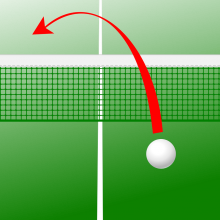
Repairing damage in the nervous system is incredibly challenging, but our guests this week have some promising solutions. Consultant ophthalmologist Dr Robert MacLaren from Moorfields Eye Hospital and colleagues at University College London have discovered a way to encourage the growth of photoreceptors in the retinas of blind mice, and Professor Geoff Raisman from University College London will discuss his research into spinal cord repair. In Kitchen Science, Derek Thorne and Hugh Hunt take a closer look at the aerodynamics of a ping pong ball.
In this episode
The Nano Piano
Could nano-music be on the way? Probably not, but scientists at Delft University in the Netherlands have successfully made and tuned the world's smallest piano wire. The wire is made of tiny carbon nanotubes, just 2 nanometers in diameter and one micrometer long. That's just two millionths of a millimetre by a thousandth of a millimetre. The team attached the wires to electrodes and placed on a layer of silicon. They then passed an electrical current through the silicon, which makes the nanowires vibrate. By changing the current, the team could effectively "tune" the wire, like tightening a piano or guitar string to tune it. Sadly, the team aren't planning to build the world's tiniest violin, or make a very baby grand piano. The tuning technology could be used for nanosensors, to weigh tiny particles like viruses based on the way they affect the vibrations.
X-ray-ted Molecular Movies
Scientists have found a way to see molecules in motion, providing us with new insights into the way complex chemistry takes place. Zurich University's Peter Hamm and his team have used a technique called infra-red spectroscopy to track the movements of individual chemical groups in a larger molecule. The discovery is important because until now we've only been able to gain individual snapshots of what molecules look like, frozen in time, by shining x-rays through solid crystals of them. But the atoms in molecules are more like beads connected to each other by springs, and they bounce about continuously. Indeed it's these movements that enable nature's catalysts, called enzymes, to do the jobs they do, powering our metabolism. In the new technique the researchers glued down one end of a molecule and then shone infrared light at it from two directions. Because the bonds linking different chemical groups absorb infrared energy in a highly specific way it's possible to track, incredibly quickly, how these groups are moving around. At the moment the team have only worked with very simple molecules but it should be possible to scale up the process to tackle much bigger beasts. "We can use chemical isotopes placed at very specific positions in a molecule to shift the infra-red signal by a known degree and this will enable us to study more complex structures", Peter Hamm suggests.
Bling Helps To Detect Cocaine
This week we've been hearing about the radioactive Polonium poisoning that killed Russian Alexander Litvinenko. Although that's extremely rare, doctors are often faced with patients that have been poisoned with more common substances, or have taken drugs overdoses. For treatment to be effective, it's very important to know as quickly as possible what they have taken. But sometimes this can take long and complex lab tests, using up vital time. Now a team of scientists at the University of Illinois in the States have developed a testing technology that's simple and fast. You simply dunk a test strip in a sample of saliva, urine or blood plasma. The secret behind the strips is "bling" technology. They rely on gold particles and tiny pieces of DNA called aptamers, designed to stick very specifically to the target poison. In the test strip, the DNA aptamers hold together tiny particles of gold. But when the stick is dipped into a samples containing the poison or drug, the aptamers bind to it very tightly instead, releasing the gold particles. Thanks to some clever biochemistry, the gold particles then travel up the strip and are trapped, forming a distinct red band. So far, the team have developed a test to detect cocaine, and the strips seem to be as effective as lab tests. The lead researcher Li Yu hopes that they will be able to use their method to detect a wide rang of drugs or poisons, because it is easy to screen large numbers of different DNA aptamers to find the ones that stick to specific targets. The technology could also be used to detect biological molecules in blood, saliva or urine for diagnostic tests in hospitals, or for monitoring toxins in the environment.
