We catch up with the latest in Cancer research this week, with our very own Dr Kat bringing us the news from the National Cancer Research Institute Conference in Birmingham. We find out how computers can help 'read' breast cancer scans, how to mount an immune response against tumours, and we discover the first vaccine against cervical cancer. Plus, We discover how blood cells can be used as a Trojan horse - sneaking in chemicals to improve body scans, what a 'fossil' of HIV can tell us about how disease spreads, and how beetles create their own antibiotics. And in kitchen science, Ben and Dave use the power of steam to crush cans!
In this episode
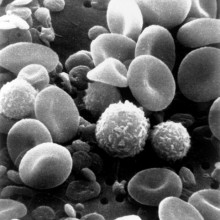
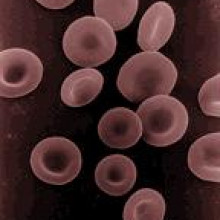
Turning blood cells into Trojan Horses
Scientists in Italy have found a way to boost the power of MRI tracer chemicals - by hiding them inside a patient's own cells.
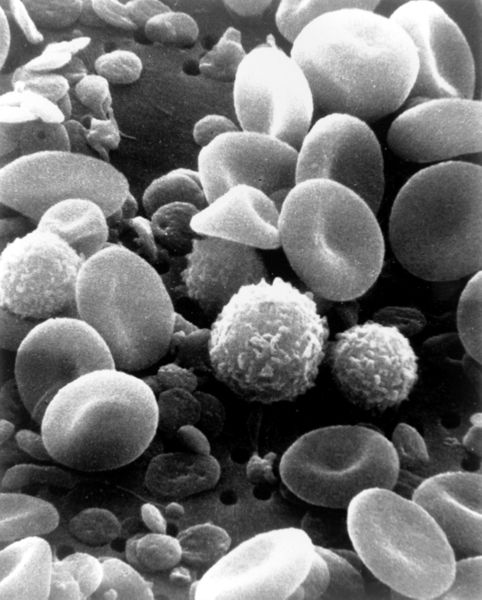 A major problem with contrast agents like iron oxide nanoparticles, which are designed to enhance the signals scanners can pick up from certain tissues is that the agents are rapidly diluted out or picked up and excreted from the body. Now University of Urbino researcher Mauro Magnani and his team, writing in the Journal of Nanoscience and Nanotechnology, has found a solution.
A major problem with contrast agents like iron oxide nanoparticles, which are designed to enhance the signals scanners can pick up from certain tissues is that the agents are rapidly diluted out or picked up and excreted from the body. Now University of Urbino researcher Mauro Magnani and his team, writing in the Journal of Nanoscience and Nanotechnology, has found a solution.
The researchers first incubate a sample of a patient's red blood cells in a solution containing the nanoparticle-contrast agent. Crucially the concentration of the solution is adjusted to make it more dilute than blood plasma. This makes the cells swell up as water moves into them due to the process of osmosis. As this happens the cell membranes become leaky allowing the iron oxide nanoparticles to enter. When the concentration is later returned to normal the cells shrink but the nanoparticles remain trapped inside.
The blood can then be re-infused into the patient where the red cells, carrying their contrast cargo, remain in circulation for the rest of their normal lifetime, which can be up to 120 days. This should enable doctors to make repeated measurements on patients over time, but without needing to top up the contrast. It could prove useful in spotting signs of internal bleeding, for instance post-surgery.
The italian team have signed a deal with Phillips research to pursue the work, which has not yet been tested on humans although the contrast agent itself has and is safe.

Marine "dead zones" could be even larger than thought
Crabs and other crustaceans in the ocean could be the first to suffocate in the increasing number of marine "dead zones" in the world, areas where there is little or no oxygen. What's more, the extent of oxygen deprivation in the oceans could be much larger than previously thought.
