Inside the Ebola Epidemic
Ebola has rocked the world in 2014, but why has this outbreak been so devastating? This week we get inside Ebola to find out about the virus itself, and how it causes disease and spreads. We talk to healthcare and charity workers on the ground in West Africa to find out how what is being done to stem the epidemic; we catch up on progress towards a vaccine and we hear how the virus is also crippling gorilla populations. Plus, in the news, the latest on the Rosetta mission to comet 67P-Churyumov-Gerasimenko and how Wikipedia can reveal what diseases are circulating and where...
In this episode
01:09 - Landing on a Comet
Landing on a Comet
with Professor Andrew Coates, University College London
European space scientists have made history. As part of a mission called 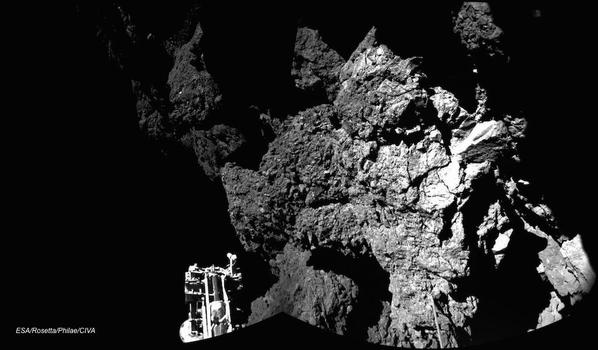 Rosetta, they have landed a washing machine-sized probe called Philae on the surface of a comet, over 300 million miles away. This needed precision equivalent to firing a bullet from London and hitting the head of a nail in New Delhi.
Rosetta, they have landed a washing machine-sized probe called Philae on the surface of a comet, over 300 million miles away. This needed precision equivalent to firing a bullet from London and hitting the head of a nail in New Delhi.
But not everything has gone to plan. Philae didn't land in the spot it was supposed to and now, it might not get enough lights to charge up its solar panels. UCL space scientist Andrew Coates developed one of the instruments on the Rosetta Orbiter and spoke to Chris Smith.
Andrew - Well, what happened with the lander was, it landed first of all, almost in the right place, in fact within 10 meters of the expected point. But unfortunately, there are a couple of systems which were supposed to happen, which didn't, one of the things where the thruster which was supposed to hold on to the comet, the other thing was harpoons, which were supposed to anchor it to the comet. And those didn't work. What happened was it bounced off to a completely different location. In fact, the location that it bounced off to haven't quite been found yet. But within the last few minutes, it's been shown that there was a photograph after the bounce which shows the direction of travel. So, that will help to narrow down where it actually did. But when it got to the surface, it landed unfortunately very near to an ice cliff on the comet and also, surrounded by boulders, in a place where sunlight actually was very limited. So, that meant that there was a limited battery life. So the comet rotates every 12 hours and the place where it landed is about 1 ½ hours of sunlight. To add to that it was actually on its side. So, it was trying to do the experiment on the surface and it successfully did do all the experiments in the first experiment block, 100%. So actually, I think that's pretty impressive to get that data back to Earth before the batteries run out.
Chris - What experiments has it done, Andrew?
Andrew - Well, what it has been able to do is obviously take images. There's images of the location, there's panoramic images. Basically, all of the experiments on board were exercised in some way, including a drill that was extend to try and drill at the surface and get the pristine material from the cometary nucleus, into the laboratory to do some tests and so, all of that was successfully done. So, drilling was done. It's not quite sure exactly whether we caught a pristine sample yet. It certainly was able to sample the vicinity and also to do some measurement of the physical structure of the surface and those sorts of things.
Chris - Some of the big broadsheets are saying today and yesterday that there could be data now loitering on the probe which can't be returned but which could be very, very important. Is that because it's just out of power and can't transmit the data back?
Andrew - Well actually, 100% of the data was in fact transmitted back from the first experiment sequence. So, the next step is to try and charge up the batteries and do some more experiments. I mean, it was a huge success really to get all the data back on on Friday night which possibly could be off the orbiter, so there is not one bit of information left on the lander that could in principle be sent back. So actually, it's a huge success to have gotten all that data back. But the next step is to try and charge the batteries and this will probably take days or weeks, possibly months even. So, to put in perspective, the comet is traveling around the sun and it gets closer to the sun over the next few months up until august next year. And so, every moment, the amount of sunlight is increasing. So, although the power available per day or the sunlight available per day is relatively limited, the amount of power will actually be increased. In addition to that, it was possible to actually move the probe a little bit on the surface to mean that there's more solar panels now which are facing the sun than there were before. And so again, that is a good possibility for being able to power it up in the future. But in the meantime, I think 100% success rate in getting the data back from the first few hours is actually very, very impressive and putting combination with experiments on the orbiter where we're involved, this means that this was a fantastically successful mission which is still going to be sending us back data over the next few months.
Chris - What do we hope to still learn or what have we learned so far? Why is this important?
Andrew - With the orbiter, there's a number of experiments on board. There's 11 experiments on board the orbiter and 10 on the lander. Comets are very important because they're very old members of our Solar System. We're taking in fact 4.6 billion years. So, they're the building blocks really of the planet. So, formed in the region between Uranus and Neptune where it's cold enough for water ice to be in a solid state. And so comets, they're building blocks really of the outer Solar System. So, they were made there and then kicked out to sort of storage regions. One of them is the Kuiper Belt which is in the plane of the planets. The other one is Oort cloud which is a sort of spherical cloud of comets, a quarter of the way to our nearest star. So, they've been in cosmic deep freeze effectively from the beginning of the Solar System. So every time one of these comets comes into the inner Solar System, there is the possibility to look back really about time, 4.6 billion years ago.

06:19 - Predicting outbreaks with the Internet
Predicting outbreaks with the Internet
with Sara Del Valle, Los Alamos National Laboratory
Have you ever looked up your symptoms online in a bout of paranoia? Although this isn't recommended, you might actually be helping the people who look after our public health. Experts at Los Alamos in New Mexico have discovered that the number of hits about different illnesses on Wikipedia pages actually predicts when and where outbreaks of disease are happening, long before healthcare services get wind of them. Sara Del Valle explained the process to Kat Arney...
Sara - The idea behind the study was to see if we could use Wikipedia not only to monitor but also to forecast diseases around the world. We looked at influenza, which is transmitted from person to person. We also looked at dengue, which is transmitted from mosquitoes to people and also tuberculosis, which is an airborne disease.
Kat - What kind of countries were you looking at?