Bug Helps Chemo Home in on Cancer
Scientists have found a bacterium that can help target anti-cancer drugs to the heart of a tumour, reducing the damage done to healthy tissues and minimising side effects. Writing in this weeks edition of the journal Science, Bert Vogelstein and his team, from the US Howard Hughes medical Institute, describe how a relative of the bacterium that causes tetanus, called Clostridium novyi-NT (C. novyi-NT), can selectively release chemotherapy drugs inside cancers. The researchers used mice with a form of colon cancer. The animals were first injected with spores from the C. novyi-NT bugs, followed by a dose of the chemotherapy chemical doxorubicin which had been packaged into tiny fatty droplets called liposomes. This provoked complete tumour regression in 100% of the mice, and 65% of them were still alive 90 days later. By comparison, none of the animals left untreated, or animals given just the chemotherapy agent or the bacteria alone survived for more than 40 days. The team found that the C. novyi-NT bacteria, which are anaerobes (they cannot grow in oxygen), first homed in on the oxygen-poor centre of an animal's tumour. There the bugs released a fat-digesting factor, called liposomase, which broke-open the packages of the chemotherapy chemical once it was administered, producing very high levels of the cancer-killing drug just within the tumour. The researchers have now pinpointed the gene used by C. novyi-NT to make the liposomase, which means it will be possible to produce the agent artificially and use it to better target chemotherapy to cancers, allowing doctors to use lower doses and therefore cut down side-effects.

- Repairing The Retina
Repairing The Retina
with Dr Robert MacLaren, University of Oxford and Moorfields Eye Hospital
Chris - Thanks for joining us on the Naked Scientists. So tell us what it is you've managed to achieve.
Robert - Well thank you very much indeed for inviting me onto your programme. What we showed was that, if you transplant photo receptor cells, which are the cells you mentioned earlier in the programme the light sensitive cells at the back of the eye, if you transplant these cells at a certain critical stage during development, it's possible that these cells can make connections in a new host after transplantation. And in sufficient numbers to restore certain visual reflexes, such as the light pupil restriction reflex.
Chris - So what's the major problem with the eye just repairing itself anyway? Why doesn't it repair in the same way that other tissues in the body can?
Robert - Well the retina is a nervous tissue, pretty much like any other nervous tissue in the brain or the spinal cord. So we are faced really with the same problems that spinal cord surgeons would have in that, once there has been a significant injury to the nerves, it's very unlikely that they will make connections and recover function. Some diseases that I deal with on a routine basis, for instance, age related macular degeneration which is the commonest cause of blindness in the UK, that particular disease becomes irreversible, once the light sensitive cells, the photoreceptors, are lost. And these photoreceptors are neurons and as such they don't regenerate or re-establish their connections as we would see with other parts of the brain.
Chris - So your strategy to get around that problem is to replace the cells that have been lost?
Robert - Absolutely. And we're of course very excited by it because our research is very much geared towards eye disease. We're interesting in treating diseases that affect photoreceptors because there are simply so many of them. Not just macular degeneration but inherited retinal diseases such as retinitis pigmentosa. These diseases have a big impact on patients how suffer loss of vision as a result of photoreceptor loss, and we're very excited at the prospect of actually... sometime in the future I must stress that these experiments that we have been doing are not yet at the clinical stage, it's all very much in the laboratory but we're very excited at the prospect of actually being able to transplant these cells and certainly now I think we know a little bit more about the properties of the cells, and what we need to do to actually achieve our goal of doing this in patients.
Chris - People have tried using various stem cells to do what you've done in the past but they didn't succeed. So why did they stumble when you managed to succeed?
Robert - Well that's a very interesting point. I must say, stem cells can be used successfully in other ways, but we're interested in generating a specific cell type, the photoreceptor, which as I said is a neuronal cell type. If you take a very undifferentiated stem cell, simply a dividing cell that has yet to decide what kind of cell it's going to become, and you put that into the retina, those dividing stem cells won't necessarily know they should become a photoreceptor or indeed any one of the perhaps 220 different adult cell types in the human body. And our approach which was somewhat different was to take cells that were about to become photoreceptors, in other words the signals within the dividing cells had already been switched on, the genes had been activated, and transplant them at that specific, critical time point. If you like we're transplanting immature photoreceptors that have already passed the point of no return, they're going to become photoreceptors. And that allowed us to focus more on the properties of these cells actually making connections.