These are the findings of a study from Mediterranean Institute for Advanced Studies in Spain published by Raquel Vaquer-Sunyer and Carlos M. Duarte in the journal PNAS this week which looked at how well different types of bottom-dwelling marine creature can tolerate lowered levels of oxygen in the water in the laboratory.
 |
| Picture of the sea floor in the Western Baltic covered with dead or dying crabs, fish and clams killed by oxygen depletion © Kils @ Wikimedia |
The researchers searched through hundreds of other previously published studies of two hundred different species to investigate exactly what the threshold level of oxygen is for life in the oceans to be sustained.
What they found was that there is quite a range in the tolerance of different species to restricted oxygen. Some like the American Oyster can put up with virtually no oxygen, while others are much more sensitive - the young larvae of the rock crab will die if there is less than 8.6mg of 02 in every litre of water.
The problem of lowering levels of oxygen in the oceans stems mainly from a process known as eutrophication, which is triggered by nutrients - mostly agricultural fertilisers - washing off land and into coastal waters. Higher levels of nitrates and phosphates cause algal blooms, both of large seaweeds and single celled phytoplankton. When the algae die they sinks to the seabed where bacteria break them down, using up all the oxygen in the water and leading to the so-called "dead zones".
Climate change may also make the problem worse since warmer water holds less oxygen.
A study published earlier this year in the journal Science revealed that there has been an exponential increase since the 1960s in the number of "dead zones" in the world, which currently cover around 245,000 square kilometres.
That study defined dead zones based on a threshold level of around 2 mg of oxygen per litre. What this latest study now suggests is that the threshold could in fact be as high as 4.6 mg of O2 per litre, which would meant the total extent of marine dead zones could be far greater than was previously thought.
All in all, this means that we made need to think again about the health of the oceans and for water quality standards to be set accordingly to tackle the increasing extent of marine dead zones.
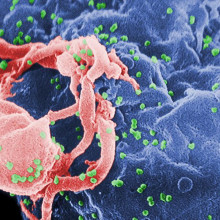
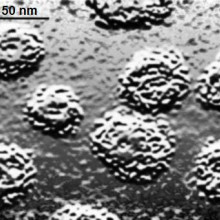
Fossil AIDS virus
An international team of scientists have found new evidence pointing to 1908 as the year when HIV was born. Writing in Nature this week, University of Arizona researcher Mike Worobey describes how he and his colleagues uncovered traces of a fossil form of HIV in tissue samples collected in Africa nearly 50 years ago.
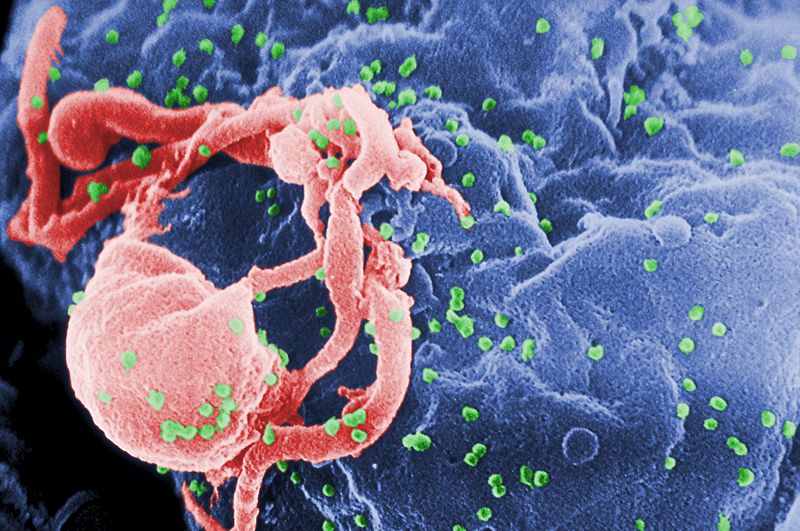 |
| HIV viruses in green budding from a lymphocyte © Centers for Disease Control and Prevention |
Working with scientists in the Democratic Republic of Congo, which was historically a Belgian colony, the team gained access to a collection of old biopsy specimens and tissue samples dating from 1960. The material had been chemically "fixed" and embedded in paraffin, which had helped to preserve it in reasonable condition. The researchers dissolved away the wax and were able to extract genetic material from the samples, which they they then probed for signs of HIV. In one of the extracts, which was from a lymph node biopsy, they struck gold. The sample contained a virus frozen in time, giving the researchers a window back in time to the structure of HIV as it was in the 1960s, twenty years before the world even knew it existed.