Sara - We looked at dengue in Brazil and Thailand; influenza in Japan, Poland, Thailand and the United States; tuberculosis in China, Norway and Thailand. And we looked at Ebola in Uganda.
Kat - So, what can web statistics from Wikipedia tell us about these diseases?
Sara - People go to Wikipedia before they actually go to see the doctor. Wikipedia releases hourly counts of how many people access each article on different languages. So, if people go to their Wikipedia article for flu, we can see the article was accessed in English or in German or in Russian or in Portuguese. And that's what we decided to use to monitor the prevalence of diseases and also, to forecast because you typically go to a Wikipedia before then so you will see them later on on regular public health data.
Kat - How early can you predict that there might be an outbreak of this disease?
Sara - It varies. For flu, we were able to forecast up to 4 weeks in advance. For dengue too, we were able to forecast 4 weeks in advance. For tuberculosis, we could only forecast about a week in advance.
Kat - With something like Ebola, I mean, I've looked at the Wikipedia page. How do you know people aren't just curious about the disease rather than thinking, "Oh, maybe I've got this"?
Sara - It's interesting that you mentioned that because it appears that Ebola is just an interesting disease that is accessed on a regular basis, given that few numbers of cases in Uganda, the number of people go into the Ebola page just completely messed up the model. When there's something going on, or there's a lot of media hype, or attention to a specific disease, I think it would be very hard to pick up some of those patterns.
Kat - So you can see - you think, it looks like there's an outbreak of this disease in this country. What should you do with that information?
Sara - Our goal is for public health officials to use this kind of information so that they can prepare and plan ahead of time if they know that people are going to be showing up with flu symptoms or with dengue symptoms that they can be prepared. They have staff and resources to treat those people.
Kat - How are you going to try and take this forward and make this a better tool?
Sara - Right now, we are working with the Wikipedia Foundation. I think once they move forward towards and stratify the data then we can do better analysis on country disease pairs. We only looked at 14 different contexts and we would like to look at more diseases and more countries. We were able to train our model using data from one country and then to forecast a different country. I think that can completely revolutionise bio-surveillance for diseases, because there's many countries we know that they don't really collect a lot of data. If we can show that we can use other countries that actually collect data and have very good public health departments to train their models and we can forecast diseases in developing countries, I think that would be a great contribution to the public health system.

10:37 - Lightning strikes set to increase
Lightning strikes set to increase
with Victoria Gill, Science Reporter
Every second, the world gets zapped by about 100 lightning bolts - that's nearly 9 million strikes a day. But we could see that number climbing dramatically, owing to climate change according to a new study by scientists at the University of California, Berkley.  This increase could harm people, it could start fires and it could even further intensify global warming itself by producing more greenhouse gases. Victoria Gill told Chris Smith why we can expect more frequent bolts from the blue in future...
This increase could harm people, it could start fires and it could even further intensify global warming itself by producing more greenhouse gases. Victoria Gill told Chris Smith why we can expect more frequent bolts from the blue in future...
Victoria - Lightning, as well as being very dramatic, is really important because it causes chemical reactions to take place in the upper troposphere where our weather is. And our atmosphere being mostly nitrogen and oxygen, that causes lots of chemical reactions between those two gases. So, it produces lots of nitrogen oxide and also feeds chemical reactions for greenhouse gases. So, it's not just this big dramatic display. It's also doing stuff to the chemistry of our atmosphere. What these researchers were trying to find out was exactly how much more lightning we should expect as temperatures increase over the next century.
Chris - And that would be relevant to global warming.
Victoria - That would be relevant to global warming because we already have a temperature increase that's forecast up until 2100. It's also because lightning does change this atmospheric chemistry. It'll also feed it back into that global warming by actually directly and indirectly producing these puffs of greenhouse gases by feeding these chemical reactions.
Chris - So, what did they do?
Victoria - Well, they actually had access to quite an amazing data set. In the US, there's a thing called the National Lightning Detection Network. So, every time you get a lightning strike, you get this electromagnetic pulse and that's picked up by a radio receiver and they can detect that within a 1-km radius. So, they've actually produced this animation of over the year 2011, how many lightning strikes were all over the US. What they can do is then match that with the temperature changes and then they can project that forward and say how many more lightning strikes we'll expect over the next century.
Chris - And how many more can we expect?
Victoria - For every degree Celsius increase in temperature, we get a 12% increase in the frequency of lightning strikes. Now, to put this into real terms, what David Romps at the University of California Berkley says that means, is that for every 2 lightning strikes in the year 2000, there'll be 3 in 2100, so quite a noticeable difference.
Chris - I did read somewhere that at any moment in time, there are 2000 thunderstorms crackling away all around the world. Does it really matter though if we get more lightning strikes by 12% per degree in a hundred years time?
Victoria - People do die from being struck by lightning, but that is very infrequent. But you do see the huge frequency of these thunderstorms in this animated dataset. Every single time one of those lightning strikes is happening, there's this little puff of nitrogen oxide and also, all of this extra energy that's feeding the chemistry in the atmosphere. So, that is contributing to greenhouse gas formation in the atmosphere. Also, lightning storms trigger half the wildfires in the US apparently. So, what that means is that these very unpredictable patterns of lightning are going to increase in frequency and that's going to be triggering more wildfires which is obviously a real problem.
Chris - So, we've got a situation where we could see an acceleration in the numbers of lightning strikes. This could in turn affect the composition of the atmosphere, including producing more greenhouse gases which could in turn, increase the temperature and increase the frequency of lightning even more. So, this is important to sort of model into climate change modelling and scenarios going forward I suppose.
Victoria - Yeah, exactly because those little puffs of nitrogen oxide are very, very small and obviously, very quick. When you see a lightning strike, it's extremely fast. If that's just growing exponentially in its frequency then that's going to build up and become something that is significantly contributing to the change in the chemistry of our atmosphere. This is a really interesting physical and what will be very visible change in our weather that's directly related to global warming.

14:46 - Switching off!
Switching off!
with Professor Jeremy Sanders, University of Cambridge
For universities, being at the forefront of academic research comes at a high price because, according to the Carbon Trust, annual energy costs in the UK higher education sector are £400 million and contribute CO2 emissions of around 3 million tonnes per year.  To cut these costs, Cambridge University have set up 'Switch Off Week'. Georgia Mills went to see Jeremy Sanders, Pro-vice Chancellor of Institutional Affairs, who explained why the University has decided to turn out the lights...
To cut these costs, Cambridge University have set up 'Switch Off Week'. Georgia Mills went to see Jeremy Sanders, Pro-vice Chancellor of Institutional Affairs, who explained why the University has decided to turn out the lights...