Chris - Now you did this using mice, obviously, because you mentioned you haven't got this into the clinical trial stage yet, but does this mean that you're going to be able to do this in humans? Because there aren't, obviously, going to be the potential opportunities to go to humans that are in very early stages of development and take photoreceptor cells from them. So how would you get round that problem?
Robert - Well that's absolutely right, and of course our work has been looking at the practicalities of the transplantation. But if you think about it, I mean there are a number of adult stem cells in the human body, not just embryonic stem cells, everyone thinks about stem cells as being an embryonic stem cell, but there are many cells around the body that are dividing, and all of those cells have identical DNA. What makes one cell a photoreceptor and another cell a skin cell or a liver cell, is the genes that are switched on within those cells. And if scientists who are working in cloning and genetics can find ways of manipulating the genes that are switched on, then it is not inconceivable that one could generate a primate photoreceptor from an adult stem cell. Indeed there have even been reports of retinal stem cells, these are stem cells actually in the eye, that are dividing to make ocular tissues. Really, one can not make the assumption that it's going to be embryonic because there is a lot of research going on at the moment looking at adult stem cells which is a very, very exciting area.
Chris - I suppose one of the really interesting things was that all of the signals are there in the eye so that the cells when you put them in, a) know where to go, b) know what to turn into and c) how to wire themselves up into the retina so that they can restore the ability to see in the animals you tested.
Robert - Yes, I mean we are very fortunate in a way working with the photoreceptor. Because, of all the neurons in the body, the photoreceptor in one way is quite simple, in that it only makes a connection in one direction, because it's stimulated by light. A lot of neurons need to be connected in two directions, both upstream neurons and downstream, via the axon. In the case of the photoreceptor we really only need to make one connection. The distance for the connection is also very short. Within the retina there are very few inhibitory proteins that would inhibit the growth of an axon. And I think one of the other things is that, the actual photoreceptors sit in a natural anatomical cleavage plane, a natural space, where it's relatively easy to introduce these sort of cells without damaging any of the surrounding tissues. We even know from the studies during development that the pigmented part of the retina which is called the pigmented epithelium has a major role in helping the photoreceptors to orientate and develop and make connections. And it certainly seems to be that the retinal pigment epithelium in the host retina, if we put the cells in at the right place at the right time, are able to actually help these new cells make fresh connections.
Chris - Now you can't ask a mouse whether it can see, you certainly can't ask it to read a chart that you would be showing it at the ophthalmologists, or in the opticians to test your vision. How do you know that these mice are able to see again once you've done this?
Robert - That's quite right. We were very interested to know what the level of vision was, and most importantly we wanted to test the level of visual function that actually told us whether the brain was responding to the visual signals. So as well as the fairly routine physiological tests, we also looked at another test, which is the ability for the pupil to constrict. And we took congenitally blind mice that have a deficiency of the rod photoreceptors, again, the cells that you mentioned earlier. These are the cells used for night vision, and for mice, being nocturnal animals, they depend heavily on these cells. We transplanted photoreceptors into the retinas of these mice, and we were able to restore the light pupil restriction reflex. So essentially, if you shined a light into the eye, the pupil constricts which is the normal thing that happens. And we were able to restore that reflex with the transplanted cells. And that really was proof, not just that the cells were in the retina and receiving signals, but that the brain is interpreting those signals, and signals are then being sent back into the eye, to cause the pupil to constrict. And I think that's pretty much as close as you can get with a mouse.

- Repairing Damaged Spinal Cords
Repairing Damaged Spinal Cords
with Professor Geoff Raisman, University College London
Chris - We've looked at the eye, you're working at the other end of the body, on the spinal cord. Why is it such a problem when the spinal cord gets injured, why doesn't it just repair itself?
Geoff - Well there's a number of opinions about that, and the answer is we don't know. But the idea that we have is that the spinal cord attempts to repair itself, but the damaged nerve fibres are unable to grow back.