The team then compared the genetics of the virus with those of another fossil sequence, uncovered several years ago in a blood sample collected in 1959. The two viruses were significantly different from one another, arguing that HIV had potentially been circulating and evolving in the human population for much longer than thought previously. According to Mike Worobey, "our best estimate for when HIV entered humans is 1908, but it might have been from 1884 to 1924." Either way, what's unarguable is that these dates are slap bang in the middle of the time when the first European settlers arrived and founded large cities like Leopoldville (now Kinshasha), and the team suspect that the high population density, debaunchery and risky behaviour that tends to go on in cities was probably the catalyst that unleashed HIV on the human population.

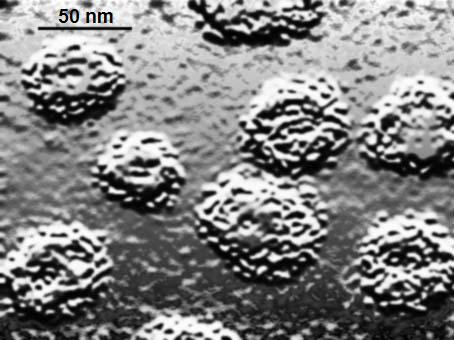
Beetles use antibiotics to protect their food
Beetles use an antibiotic new to science to protect their fungal food stores from attack by other fungal invaders. That's according to a new study published this week in the journal Science by a team of researchers led by Jarrod Scott from the University of Wisconsin Madison.
Southern pine beetles are a major pest in the southern United States where they infest pine trees and cause millions of pounds of damage. The adult beetles dig tunnels under the bark of pine trees, and infest them with a particular strain of fungi, called Entomocorticium, which they carry in a special pouch called a mycanjium. The beetles then harvest the fungus to feed to their growing larvae.
It was already known that the Entomocorticium fungus the beetles carefully farm can be outcompeted by another fungus called Ophiostoma, which disrupts the development of young beetles because they don't have enough food. What Scott and his team have discovered is that the beetles play host to two types of bacteria that produce antibiotics which keeps the invading fungus at bay, but which leave the beneficial food fungus alone.
Using a scanning electron microscope they scrutinised the beetles and their homes and it was noticed that the tunnels dug by the beetles in the pine bark were filled with a type of bacteria called actino-bacteria that no-one had noticed before. The researchers also found the bacteria inside the mycanjium pouches of the adult beetles, where they carry the food fungi. They tested the effects of the bacteria and showed that the invading fungus is 20 times more susceptible to it than the food fungus.
This is the first time that beetle has been shown to seek out the help of not just the food fungus but also the bacteria to protect it.
Back in 2006, leaf cutter ants were discovered to do something very similar, using home-made antibiotics to protect the colonies of fungus that grow on leaf clippings inside their nests. Future research targeting the bacteria and antibiotics used by the Southern Pine Beetles could provide a brand new way of dealing with the pest beetle and others like it.
13:17 - News from the NCRI Conference
News from the NCRI Conference
with Kat Arney
Kat - I'm here at the NCRI conference, that's the National Cancer Research Institute which is an organisation which brings together all the funders of cancer research here in the UK. That's people like the government, charities all sorts of organisations that are funding cancer research. The conference is really a fantastic opportunity to showcase what's going on in the world of cancer research. We've got everyone from people doing the really fundamental lab research. We had a talk this afternoon from Professor Tony Kouzarides from Cambridge University who's looking right at the sort of molecular post-it notes that are put on our DNA that are important in cancer. Right now we're sat above the lecture theatre and there's someone talking about the importance of dying with dignity when people come to the end of their journey with cancer. There's going to be everything from the very basic research through to the much more quality of life, patient care areas.