Jeremy - Every year, the university spends £16 million on electricity and gas. That's over £1800 an hour. One of the things we need to do is to reduce that. In part, we can do that through big projects of changing buildings, changing the way that we generate and buy electricity. But another way we can do that is for students and staff across the university to use less electricity by switching things off. And so, what 'Switch Off Week' is, is a way of engaging staff and students across the university. A variety of activities and road shows designed to raise people's consciousness and get them to switch things off.
Georgia - What kind of activities are you using to try and get this 'Switch Off' to happen?
Jeremy - Well, today is thermal Thursday. So, as you can see, I'm wearing a warm jumper. The more clothes that people wear, the more we can turn down the thermostats in their offices and in their labs. We're getting people to think about turning off the lights, turning off the computer when they don't need it, turning off their lab equipment when they go home in the evening. One of the activities is a competition where we're asking across the whole university, "What's your best idea?" now, the first time we held 'Switch Off' week 2 years ago, the winner of the competition was wireless occupancy sensors. This is now a project that we're rolling out across much of the university. What the wireless occupancy sensors do is, they detect if there's any movement in the room. If there's no movement in the room for a couple of minutes, you assume that there's nobody in there or maybe they're asleep. But then the lights go off automatically. That has the potential to save a lot of money and a lot of carbon.
Georgia - The statistic you said earlier about the university spending over 1800 pounds an hour on electricity is shocking. Is this something of an inevitability when it comes to a research institution or do you think there's a lot that can be done to cut this down?
Jeremy - Well, it's certainly true that if you have a science intensive institution, there will be a large electricity demand. We have a lot of computers, we have a lot of labs that need to be kept at constant temperature, and so on. The question is, what's the best way to minimise that demand? So, we've just built a data centre where we are going to collect together as many of our really intensive computers as possible and we're going to put them in an environment where the cooling will be very efficient. In many rooms where we have heavy computers, we spend as much electricity on air-conditioning as we do on running the computer. There's a huge saving to be made by bringing all those machines together and cooling them efficiently. So yes, there will always be a big demand but there's a lot more we can do.
Georgia - Do you have any tips for people who are listening and wondering small ways they can cut down on electricity use?
Jeremy - What I would say is, put on more clothes and turn down the thermostat. That's the most important thing to do. The next time you make a cup of tea or coffee, either heat up one cup in a microwave or just put less water in the kettle. We waste a huge amount of electricity across the country by filling up the kettle and then just making one cup.
19:02 - What is Ebola?
What is Ebola?
with Dr Suzie English, Addenbrooke's Hospital
Ebola has been dominating the headlines for many months with governments and healthcare providers worldwide caught off-guard by the outbreak that's happening in West Africa. 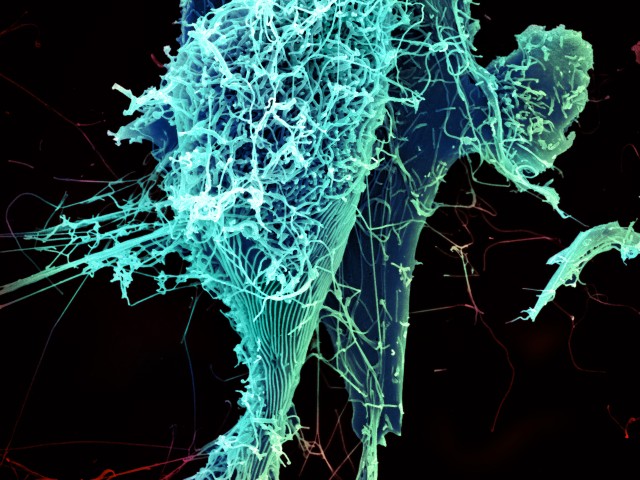 Recently, according to the WHO, the death toll passed 5,000 people and the number of infections is still rising. Suzie English, a virologist from Addenbrooke's Hospital in Cambridge, explained to Chris Smith what Ebola is and how it causes disease...
Recently, according to the WHO, the death toll passed 5,000 people and the number of infections is still rising. Suzie English, a virologist from Addenbrooke's Hospital in Cambridge, explained to Chris Smith what Ebola is and how it causes disease...
Suzie - Ebola is a viral infection. It was discovered in 1976 after two very large outbreaks in central Africa in Zaire, now the Democratic Republic of Congo and the Sudan. In between human outbreaks, the virus is thought to hide out in fruit bats. At the beginning of outbreaks, it's thought to be transferred to humans through the consumption of or contact with bush-meat which may be the bats themselves or other animals that have been infected by bats.
Chris - What can you tell us about the present outbreak? Where did it come from and why has it been so dramatic?
Suzie - Well, the origins of the present very large outbreak in west Africa are not precisely known, but it is thought that there is an animal origin and that it has been transferred into humans through the consumption of bush-meat. The present outbreak began in a very rural area of Guinea, near the Liberia and Sierra Leone borders where there is a lot of cross border travel. And the viruses rapidly spread through those countries.
Chris - Do we know anything about how it got started in the first place?
Suzie - The index case has been traced back to a small child in December of 2013 in Guinea. Early work has looked at how the virus was transmitted firstly to people who cared for this child and then for people who cared for those people, and looked at in particular, the amplifying effects of hospitals and funerals in propagating the infection.
Chris - And talking of propagating the infection between individuals, how does it spread because there's been enormous controversy in the media about whether or not there's airborne spread or other mechanisms? How does it get about?
Suzie - So, Ebola is spread from person to person through direct contact with infected bodily fluids. A person who's infected with Ebola is particularly infectious during the later stages of their disease when they produce vast amounts of viruses in many bodily fluids. And also, people who have recently died from Ebola are also very infectious. Their bodies are very infectious. Funeral practices can propagate the infection when a large number of people come into contact with the recently deceased person's body.
Chris - Once a person has got it, a, how do we diagnose it? And, b, what can we do about the infection?