Chris - It's not that they're just dead?
Geoff - No, it's not that they're dead, in fact they're trying to grow. But the pathway that they need to grow has been destroyed by the injury.
Chris - So what you're saying is that wherever there's a lesion or a cut, or a bit of damage in the spinal cord, this creates some kind of impenetrable barrier that the tiny nerve fibres just can not bridge.
Geoff - Yes. Basically the nerve fibres in the spinal cord run along a kind of pathway cell rather like railway lines or tram lines. And when the damage occurs, these lines are disrupted, they're opened up, and a scar forms which closes off the pathway. So although the nerve fibres have the ability to grow, they're not provided with a pathway to grow along.
Chris - But there are quite a few nerve fibres within the spinal cord, I mean a conservative estimate for just one of the motor pathways is that there's a million fibres in it, so how can you possibly re-lay that pathway for them to be guided where they need to go?
Geoff - Well you can't re-lay the roadway in such a way that everything will grow back. What we are trying to do, and it's only at the experimental stage, (only in animal experiments) is to provide a pathway and see what happens. Now in our situation, what we have found is that less that half a percent of fibres grow back along the pathway that we provide. It sounds very small. But the function that is brought back by that small number of fibres, is very large.
Chris - What's special about that half a percent then? Is there something special about them that mean they're the ones that want to grow and if so do they hold the key to why the other 99.5% wont?
Geoff - Unlikely. What's likely to happen, is that a small amount of signal is carried through by these. A signal is carried across to carry out the function. And the animal, and we hop in future when we do it with people, the person can relearn to use that very small amount of signal.
Chris - But what I'm getting at Geoff is that half a percent of fibres regrow, but the other 99.5% don't. So what's special about the half a percent that enables them to get around this problem, or to grow back? And the 99.5% that don't, why not?
Geoff - It's probably completely random. The pathway's destroyed. Now imagine the pathway was a great 12 lane motorway. We've managed to relay a very small amount of it, a very constrained pathway. So those fibres that are lucky enough to find their way onto it can get through, the rest don't. If we could lay a better bridge than we do, and that's the sort of thing we're trying to do, then you could get even more fibres growing back.
Kat - And what sort of distances are we talking here? When someone for example has a spinal injury, they could just have a very small injury or it could be quite a large crushed area. How far can you make these nerve fibres grow?
Geoff - Now we're talking about experiments in animals, rats, injuries are very small indeed. 1mm. And the fibres will grow across that distance. We do it by transplanting cells, a kind of adult stem cell. We don't have enough cells available to make larger bridges.
Chris - Why do you need to put cells in in the first place, Geoff? Because you said that the scar that's made seems to seal the area and stop these nerve fibres being able to grow through but why do you need to put cells in and what do they do to surmount that problem?
Geoff - Imagine that it's a motorway, a freeway. Travelling over bridges, and half of it falls away in an earthquake. The only way that the cars are going to get across that gap is if you can relay the roadway. Now the roadway in the nervous system is made of living cells. So to repair the roadway you have to be able to transplant the cells in such a way as to bridge the gap.
Kat - So these are more support cells, rather than nerve cells themselves.
Geoff - Yes, they're not nerve cells.
Kat - So you're laying a bridge, really, of these supporting cells, that tell the nerve cells where to grow across.
Geoff - If it was an old fashioned road, relaying the cobble stones. You want the cars to get across it, they're the nerve fibres.
Chris - How do you actually get these cells into the nervous system? Do you have to quite literally open up the entire spinal cord, which is quite a stupendously big thing to do, and then put the cells in where you individually need them? Or are they more intelligent than that?
Geoff - You have to be able to put the cells in the place that you want them. That doesn't mean opening up the entire spinal cord it may mean, for example in our situation, penetrating it with a very fine needle. An injection of sorts.
Chris - So what evidence have you got that this actually works at the moment, Geoff?
Geoff - What we have at the moment is a rat model. And we have shown that with injuries that, for example, impair the use of the limbs, say in climbing or in taking pieces of food, when we transplant the cells the nerve fibres grow back across the injury and those functions come back again. So we can repair this experimental model both anatomically, in structure, and also functionally.