 Chris - What's the problem with the UK allegedly not doing so well with the cancer stakes compared with the rest of Europe?
Chris - What's the problem with the UK allegedly not doing so well with the cancer stakes compared with the rest of Europe?
Kat - Exactly. The first lecture today was from Professor Michel Coleman from the London School of Hygiene and Tropical Medicine. He's one of the world's leading epidemiologists. That's someone who studies the statistics and the populations to do with cancer and he was pointing out there have been a lot of studies. These Eurocare studies that have shown that Britain pretty much is one of the sick men in Europe. In terms of football league tables we're drifting towards the relegation zone. This is happening for a number of reasons. For a start the Eurocare studies are using relatively old data. In fact, here in the UK around the year 2000, 2002 we brought in a cancer plan. We are turning around what we're doing but it has shown that the UK has been falling behind. It's not actually what people think. It's not about access to drugs. It's actually really to do with early detection. That was one of the most interesting results hat he showed. When you look at five year survival rates across Europe (this is the standard bench mark that people use for how many people survive that long). If you take out from those statistics all the people who die from cancer within a year, that's people who die from very late/very advanced tumours, if you take those people out of the equation Britain comes back in line with the European average. This tells us that in fact in Britain our major problem is diagnosing cancer early.
Chris - Why is that?
Kat - There's a number of reasons. It's obviously a problem with just educating people. We need to get more information out there about what the symptoms of cancer are and that people should not just get the stiff upper lip and think it'll probably go away if I ignore it. Go to the doctor. There's also an issue with educating the GPs as well to spot when someone presenting with certain symptoms may have cancer. You'd think well cancer is a relatively common disease but actually GPs may only see six to ten patients a year who actually do have cancer in a list of 2-3000 patients. It's not really that common for each GP so we need to do more in education for GPs and the public. Also more in things like CT scanning, MRI scanning to try and get cancer detected as early as possible.
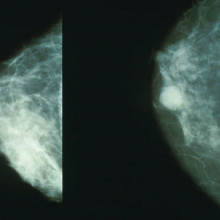
Chris - Also in the news this week is a story about how computers can help to read mammograms which might help to bring out the prediction and detection rates.
Kat - Exactly and this ties in to the whole early detection thing. In the Uk we have a fantastic system of breast screening run by the NHS and it does save thousands of lives. It invites all women in their fifties from fifty to seventy to go for a mammogram every three years. Every mammogram is read by two doctors; two radiologists look at it, look for any dodgy spots and decide whether to call the woman back or not. Now what these researchers, led by Professor Fiona Gilbert at the University of Aberdeen, have shown is that you can use one doctor and a computer-aided detection system. How this works is the computer system scans through the mammogram, spots anything that it thinks looks suspicious and then the doctor looks at it and goes, ' Yep, that looks dodgy...no, that's just an area of fluff or whatever.' Then you only need to have one doctor's time per mammogram. Basically you're holding the workload for doctors. This is really important because in some areas of the country we're seeing screening - the interval of screening is meant to be 3 years - but we're seeing it drift out to three and a half, four years. There simply aren't the resources. This could be a really great way to get more women screened and to help ease the pressure on screening services.
Chris - Which would be very good for affecting that diagnosis detection problem.
21:40 - Human Papilloma Virus
Human Papilloma Virus
with Anne Szarewski, Cancer Research UK
Helen - Cervical cancer is the second most common cancer in women under 25 and the majority of these cancers are caused by infection of members of a family of viruses known as the human papilloma virus (HPV). There are more than a hundred different types of HPV which can cause verrucas and warts and all sorts of things (genital warts) but surprisingly just two types of HPV known as strains 16 and 18 are the cause of the majority of cervical cancers. This means it's been possible to make a vaccine to prevent infection of these cancer-causing strains. This is now being rolled out across the UK and given initially to girls aged between 12 and 13. Dr Anne Szarewski is from Cancer Research UK and she joins us now to explain a bit more about the vaccine. Thanks for joining us. Can we start off first of all with just a little bit about what HPV is and why does it cause cancer?