Suzie - So, when a person first becomes infected with Ebola, there's a period of silent multiplication of the virus within the body. This is called the incubation period. During the incubation period, the person is asymptomatic which means they don't have any symptoms, they don't have a fever, and they're not infectious. The first detectable manifestation of the infection is a fever which the person may or may not be aware of. And this is why people who've been exposed to Ebola have their temperature monitored. After the onset of the fever, the patient may develop flu-like symptoms - sore muscles, sore joints, headache, severe fatigue, and then after a few days may develop tummy pains, lack of appetite, nausea, vomiting and diarrhoea. Towards the end of the first week of their disease, the patient will develop dysfunction of many organs. So, they may develop kidney damage, liver damage, an inability to clot their blood and a severe immune response throughout their body which can damage their body further. For those who do not survive Ebola, this is the time when they develop multiple organ failure and shock. For those who survive Ebola, the disease typically lasts for approximately 2 weeks. But even after they recover from the virus, they can still be shedding the virus in their bodily fluids for some time and need to be retested to see if they have cleared the virus. In terms of treatments, the treatments fall into roughly three categories and all of them are under study. So, there's no definitive treatment for Ebola at present. The first category of treatment is supportive care. So, this is designed to support the body through the period of the disease until their body can fight off the infection. The second broad category of treatment are immunological therapies. These treatments involve giving antibodies from people who survived Ebola or synthetic antibodies to try and neutralise the virus and prevent it from infecting more cells in the body. The last category is anti-viral drugs which aim to prevent the virus from replicating in cells after they've infected the cells.

23:45 - The fight against Ebola
The fight against Ebola
with Marie Blackman Northwood, Public Health England
There's no cure for Ebola, however people can be treated although facilities in  countries like Sierra Leone are under huge strain coping with the outbreak and the death rate is extremely high. Charities and governments around the world are sending people and equipment into the infected areas to keep on top of the outbreak. The UK government have recently pledged £20 million to open and operate three diagnostic laboratories to help test for the disease.
countries like Sierra Leone are under huge strain coping with the outbreak and the death rate is extremely high. Charities and governments around the world are sending people and equipment into the infected areas to keep on top of the outbreak. The UK government have recently pledged £20 million to open and operate three diagnostic laboratories to help test for the disease.
One of those labs is in Kerry Town, which is one of the areas worst hit by Ebola in the west of the country. Chris Smith caught up with Marie Blackman Northwood, a biomedical scientist with Public Health England. She's traveled out to Sierra Leone to help to set up and run one of these labs...
Marie - At the moment, the treatment centre is based on receiving referral cases throughout the community. So, that's a lot of small villages based around Kerry Town. People can travel for miles. It's not quite like England where things are very accessible and down the road. So, they rely on an ambulance service. to be able to get them to the treatment centre. We've had a few cases admitted. It's sometimes adults, children at different stages of being infectious. We have had people who have moved on and done well in the centre, but we have had casualties of Ebola as well. However, we have had people admitted who have had malaria which exhibits very similar symptoms. So, we are doing testing for both Ebola and malaria. I don't think someone's being quite so happy see a malaria positive test because it does mean that we can separate that person from someone with a suspected Ebola and effectively treat as well.
Chris - What are the facilities like?
Marie - It's very basic but good at the same time. we did bring in a lot of equipment from the UK. We are using a polymerase chain reaction platform. We have brought in portable cabinets to isolate the organism. And so, we're working in very safe practices. It's very important that we can get the turnaround times which we aim for four hours to give results especially for patient within the centre.
Chris - How are the locals taking to your presence?
Marie - They have been absolutely marvellous. They welcome the help. For them, it's seen as, we need people to come in and help because our health system has fallen down. The economy was on the up and the sad story is that because of Ebola, it's taken quite a hit. So, to have people coming in and still wanting to come and visit - what is a very beautiful country - is a joy to them, but a lot of people's response towards myself and my colleagues has been thank you.
Chris - And you're coming home soon. Are you at all concerned because there have been a number of cases of people who've been working like you are at the moment and they faced quite a bit of prejudice, they face people ostracising them because of fears that they may pass on Ebola?
Marie - I did have my concerns before I left, but I did say to people that you've got to look at this in a rational way. I'm working in the laboratory quite protected. I've had training. I've had to wear a lot of protective gear. I've had limited social contact out here. also, we have screening processes up and running now at the airport. I've been screened so many times whilst out here as well. And I've taken a self-responsibility of monitoring myself. So, I wouldn't want to put anyone in danger especially my family that I'm coming back to and I'm really looking forward to hugging and being around.

27:32 - The knock-on effect of Ebola
The knock-on effect of Ebola
with Dr Yaron Wolman, Unicef
The Ebola outbreak doesn't mean that all of the other major health problems, like  malaria, that were previously in affected countries like Sierra Leone, have disappeared. In fact, the strain of coping with Ebola is having some serous knock-on effects and it's robbing people of routine care for many other diseases and even child birth. Dr. Yaron Wolman is the head of the child survival section at Unicef. He's currently in Free Town, the capital of Sierra Leone, where he's leading the charity's efforts to stop the outbreak becoming a full blown humanitarian crisis. He explained to Chris Smith what factors turned Sierra Leone into a ticking time bomb for Ebola...
malaria, that were previously in affected countries like Sierra Leone, have disappeared. In fact, the strain of coping with Ebola is having some serous knock-on effects and it's robbing people of routine care for many other diseases and even child birth. Dr. Yaron Wolman is the head of the child survival section at Unicef. He's currently in Free Town, the capital of Sierra Leone, where he's leading the charity's efforts to stop the outbreak becoming a full blown humanitarian crisis. He explained to Chris Smith what factors turned Sierra Leone into a ticking time bomb for Ebola...
Yaron - One of the reasons that the Ebola outbreak has expanded so quickly in this country is that the health system was very fragile even before the Ebola outbreak from very long civil war in these countries. The impact of the Ebola outbreak on this very fragile health system is that less women and children are visiting the health facilities. Many of them have less access to all the essential primary healthcare services like vaccinations, treatment for malaria, treatment for pneumonia, treatment for diarrhoea, skilled birth attendants. Things that were there before the Ebola outbreak are not there anymore. People are scared to go to the health facilities because they're afraid of being infected there. And also, in some of the health facilities, some of the health workers unfortunately got infected and some of them have died. So, there are also some health facilities that for some period of times do not have the health workers to provide the healthcare services there.
Chris - In theory, the impact of the other problems could be far and away much larger than the impact that Ebola has had.
Yaron - Well, it's very difficult also to differentiate between the two because they're very strongly interlinked. Currently still, probably more people are affected by malaria than they are affected by the Ebola number-wise. But the nature of the expansion of the Ebola outbreak means if we do not contain it in the coming weeks, we might face a very severe catastrophe like previous large scale global outbreaks from the early 20th century like the Spanish flu for example. So, unless currently we do manage to concentrate all our efforts and to contain the outbreak in the coming weeks, the scope of the outbreak will deteriorate very quickly and we might encounter massive numbers of patients because of the very high mortality rate, massive numbers of casualties.
Chris - Can you paint a picture for us of what the situation is like at the moment on the ground?