Chris - So if you didn't put the cells in then the rats can't make these limb movements, that function only returns when the cells are put in.
Geoff - The function only returns if you transplant the cells.
Kat - Here's the $64,000 question. How far away do you think we are from seeing this being applicable to humans who've had spinal injuries?
Geoff - Well to answer that let's think of the steps that will have to be taken, and some of which we're taking. The first is, do these cells exist in humans? And the answer is they do. The second is can we get them in a patient in a reasonable way? And the answer to that is Yes, we can get them from the lining of the nose, so we can obtain these cells.
Chris - Why are they in the lining of the nose?
Geoff - Well that's the reason we went there in the first place. As you said, the brain and spinal cord do not repair after injury. But the only nerve fibres which continually repair throughout life in the adult nervous system, are those concerned with the sense of smell. So they have a special roadway, which can repair itself.
Chris - So can you get enough of them to make a repair? Because the human spinal cord's pretty large, the number of nerve fibres in the bridge of my nose is not. Is it possible to get enough of these cells in order to make a decent repair in a human?
Geoff - That's a question we'll have to meet when we get there. But, we are taking these cells from an adult stem cell, which means that it can divide, and in tissue culture, it can make more.
Kat - So you could grow them in the lab, potentially.
Geoff - We do grow them in the lab, unfortunately we still only get a small expansion. Perhaps three fold.
Kat - But if as you say, you only need a very small number of cells to make some kind of functional connection, then potentially that's better than nothing.
Geoff - Indeed. We are hoping to be trying out human cells within the next year or two, in very small injuries of the type where we can hope to get enough cells through a patient. If we can take that step, then we can demonstrate these cells exist in the human, we can obtain them, and they are safe to put in.

- Colour and how brains shape society
Colour and how brains shape society
with Chelsea Wald and Bob Hirshon, AAAS, the Science Society
Bob - This week for the Naked Scientists, we're going to tell you some new things we've recently learned about the brain-in particular, how our brains help shape our societies. I'll talk about money-but first, Chelsea has a report about something all our brains seem to be able to agree on-colour.
Chelsea - Gertrude Stein said "a rose is a rose is a rose." Now, psychologists Delwin Lindsey and Angela Brown of Ohio State University have proven that red is red is red. Using the World Color Survey, in which speakers of 110 different languages categorized colored chips, they found that people universally classify a colour according to its position on the rainbow. In other words, Lindsey says any non-English speaker's word for "red" would include shades like burgundy, brick, and cherry.
Delwin - Perhaps their sample might extend a little bit into the pinks and a little bit into the oranges. But they certainly would not have a colour name that would span two entirely different categories.
Chelsea - But while basic colour classifications seem to be hard-wired into our brains, the actual number of colour names and categories varies tremendously across cultures and languages. For example, Lindsey says some traditional cultures have only two different colour names, one for warm hues and one for cool hues. On the other hand, industrialized countries have far more colour names.
Delwin - In very traditional cultures in which objects within that culture could be identified on the basis of a number of different kinds of features, they would tend to use or have relatively few basic colour terms. But as that culture advanced technologically, so would its capacity to make artifacts or objects that could be distinguished solely on the basis of colour.
Chelsea - ... leading eventually to the hairsplittingly specific colour names you see in clothing or paint catalogues.
Bob - Thanks, Chelsea. Does money encourage self-sufficiency, or selfishness? Yes and yes, according to University of Minnesota consumer psychologist Kathleen Vohs. In a series of nine experiments, Vohs and her colleagues found that the mere suggestion of money - through word games, pictures, or play money - made people work longer on challenging tasks before asking for help. But it also made them less inclined to help others on similar tasks, donate spare change to charity, or even pick up somebody's dropped pencils.
Kathleen - So it suggested that they just thought that everyone should be working toward their own goals without wanting help, just like they had done in the other experiment.