Anne - HPV is a human papilloma virus and it's an extremely common virus. Basically it's been described as a normal consequence of having sex. It's actually so common that just about everyone's going to get it at some point in their lives. In itself it's quite boring actually but the problem is that some people don't get rid of it. Most people catch HPV a bit like a cold and months later they've got rid of it. A small percentage of people don't get rid of it and it's those people where the virus becomes persistent, where it takes hold. Then it can start to change the cells, it can make them abnormal and it can cause cancer.
Helen - And now there's this brand new vaccine which we've been hearing about i the last couple of weeks. How does that work?
Anne - Basically what it does is it mimics the virus so it's called a virus-like particle. They've taken the coat of the virus and they've made it look exactly like the coat of the actual virus. There's no HPV DNA inside so there's no active anything that could actually give you disease. It's like a ghost in a way and so what it does is it makes the immune system think that the virus is actually there. The immune system recognises this coat and it reacts to it. You get a very strong response from the immune system without there being anything present that could actually harm you.
Helen - So why doesn't the presence of the virus itself not lead to any kind of immunity and a natural way of getting rid of the cancer?
 |
| HPV infected basal tissue © PhD Dre @ wikimedia |
Anne - It's a very interesting question and this virus appears to have evolved and adapted so it kind of sits around. What it does is it invades skin cells. If you think about this your immune system has to be more or less turned off to what goes on in your skin or we would all have loads of allergies. We'd all be atopic, eczematous. Your skin is actually relatively turned off in terms of immunity. The HPV takes advantage of that and it actually invades into skin cells which are kind of under the radar, if you like, of the immune system. It can just replicate quietly - doesn't go in the blood stream so it doesn't alert any part of the immune system that it's there. It just replicates and replicates and then skin is shed all the time. That's how it's passed on from one person to another. The other important thing to know about it is that it's not just transmitted through penetrative sex. It's transmitted though skin to skin contact so you can get it without actually having sex.
Helen - And coming back to the vaccine what sort of numbers do we need to look at in terms of protection to try and combat this as a disease in the population?
Anne - If we're looking at what's called herd immunity where you have enough people vaccinated so that the whole population becomes protected, even those who aren't, then you're really talking around 80% which is quite an ambitious target.
Helen - Absolutely. Why is it we're targeting these girls at this particular age, around 12 years old?
Anne - Two reasons. One is that the vaccines will obviously work best before there's been any contact with HPV. You want to vaccinate people before they've actually had sex. Also, importantly most vaccine actually work best when they're given to younger children and adolescents. In terms of immunity you're actually quite old by the time you're 20 which is rather a sad thought. Your immune system's already running down by then so you get the best antibody response if you actually give it to young adolescents.
Helen - Am I right that there is some level of cross-protection to other types of HPV that cause other problems like genital warts? Have we got any protection against those things as well with this vaccine?
Anne - Then I think it's important to realise there are actually two vaccines. One of them does contain the strains of HPV that would be to genital warts. The one that's been rolled out in the vaccination programme is the one that only contains the cervical cancer types. However it does appear that there is cross-protection against other HPV types but they are the cancer types. Interestingly enough this vaccine that is being used in the programme appears to have quite good protection against HPV 45 which is another of the more important ones in cancer and also HPV 31.

27:47 - Cancer Imaging - Zooming in on Cancers
Cancer Imaging - Zooming in on Cancers
with Herbie Newell, Northern Institute for Cancer Research
Kat - Joining me here in our little booth overlooking the lecture theatre at the NCRI conference is Herbie Newell and he's Professor of Cancer Therapeutics at the Northern Institute for Cancer Research. Hi Herbie.
Herbie - Hi, Kat.
