to develop cancer or recover from cancer, or be treatable, then that also helps in the management of the population.
Kat - That was John Hammond, from the Pirbright Institute. And his research was published in the Proceedings of the Royal Society B journal last month - the reference is on our website, that's Nakedscientists.com/genetics

20:54 - Breast cancer - Hope or reality?
Breast cancer - Hope or reality?
with David Miles, Mount Vernon Hospital; David Cameron, Edinburgh University
Kat - At a somewhat gladatorial debate hosted by the charity Breakthrough Breast Cancer on the first night of the NCRI Cancer Conference, researchers debated whether treating metastatic breast cancer - that's breast cancer that has spread through the body - with genetically targeted therapies is hype or reality. To get a flavour of the discussion, I talked to two of the expert speakers - Dr David Miles from Mount Vernon Cancer Centre, and first, Professor David Cameron (no relation to the one at Number 10) from the University of Edinburgh.
David C. - I think one of the key points is, it's not just the future. It is also happening today and the biggest and best example is, when we use treatments to target to the HER2 oncogene. But this is gene which are multiple copies in some breast cancers that alters the behaviour of the cancer and allows us to target it therapeutically.
Kat - And that's with the drug Herceptin that people have heard of.
David C. - So, this is something that we can already use to treat some of our breast cancer patients.
Kat - And this is all stuff that's come from our understanding of the genetic faults, the molecular nuts and bolts of what's gone wrong in cancer cells.
David C. - Exactly. Now it's true, we haven't got a map that allows us to target every single observed or measured genetic change, but the reality is, we're able to do it for some people now. By mapping that in more detail, I believe that there'll be more patients inn whom this will become a reality.
Kat - And you David, you're a little bit more sceptical about this being the way forwards. Tell me where you're coming from.
David M. - Like many developments in their infancy, this is being somewhat overhyped. So, there is the suggestion that by understanding the alterations in the genome, that that will necessarily result in treatments that can target those alterations. Now, in some tumours, that may be true. In breast cancer, we're still struggling to understand what the driver mutations are. Now, the HIR2 alteration in breast cancers, that was not really discovered through changes in genomics. That was through understanding signal transduction. Now of course, it does eventually go back to genomics, but that advance in treatment of patients with that sort of breast cancer wasn't made through genomics.
So, I think my argument is that just because you can take a picture of a very, very complex situation does not automatically mean that you're going to have useable treatments. Such is the complexity of the biology that just squeezing one particular pathway, you're going to have compensatory mechanisms many, many times, meaning that that therapy is very rapidly overcome and bypassed. So, I think it is very much work in progress. Now, I'm not convinced in breast cancer metastatic disease at least that it is actually reality now in those terms of using the genome to develop targetable lesions.
Kat - One of the things that we've heard a lot about lately is this concept of tumour heterogeneity - not all the cells in a cancer being the same- and also, tumours evolving within the body, becoming resistant to treatments, as you say. Is this as you see it, the biggest block to using this kind of targeted treatments?
David M. - Yeah. I mean, in my arguments with David here, I was sort of trying to use that Darwinian principle that says, "If put pressures on an organism or a cancer cell from one side or another, it will develop changes and adapt to overcome those particular pressures" and I think that's what the challenge is going to be. So, cancer is extremely smart and we are relatively dumb.
Kat - David Cameron, cancer is smart and we are dumb. How do we go forward from here?
David C. - I hate to agree with an opponent in the debate but I think you make a very valid point. We've been rather dumb about this. I think there's been a very naïve expectation that by spotting a few mutations we will suddenly have a few wonder drugs. The argument here I think is that we need to be clever and think in a more complex way and realise that what drives a cancer's behaviour are the genetic changes. And they're very good at acquiring new ones. Have we sat and worked out which are the key drivers that allow that mutational picture to appear? If we simply pick off a few mutations because we happen to be able to and that some of the hype has been expected from outside, that's probably where we go wrong.
But that hard reality is, that's what's happening in the cancers in the patients. It is a genomic mess and I think we've been simplistic in how we've approached. We need to be smarter. We will never be as smart as a cancer, but if we could understand better the complexity of that genome picture - the challenge of drugging what's called the undruggable, and some of these may look in our current science as undruggable, we've cracked it before and I'm sure we'll crack some of them again.
David M. - It is comparatively easy to look at the genome level. It is much, much more difficult to look at the protein level. I think we have to look at all aspects of expression really to understand the pathways. So, we have to look at all aspects of how the cancer cell behaves.
Kat - There's lots of researchers around the world that are doing things like the International Cancer Genome Consortium, sequencing the DNA and mutations of lots and lots of tumours. So, do we just have to wait until our technology catches up to look in this greater detail?
David M. - I think it's not so much the technology. I think what is clear is that ascertaining the genome is becoming very, very straightforward. I think the informatics that is the biggest, biggest challenge.
David C. - And mixing that as you said with more than just a straight genetic mutational picture. How do we do that? We can't ignore any one of them.
Kat - To sort of wrap up, one point that was raised was that a hundred years ago, we would've looked at breast cancer patients today and said, "We can hardly cure any of them" and today, women with breast cancer will survive for several decades. Do you think maybe painting a picture, 50 years in the future that this will be a debate that - we have this debate now but actually, then we discovered that we could cure these women, thanks to genomic medicine. What's your hope?
David C. - I think we will cure more of them. It will be lovely to predict that we'll cure them all, but the reality is, I think at the moment, cancer is telling us, well, you're chipping away at me, but ultimately sadly, they'll still win for some patients. But yes, I believe with genomics and working in a multivariable way with the other -omics, we will cure more of them.
Kat - David Miles.
David M. - I think it will have a place ultimately. I think the point we were trying to make this evening is the fact that a patient coming in through the clinic today has an expectation that somehow, by understanding the changes at that DNA level means I can make a difference to their treatment today. Sadly, we are not there. We may be there in some years' time but it's going to be a long haul.
Kat - That was David Miles from Mount Vernon Cancer Centre and also you heard David Cameron from Edinburgh University, discussing whether genomic medicine for breast cancer is hype or reality, after their Breakthrough Breast Cancer-sponsored debate at the NCRI Cancer Conference.

27:53 - Gene of the Month - BRAF
Gene of the Month - BRAF
with Kat Arney
And finally it's time for our gene of the month, and this time it's BRAF (B-Raf). Although it may not have an amusing name, like many of the genes we cover, it's been very important for underpinning new approaches for treating certain types of melanoma skin cancer, as well as other cancers too. In 2002, scientists at The Institute of Cancer Research, as part of an international team, figured out that a faulty version of BRAF was found in the majority of tumour samples from patients with melanoma.
But rather than knocking out the function of BRAF, which normally sends signals telling cells to divide only when they're needed, the faults made BRAF become overactive, driving cells to divide out of control and form a cancer. After just 10 years, a drug blocking overactive BRAF, called vemurafenib or Zelboraf, was licensed for use on the NHS for treating people whose skin cancer had the faulty gene.
But although many patients have experienced impressive results, unfortunately their cancers evolve resistance to the drug and come back with a vengeance. Researchers are now working hard to understand how this resistance develops, and how to deliver the right combination of drugs to stop the disease in its tracks.
- Previous Why aren't there any flying spiders?
- Next Shift Work Shafts Brains









Comments
Add a comment