Yaron - Well, I'm based in the capital which is called Freetown. Freetown is one of the epicentres of the outbreak currently. We do see even here that it's very difficult to provide proper treatment services to the Ebola patients. However, because of the efforts of the different development parties with the government, gradually, things are improving in terms of the number of beds that are being available for treatment and the laboratory facilities. But still, the number of cases are on the increase. We do need to ensure that in such a setting who have crowded urban settings with slums, we do manage to invest enough, both in the prevention of Ebola. So, very strong social mobilisation and communication campaigns and at the same time also in the Ebola treatment part, which is to ensure that there are enough treatment beds for patients, enough laboratory capacity in order to provide rapid and accurate diagnosis of the cases. And at the same time also, cater to the special vulnerable groups like children and women because women and children are disproportionately affected by the outbreak and we have multiple cases of children who are either they're mothers or both their parents have been affected by the outbreak. They have suspected contacts, but they haven't yet develop the symptoms. These are the kinds of challenges that all of the partners, the development partners are encountering in our efforts to work together with the government to contain the outbreak.
Unicef is one of many national and international charities helping to fight the Ebola outbreak, to find out how you can help click
here.

31:59 - When will an Ebola vaccine be ready?
When will an Ebola vaccine be ready?
with Eleanor Malone, SCRIPintelligence
With Ebola raging in west Africa and fear growing on other continents,  our limited ability to treat this lethal virus has become an increasing public health issue. Can Ebola be halted in a way that does not rely on ineffective treatment practices? Competing pharmaceutical companies have been working to develop an Ebola vaccine and are now in human trials.
our limited ability to treat this lethal virus has become an increasing public health issue. Can Ebola be halted in a way that does not rely on ineffective treatment practices? Competing pharmaceutical companies have been working to develop an Ebola vaccine and are now in human trials.
Kat Arney spoke to Eleanor Malone, the editor of pharmaceutical analysis news source SCRIPintelligence, who updated her about the progress being made with vaccines...
Eleanor - We're at a very early stage - phase one testing which is safety testing in humans after animal testing. So that vaccine and another one that's slightly ahead of that by GlaxoSmithKline and the American National Institutes of Health are both in humans. They've done well in small numbers of monkeys. They stopped the monkeys catching the virus and the ones that were exposed who hadn't had the vaccine died. So, that's promising.
Kat - Yeah, I'd say.
Eleanor - At the moment, they're phase one testing in relatively small numbers of people, healthy volunteers. But yeah, we're still quite at an early stage. The good news is that they kind of accelerated the trial process. So, the next stage would be efficacy testing and then there'll be bigger trials. All of the data is being fed back to the regulators and advice is coming through and the data from different vaccines is being shared in a way that the pharmaceutical industry wouldn't normally share data. So hopefully, we'll have good safety data by the end of this year and go into efficacy testing maybe even by the end of this year as well.
Kat - So, these trials right now, they're just checking basically, "It's safe and you can give it to people"?
Eleanor - Yeah.
Kat - And the pharmaceutical industry is quite known for being very slow with trials. It takes a long time to get through all the regulatory process. We're right now in a crisis situation in west Africa. You say there might be safety data coming along the line. How soon do you think it could be before larger trials are available, maybe testing how effective it is or even a vaccine coming on to the market?
Eleanor - Actually, quite soon - by the end of this year or early next year we should see the efficacy testing if all goes well. They're also already working on scaling up the production so that they could have tens of thousands of doses available quite soon and make and moving into hundreds of thousands of doses if all goes well in the first half of next year. And then the efficacy testing will be out in west Africa.
Kat - Who would be the priority for these vaccines?
Eleanor - Well at the moment, it's the healthcare workers. I think it depends quite a lot on what we get from the data because there are certain groups of people for whom this may not work or may be dangerous - HIV infected people, children, pregnant women. There are large numbers of these people in west Africa, so we have to see what the data are.
Kat - And it does seem like this has happened extremely quickly. Is it that maybe it's been particularly easy to develop the viruses or are there other factors at work?
Eleanor - I think they're not the most difficult vaccines to develop, but there has not been an economic incentive in the past to develop a vaccine for Ebola, partly because it's in Africa and also because hardly, anyone has ever had it. But things are definitely speeding up with huge attention and public money going into this and also, the companies have stepped up in the last few months. They're collaborating with each other, they've put their own money into it, and they're not going to make money on it.
Kat - It does seem like quite a nice thing for the world to get behind.
Eleanor - It's amazing, yeah.
Kat - It's a good story from the pharmaceutical industry.
Eleanor - Yeah, if we can learn from this and apply it to other diseases, it would be fantastic.
Kat - We've talked about three vaccines that are heading into trials at the moment. What about other vaccine approaches or even treatments that might actually get rid of the virus once people have it?
Eleanor - There are various other vaccines at earlier stages. Our databases have around 20 or more products in kind of pre-clinical early stage development. And so, the treatment approaches are quite varied, all still very early stage. There's monoclonal antibodies, various viral treatments like an approved flu treatment which could be used.
Kat - Because flu is a virus as well.
Eleanor - Yeah, it may work. And some of them are good because they're easy to administer or they're already manufactured in sufficient numbers. So, that makes it better, but they're not looking as effective. Other are very difficult to make or unpleasant to administer.