Kat - We're going to talk about some very exciting new initiatives that have been announced in terms of cancer imaging. Let's take a little step back and look at what we mean when we talk about imaging. Why do we need to do it, why's it important?
 Herbie - Ok, so most people are familiar with imaging in the form of x-rays or maybe MR scans and a lot of people would have had those. What we're talking about here is taking it to the next stage where you're not just looking at what's inside the body but you're looking also at the genes and the molecules inside the body. In the case of cancer the genes that have gone wrong.
Herbie - Ok, so most people are familiar with imaging in the form of x-rays or maybe MR scans and a lot of people would have had those. What we're talking about here is taking it to the next stage where you're not just looking at what's inside the body but you're looking also at the genes and the molecules inside the body. In the case of cancer the genes that have gone wrong.
Kat - This new initiative, what's all that about? What's Cancer Research UK and its partners up to?
Herbie - It's a fantastic example of partnership between Cancer Research UK, the Engineering and Physical Sciences Research Council and also supported by the Medical Research Council and the departments of Health in England. What we're doing is we're putting fifty million pounds into cancer imaging reflecting how important this is going to be to attack the cancer problem.
Kat - What sort of things are we hoping to look at? What sort of avenues are we going to be exploring with these very large sums of money?
Herbie - Well, we're going to be using lots of different techniques. First of all, as you say earlier, to try and find cancer earlier. We're expecting to have tests that will tell us when someone might have the cancer but the critical question is where is that cancer in the body? You can send the surgeons in to the right place. Then as we develop new treatments we need to demonstrate that they're working much earlier than we have to do at the moment where we do big clinical trials costing millions of pounds before we can really find out whether a drug's working. We want imaging techniques to find that out earlier.
Kat - What sort of techniques are we actually looking into? We hear about things like CT scanning, MRI scanning, PET scanning. What sort of techniques will our scientists be investigating?
Herbie - So as part of this CRUK and EPSRC initiative we're going to be using any kind of imaging that might work so for example it may be like CT where there's ionising radiation outside the body. It might like a technique called positron emission tomography where you give radioactivity to a patient. It may not involve radioactivity at all like magnetic resonance imaging. We're also looking at some optical techniques as well to try and make microscopy work but in a whole living person.
Kat - So you could actually use light to see inside someone?
Herbie - That's absolutely right. And see right down to the level of the cell, which of course is the thing we're looking for in cancer.
Kat - What sort of areas of research are the development of these techniques going to help? We talked about diagnosis earlier but are there other areas of research and cancer treatment that would benefit from this?
Herbie - Absolutely. These could play a really important part in every stage of the cancer journey. Not only catching it earlier but getting the diagnosis right. Working out for each patient what their prognosis is, how their tumour might go on, whether it's a high-risk or a low-risk tumour. Then when it comes to treatment, making sure that each patient gets the treatment that's most likely to work and also knowng much sooner whether it is working or not.
Kat - A lot of these imaging techniques are based around radioactivity so for example tracers that are put into the body. What areas are being investigated in that aspect because I think this is quite an exciting area of science?
Herbie - Absolutely so one of the big new techniques that has come on recently and the government are rolling this out across the country is a technique called positron emission tomography. It's at the other scale to electrons - they're positive electrons. You give these radioactive materials to people and they're already important for getting the diagnosis and prognosis of lung cancer right, helping with managing patients with some kind of haematological malignancy, some types of lymphoma. At the moment we've really only got one type of tracer that we use. What we'll do in this initiative is develop a whole new family of tracers that will tell us about all aspects of cancer cell biology.
Kat - For the area that you, yourself, work in: the development of new cancer drugs, cancer therapeutics - how do you think these techniques are going to help you?
Herbie - These are going to be absolutely critical because what we'll be able to do is the current experiments that we can do in cell lines in test tubes but we'll be able to do them in the only model that really matters - the patient. We'll be able to look at biochemical reactions when we put in new drugs to see whether we're affecting them in the way we want to. That will help us pick out the winners, get the drugs that are going to be the blockbusters and really help cancer patients much sooner than we do at the moment.