Bob - Thinking about money also made people more interested in working alone, or choosing solitary leisure activities over social opportunities. The bottom line is that for better or worse, money appears to motivate self-reliance. And just as Vohs' research dealt with money in the abstract, rather than actual wealth, other studies suggest that even an academic interest in money can affect your behaviour.
Kathleen - And students and professors both who are interested in economics, they donate less to charity, and they're more competitive when it comes to games that we play in the lab, when there's a competitive or cooperative response that can be given.
Bob - The findings should give ample ammunition to both supporters and critics of capitalism.
Chelsea - Thanks, Bob. We'll be back next week with more stories from the country where money is green. Until then, I'm Chelsea Wald.
Bob - And I'm Bob Hirshon, for AAAS, The Science Society. Back to you, Naked Scientists…

- Why does baking soda reduce smells?
Why does baking soda reduce smells?
We think that it's because bicarb, or bicarbonate of soda, can change the acidity of things. The things that cause smells are generally very volatile chemicals. These are usually cyclical chemicals - ones that have carbon rings and things like that in them. Basically, if you can do chemical reactions between them and the bicarbonate of soda, then they might change their properties and become less volatile. This stops you getting so many smelly chemicals released into the air.

- Why are faint lights brighter if you don't look at them?
Why are faint lights brighter if you don't look at them?
I reckon it's just down to the fact that when you want to see colour, you're reliant on a different population of photoreceptors in your eye, to those which see in the dark. In our eyes we have two different populations of light photoreceptors - in other words cells that can turn light into electrical energy that the brain can understand. In the day time, and in order to see colour, you use a group of cells called cones. Cones come in a number of different flavours, and they see colour. So in other words, when light comes in, (remember light is a mixture of all the different colours), the cones respond selectively to certain wavelengths of light. The light across the road is a flashing blue light, he specifically says that. This means that it might be at a wavelength which he needs his blue cones to be able to see. Now, when we actually look at things very very closely and fixate on them, you're using the part of the retina referred to as the fovea which is where there's the greatest concentration of photo receptors, that's why your vision there is very acute. But also, that's where all the cones are, and where colour vision is, mostly. Now during the night time, and also when you look in your peripheral vision, there are fewer cones in the periphery, and you mainly use what are called rods. Now rods are much more sensitive to light and that's why they're only used in the night time. But they don't tend to be able to decode colours. So when you look at this light out of the side of your eye, you're probably seeing it using rods that are helping some of the blue cones a little tiny bit, because we know that rods can help cones a bit under low light conditions. When you look straight at it, there are fewer of these very sensitive cells and more of the less light sensitive colour specific cells so I think that's probably why you can see things more acutely in the dark, out of the periphery of your vision when they're under low light conditions, but you can read things much more accurately in the centre of your vision.

- Why can your retina detach?
Why can your retina detach?
Basically, there is a natural anatomical cleavage plane between the retina, which is a nervous tissue, and the pigmented layer, which is the back of the eye. Retinal detachment is a different situation. That's when a hole develops in the retina, and fluid goes in between that space and the retina collapses, very much like having a puncture in an inner tube, the retina collapses down. Unfortunately that's just a natural property of the way the eye's been made.

- Can you mend a detached retina?
Can you mend a detached retina?
It's very difficult for me to answer that question because your retina may be detached, and there may be other reasons why you can't see out of the eye. Certainly if your vision's changed recently then I would advise you to have an eye check-up with your local ophthalmologist. I think unfortunately though, with regard to stem cell treatments and anything like that, I don't think there's going to be anything available for the next few years. I would be more inclined in your situation to make sure that your other eye is checked on a regular basis, and that we make sure to maintain the vision that you have at the moment.

- Can a lazy eye be fixed?
Can a lazy eye be fixed?
Well it's very difficult to change the connections within the brain. In a lazy eye, we're looking at a relatively normal retina and optic nerve. It's actually the connections in the brain. And there are some 10^10, to 10^11 neurons in the brain, each of these may have 50 or even 100 different connections. You can imagine how many potential connections there are, to rewire and remodel. And I think really at the moment that's beyond what we can do.









Comments
Add a comment