36:18 - Tracking the Ebola outbreak
Tracking the Ebola outbreak
with Dr Colin Russell, University of Cambridge
Why has the Ebola outbreak been so hard to control, and why has it hit the 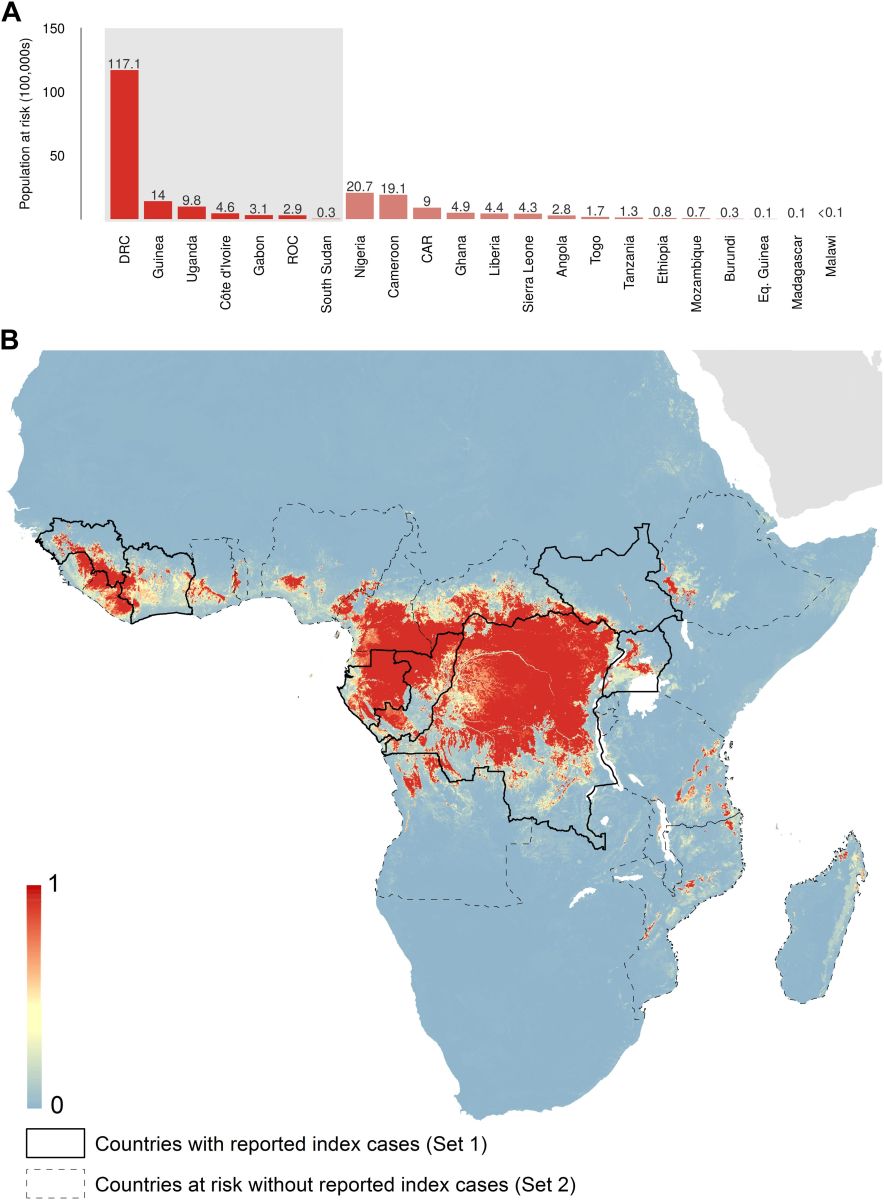 world now? Colin Russell, a disease modeller from Cambridge University, explained to Chris Smith how many epidemics begin with an animals reservoir of the disease...
world now? Colin Russell, a disease modeller from Cambridge University, explained to Chris Smith how many epidemics begin with an animals reservoir of the disease...
Colin - The majority of pathogens that are perceived to pose a pandemic risk originate in animals. These are things like influenza viruses that come from pigs or from birds, Ebola viruses, which we typically get from bushmeat but have their original home in bats, and a plethora of other pathogens which cause a tremendously severe disease when they get into humans. The difficulty is that there's a tremendous number of pathogens that exist in animals all over the world. One of the main challenges that we face as scientists and public health officials is, picking which one of those is most likely to cause the next pandemic and developing measures to be able to mitigate the spread of that virus, should it become transmissible from human to human.
Chris - So, in other words, we know the risk is there, we just have to be alert to the fact that it can happen and pick it up quickly.
Colin - Indeed. I mean, response is really the critical element here. So, there have been a number of Ebola outbreaks over the last 40 years. They've been contained long before they ever reached the stage, just because in general, when response is swift and effective, it's easy to contain an Ebola outbreak. But it's when response is slower than one would like, things can turn into the situation that we have right now.
Chris - But arguably, Suzie English [in an earlier interview] was saying, Ebola was first described in 1976. The world was a much more primitive place in terms of medicine, communications, population was lower then than we have today and it's today that it's escaped and caused a big problem. Why is that?
Colin - It's a complex situation where there was not a sufficiently rapid response to bring the situation under control to limit the early stages of the spread of the disease. Once the disease gets into its exponential growth phase whereby, two cases create four cases, create 16 cases, etc. then it becomes exponentially more difficult to contain as well. Because when the number of individuals who are infected is doubling, the number of resources that it takes to control that sort of outbreak is more like quadrupling or worse.
Chris - So, in terms of actually doing surveillance, you would argue then that what we need to do is be aware of the fact we've got this risk, be aware of the fact that, as populations grow and people have more likelihood of coming into contact with wild animals- do we need some kind of network around the world then where scientists like you are watching for warning signs that something might be about to happen so you can deploy the sort of rapid response you're saying we need?
Colin - There's a variety of types of response networks that are administered by WHO, by various national governments, that are meant to detect abnormal activity. But the difficulty that we face in a variety of low income countries is there's a real difficulty in differentiating normal from abnormal. And so, in a lot of place in west Africa, people go in to see a doctor because they feel sick and without even doing any kind of diagnostic test, they're told that they have malaria and that they should go back home. And yet, there's a number of different diseases that have malaria-like symptoms in their early days. So, in malaria endemic portions of Africa, this is not an unreasonable thing to assume. But it means that you're going to miss those extraordinary cases that have the potential to set off situations like the one that we have right now.
One of the things that we need on a really fundamental level is we need the development of basic public health infrastructure worldwide. And something that I find shocking is that every year, approximately 1.8 million people die of diarrhoea. Now, those people aren't by and large in the UK. They're typically in low income countries where the public health infrastructure is generally very weak. But if we were to develop - we, as high income nations - were to develop the basic public health infrastructure in low income countries so they could deal with diseases like diarrhoea, we'd stand a much better chance of being able to discriminate ordinary diseases from extraordinary diseases and being able to catch cases like the current Ebola outbreak while it's still early enough, well, we could really do something about it.
Chris - In other words, it's all about prediction.
Colin - It's all about our ability to respond swiftly when something happens...

40:43 - The Ebola threat for gorillas
The Ebola threat for gorillas
with Dr Peter Walsh, University of Cambridge
Alongside humans, gorillas can catch Ebola too. But unlike bats, who  don't get symptoms, gorillas get infected much the same way humans do. It's estimated that a third of gorillas have been wiped out by the deadly virus. Peter Walsh is a primate quantitative ecologist from Cambridge University, and he explained to Kat Arney what is happening to our primate cousins...
don't get symptoms, gorillas get infected much the same way humans do. It's estimated that a third of gorillas have been wiped out by the deadly virus. Peter Walsh is a primate quantitative ecologist from Cambridge University, and he explained to Kat Arney what is happening to our primate cousins...
Peter - Gorillas and chimps are our closest relatives and their immune systems are extremely similar to ours. And therefore, when a gorilla gets Ebola, it behaves pretty much the same way as it would if it was in you or me.