Kat - Sounds like exciting times ahead. In terms of the actual initiative, how's that going to work? £50 million is a bit pot of money to spend. How are you going to divvy it up?
Herbie - As ever in science we've looked at all of the centres who've worked in this area. We've looked at their proposals and decided to fund big-time 9 of the best. This is serious amounts of money that CRU, EPSRC, MRC and the Department of Health, England are putting in. With these centres of excellence we'll be able to set up a network that will get people moving together to get this exciting technology through into patients much faster.
Kat - One of the things that people get concerned about is, for example, the cost of some of these techniques. We hear that CT scanners are very expensive, MRI scanners are very expensive. I can imagine that PET scanners cost a bomb. How do you think if we do develop these techniques do you think it's going to be feasible to roll them out as widely as possible?
Herbie - It's a really important question. Our role first and foremost is to provide hard evidence that says this technique might work, this one unfortunately doesn't look so promising. Having got through that stage it then becomes a social issue that we have to recognise the value that will be brought to the individual patient and also to the whole healthcare economy by personalised medicine. That's what this initiative is all about. It's about focussing the right treatments on the right patients so we don't waste time and money with ineffective and sometimes expensive treatments being given to patients and it's not going to work.
Kat - So you can see straight away of something's not working?
Herbie - Indeed, we've got examples already where you can tell within 24 hours whether a patient is like to respond because the drug has or has not produced the effect you want in tumour cell biology. We need more of those examples.
Wasn’t there something about shining light on skin that was a method of detecting cancers?
Chris - Yes, that's absolutely true. People have found that there's a technique that's called Raman spectroscopy. When you shine light at something the light gets bombarded or ricocheted about like bullets bouncing around a room when it passes through different substances. Depending upon the structures it's passing through you get a different fingerprint scatter pattern. We know what normal skin does. If you shine light into skin which has got a malignant melanoma on it you get a different scatter pattern entirely. Scientists are investigating this as a very sensitive diagnostic technique. You may be able to use it to pinpoint a lesion which you might think I'm not suspicious enough to want to biopsy it but I might be suspicious enough to wave one of these wands at it and it would say, yes that's got a scatter pattern that says it's got a lot of cells which are in an abnormal configuration under the skin. It could be cancer, it's worth doing a biopsy.
44:37 - Why do humans have three different blood groups?
Why do humans have three different blood groups?
Karen Humm, Emergency and Critical Care Vet, Queen Mother Hospital for Animals, London.
All animals do have different blood groups. Humans have a system based on A, B and O. Other animals have different systems. Basically the blood groups are based on little proteins that sit on the outside of red blood cells. The reason it's important for us to be able to tell what blood groups an animal or a person is in is because the blood from one person may not be compatible with another person if their blood group is not the same. In dogs we have a system called DEA 1.1, 1.2, 3, 4, 5, 6 and 7. In cats we also have A and B but they're not the same as A and B in human blood systems. We don't know exactly why people have different blood groups or why animals have different blood groups but it is very important because of the risk of interactions with different blood groups in people and other animals. It might be that some blood groups give an advantage in some circumstances and certainly some ethnic groups are more likely to have blood groups than other people. People from Mediterranean origin are much more likely to have blood group B than people from non-Mediterranean background. The actual causes of them we don't fully understand.
*And Karen also made an appeal for doggy blood donors. There is currently a UK-wide shortage of blood for canine transfusions but you can take your pet down to the vet to help out - they won't take a whole pint!
Dr John Gibson, Veterinary School, University of Cambridge
The reason for ABO groups in humans is not really known but they are of vital consideration for transfusions. They are proteins on the surface of red cells. They are inherited from parents and differ between individuals
- so you can be A or B or AB or have neither (= O). In the blood there are naturally occurring antibodies which react with the blood group proteins which you don;t have. So if you are group A, you will have antibodies against group B. The antibodies will react if they see red cells with the group that they target. So a group A person needs to avoid transfusions from a group B person. As well as ABO groups, there are lots of other blood groups like Rhesus and Duffy. To most of these, there are not naturally occurring antibodies, so they are less important for a single transfusion - but the antibodies can be made following a transfusion.
But the reason for these groups is not really known. There is some association with diseases but it is weak for ABO and no real function for the proteins is known. Some other groups are proteins which do do things like act as membrane transport systems or dockage points for parasites.
Animals do not have the human ABO group on their red cells. But they do have other blood group proteins which are sometimes similarly important for transfusion. Dogs have DEAs (dog erythrocyte antigens), about 8 important ones of which DEA4 and 6 are most significant for transfusions. Cats have groups A, B or AB (but they are not quite like human ABO). Horses have groups including A, C, D, K, P, Q and U. Sheep A, B, C, D, M, R and X. Goats A, B, C, M and J. And so on. Whether these are important for transfusions depends on whether naturally occurring antibodies are present. As for human, its worth testing whether an animal's plasma has antibodies against a potential donor animal's blood.
Are there treatments for womb cancer?
Chris - Yes, there are. This is endometrial cancer. It's not that common but common enough that it's a major problem. Obviously it only affects women because men don't have a uterus. the common associations are it tends to be in people who've been exposed to certain hormones in life. It's also linked ot certain types of breast cancer, it's genetic and it's also linked to people that are carrying a bit too much weight. All those things are risk factors for endometrial cancer. The sign that it might be going to happen is people develop bleeding when they shouldn't be bleeding. In other words, when they're post-menopausal or inter-menstrually so that's a sign there might be something wrong. In terms of dealing with it there are a number of approaches. One of them is surgery. If you remove the organ then that takes the cancer out of the body. The other way to do it is sometimes used in addition to subsequent surgical treatment which is that you can use radiation. You can put these pods, if you like, into the vagina and they contain a radioactive source which is put up close to where the uterus is. The radiation comes out, goes into the cancerous cells and damages them. Then you can kill the cancer that way. Then you withdraw the whole apparatus and this is a way of preventing it. There's a number of different treatments and there's also people investigating various hormonal treatments as well. I don't know of any clinical trials that are doing that at the moment.
Is there some way of detecting cancers using sound waves?
Chris - Definitely. This was experimental but very exciting. One of the big problems with cancer spreading around the body or cancers that may be so tiny or almost impossible to see on the skin surface, for example, is how do you know if they're already in the blood stream? Cancers throw off cells. These are called metastaces or metastatic cells. If you've got malignant melanoma which is making a lot of melanin, a dark pigment what you can do is take blood samples and there might be one in a million cells in the blood stream which is a malignant melanoma. Scientists have found that if you zap this with laser light at a frequency which the melanoma will absorb but other cells won't then the cell can be made to resonate. It makes a sort of snapping or ricocheting-like noise which you can hear with a very sensitive microphone and this tells you the cells are there.
How do plants protect themselves from UV damage?
Chris - There was a study that was done on edelweiss, not just the song in the Sound of Music. This is a plant that grows high up in the alps. Because it's growing at altitude it's exposed to a lot of solar radiation and a lot of ultraviolet so how does this fend off? Scientists recently published a paper in which they looked at the surface of the leaves of edelweiss and they found these tine hairs. If you zoom in on the hairs the hairs are made of even tinier filaments which are about 100nm across. 100nm is roughly the wavelength of ultraviolet light. These hairs interfere with or interrupt the passage of the ultraviolet light, stopping it getting onto the leaf surface. Instead they channel the ultraviolet into some water in the middle of the hair and this soaks up the UV and protects that plant. Helen - Could we make this into anything we could use? The new generation of sun creams perhaps?
Chris - That's not such a silly thing to say because yes, people are saying we might be able to make nano technology sun cream. Sun cream uses titanium dioxide that you just spread on the skin. They're saying if we made edelweiss extract you could rub this on the skin and the same trick might work to fend of the UV rays.










Comments
Add a comment