Kat - So, they're getting all the horrible fevers as we had described, the bleeding and all the kind of horrible stuff.
Peter - Absolutely, yeah. It's even worse for them because think about it- They're out in forest. There's no nurses. They don't get any water. they don't get protected from other animals. It's pretty horrific.
Kat - What do we know about how these wild chimp and gorilla populations are getting Ebola?
Peter - Best guess is that fruit bats eat fruit and gorillas eat fruit. So, they go to the tree and some bats have been there and left the virus in their body fluids, maybe saliva, maybe faeces, and they eat the fruit, and then they get infected.
Kat - How widespread is this problem? I mean, are we seeing animals being affected in the areas where the current outbreak is?
Peter - The biggest mortalities of gorillas and chimpanzees have been in central Africa which is quite away from these outbreaks. But there are chimpanzees in the area where that first index case that Suzy was talking about, it was in Guinea, in a remote area. Where this outbreak started was in the most forested area in west Africa and there are still some chimpanzees and other animals like monkeys out in that area.
Kat - So basically, we just don't know.
Peter - West Africa, we don't know. Central Africa, we have a pretty good idea. We have actual evidence where we have somebody who got sick and they told us, "Well, I ate a gorilla" and they went out found the carcass and they found the same virus in the gorilla carcass that the person had. So there, it's pretty well documented.
Kat - Is there anything that can be done? I mean, it does sound like this disease is decimating these wild primate populations?
Peter - Well, because our immune systems are so similar to gorilla or chimpanzee, it means that the vaccines that work on us, work on them too. Now, I actually led a captive chimpanzee vaccine trial with Ebola vaccine. Not one of the ones that you already talked about, but a different one. The vaccine didn't cause the chimpanzees any kind of the side effects and it caused a very robust immune response. Right now, I'm trying to gear up with some colleagues to go out and vaccinate gorillas in the wild.
Kat - That's going to be a bit tricky though, surely?
Peter - It turns out to be a lot easier than you think. it's easy for these...
Kat - You have to catch and stab them?
Peter - No, you don't have to catch them. We use a blowgun. So, you don't actually have to immobilize them. It's easy for the ones that are in the tourism programme, or a research programme. It's kind of fun. It's kind of scary. You get the silver back and you think - people were certain that the gorillas are going to kill us when we did it. We went out and did it with measles vaccine and they didn't hardly respond at all.
Kat - It's like, I don't even notice. It's like a mosquito bite or something I guess.
Peter - Yeah. Go and Google gorilla and teeth and you'll see, they bite each other all the time. that's a lot worse than a little needle.
Kat - I mean, we've mentioned that the fruit bats might be the reservoir for Ebola in the wild. Is there any way we can eradicate that? How do we go about trying to track down that reservoir?
Peter - It's going to sound like science fiction, but 50 years from now, it's going to be standard practice. It's what's called a self-disseminating vaccine. What it does is you take a different virus, you pull a little piece of Ebola in that other virus and then you give that virus to the bats and then it spreads within the bat population and immunizes the bats. There's research in other species on this self-disseminating vaccines going on right now. Eventually, that's the way we're going to handle wild life vaccines. Right now, the state of the art is oral vaccination. You put the vaccine to a bait. This have been very effective in Europe and almost eradicating fox rabies. You put baits out, the animals eat it and they get immunized. But that's the kind of thing that we could do.
Kat - When it comes to actual people rather than these chimps and gorillas, what are your feelings on the outbreak and how it's being handled?
Peter - What Colin was talking about is very true, if you don't respond quickly then you have a problem. In this case, sort of institutional rivals, international rivalries, it started in the French speaking country. The French don't like the Americans. The Americans had better capacity to do this sort of modelling thing. the World Health Organisation doesn't like the Centre for Disease Control from the United States. The reason this thing got out of control was that those national and international organisations could not play well together and they let it get out of control.
Kat - Do you have hope personally that it may get back under control?
Peter - Right now, I've been doing some projections. It's difficult to tell right now whether it's going to - Liberia has slowed down a little bit and is looking a little bit better but Sierra Leone and Guinea are still moving along. It's still a chance that we're going to have really, really nasty outbreak of the kills, up until about hundred thousand people or more, just unclear.
Kat - That's pretty terrifying vision of the future. So, I really hope that some of the vaccines and treatments that we've been talking about do come online soon. Are you hopeful for those as well?
Peter - I'm actually doing some modelling on how much it's going to take, how much vaccine it's going to take. It's looking like it just depends. If it really goes big then the vaccines are the only thing that's going to stop it. And they will be in production in large number of doses by about April to do that. If it attenuates then the vaccines are going to be too late.

46:20 - The world's reaction to Ebola
The world's reaction to Ebola
with Suzie English, Colin Russell and Peter Walsh, University of Cambridge
Every day there are new headlines about Ebola as the death toll rises. But do we in the West have a reason to fear Ebola? Are we doing enough to stop  disease outbreaks in the developing world?
disease outbreaks in the developing world?
Suzie English, Colin Russell and Peter Walsh, all from Cambridge University, discuss the likelihood of Ebola spreading, how health organisations work against disease outbreaks and the media's fascination with the virus.
Chris - Now, let's take a sort of broad view and ask everyone's opinion on this. Suzie, let's begin with you. What do you think actually the threat is in terms of a British or an Australian, a sort of western healthcare system? Do you think we're well-prepared?
Suzie - Well, we've had warning. We've been able to observe the outbreak occurring in west Africa. And I think that early warning is very important for us to be able to mobilise people in our own health system, both in public health, in hospitals, in GP practices to be aware of Ebola, to know what to look for, to know who's at risk of catching Ebola. These are really important for preventing an outbreak in Britain or Australia.
Chris - Peter, do you think that we are at risk of this thing spreading much more if it were to go in a toehold in a country like Britain? Would it spread or would it just fizzle out?
Peter - It's not going to spread in Britain or in Australia. As Suzie said, we have very good public health systems. It's not really that's transmissible. The flu which Colin studies is much, much more transmissible. It's relatively easy to contain if you know what to do and you have a public health service.
Chris - Colin, Peter is saying that many of these international organisations don't play well together. You're saying that in order for them to interact, if we're going to succeed and stop this and other kinds of outbreak like this in the future, they need to be playing well together. That doesn't sound like good news then.
Colin - For influenza for example, WHO and Centres for Disease Control (CDC) work very well together. But it's the lack of international coordination on a variety of different levels that ultimately creates problems. Coming up with this sort of ability to respond locally to outbreaks which is what we really need because international response is great. But if you're really going to catch on the first day or the second day, you really need people on the ground in each country who are ready to respond at a moment's notice. That's something that is not going to be necessarily developed by a big international organisation. But it's something we have to develop within these countries themselves.
Chris - Peter, what about other sorts of disorders which might be lurking out there because Ebola is just one of the many? What should we be doing to be more on our guard against those?
Peter - It's a resource allocation problem. Until they've killed a bunch of people, nobody is wanting to spend any money. What we really need to be doing is we need to do the research and surveillance but before the fact, nobody is willing to spend the money to do it. And so, it's a huge problem.
Chris - Colin, you're nodding.
Colin - I think the current situation really highlights a broader international problem that we have which is, until there's a lot of people dying in some other place and then there's a threat to us here in the UK or the United States or Australia, it's their problem. But we don't invest enough to develop that sort of very basic public health infrastructure to actually help them stop the problem before it becomes a potential problem for us.
Chris - So, why has there been such a media storm?
Colin - Always, as humans, we're attracted to things that are spectacular and extreme. In terms of horrific disease, Ebola is one of the worst that there is. We're not concerned that much about the things that actually kill us, like influenza for example. Approximately 500,000 people die of influenza every year, but we're so comfortable with what flu is and the fact that we've had it and didn't die from it, that we don't worry about it that much.
Chris - Peter...
Peter - I agree completely. Another contributing factor is zombie movies. People have gotten so used to these movies where like, you get one little splatter and then 30 seconds later it's a zombie. Everybody is a zombie and everybody is going to die, that they have come to think that's actual science rather than science fiction.
Chris - Don't come to the cinema with me. Not if you're going to wave your hands around like that. I mean people will give us funny looks. But no, it's true though. People do like a good story and they do like being professionally scared really. But it is important though. Someone was also highlighting to us, isn't it interesting that lots and lots of people have died in Africa of this for 40 years like Suzie is saying and it's when finally, someone dies in America that people go, "Oh, maybe we should take some notice of this"? Suzie...
Suzie - Absolutely. I agree with everything that my fellow speakers have said about the need for infrastructure in countries that are least able to cope.
Chris - So, following on from that then. We've got this question that's just popped up on social media. Does the media reaction actually affect how we respond? Colin, what do you think?
Colin - Well, indeed it does. There's a couple of different components to it. So, the short term is that a really strong media reaction can help facilitate the funding of a long term international response which is incredibly positive. However, one of the things that happens over time is that Ebola ceases to become news. So, if we look at the number of headlines that reported the word 'Ebola' over the past 3 months, they actually peaked in October and they've been declining ever since then. Because at this point, everyone knows there's a big outbreak going on in west Africa. So, it's not so much news anymore. We get fatigued from it. It's not that similar to the situation with influenza. H5N1 bird flu back in 2006, it was the big scary thing that was going to kill us all and there was a big threat. But it's not in the news anymore, but the threat itself hasn't changed. And so unfortunately, we, as humans, we get tired of hearing the same thing day after day and so, we have to hear new stories. One of the things that really needs to be balanced in terms of what the media does and how it covers the Ebola outbreak is to stimulate long term public interest.
Chris - Today, the Wellcome Trust have announced they're putting in one and a half million Pounds to fund a number of little start-up projects to try to come up with new sort of Ebola initiatives. You're nodding at that, Peter...
Peter - The director of the Wellcome Trust, Jeremy Farrar, was - if you can pick one person who was instrumental in actually creating reaction to this outbreak was he. He really shamed the international community into acting on this when everybody else was not doing anything. He's a hero for that.
Chris - Suzie, are you getting lots and lots of phone calls to the hospital from worried well? That's another way that people are reacting.
Suzie - We're getting so many calls from the worried well though I'm sure that GPs and hospital emergency departments undoubtedly will be seeing people who are very concerned about Ebola. The fear is real whether or not there is a true threat. That is something that health professionals have to deal with. Certainly, people who've been coming back from west Africa from treating people have encountered an awful lot of fear and that fear is real. So, we do have to be sensitive to what people think and the reaction that the media attention has generated. I'm hoping that this media attention will bring about changes including vaccines and treatments which will be a legacy that can be used to treat Ebola going into the future.
Chris - So, what do you think should be done right now?
Suzie - So, I'm very happy that the treatments and the vaccine trials are progressing more quickly. I think this is long overdue. Furthermore, a concern from the current outbreak is that Ebola virus will become endemic in west Africa when it hadn't previously been there before. And so, there may be more outbreaks going into the future and we desperately vaccines and treatments to combat these outbreaks.
Chris - Colin, I guess on your wish list would be better international surveillance and cooperation, wouldn't it?
Colin - Indeed and it's something we're going forwards from here. Hopefully, we'll be in a situation where we can end the current epidemic with no subsequent endemic circulation. But once this outbreak is over, that doesn't mean that the threat from Ebola is gone. It came from an environmental reservoir somewhere and that threat will persist over time. We have to find good ways to monitor it and we have to find better ways to respond next time.
Chris - Peter...
Peter - First of all, as Colin knows, I think we should be modelling bat populations. I think this is much more predictable than people will admit. I think that if - in 2005, colleagues and I published a paper saying that it was predictable and if you did X, monitor bat populations, you could predict it and had they done that, this might not have happened. And so, I think that there has to be some money invested. What I was going to say is that the media has to be much more intelligent about advocating things that are actually solutions rather than just crying about how dangerous things are. And they must be much more sophisticated, but understanding what's actually a good response and a constructive response and what's just inciting fear. That's what has not happened enough to date.

54:59 - Swallowed by a whale?
Swallowed by a whale?
Joanne - Hello, Naked Scientists. We're Joanne...
David - ...and David.
Joanne - From Dublin in Ireland. And we wanted to know what would happen if a scuba diver was swallowed by a toothed whale?
David - Would he be able to escape back up the oesophagus?
Joanne - Could the whale regurgitate the diver back up?
David - Would he be dissolved by the whale's digestive enzymes and if so, how long would it take to corrode the wetsuit?
Tim - To find out the answer, I zipped up my wetsuit and jumped off a pier into ocean of knowledge with animal anatomist, Joy Reidenberg. Now, we're floating about in the sea and I can see a few orcas. Joy, are we likely to get swallowed up?
Joy - Orcas just don't have big enough mouths to swallow a human. An orca's gape is only big enough to engulf a human's head, but not much more of the human's body. What's more is the opening of the throat is much smaller than the mouth. It's going to accommodate a large whole salmon perhaps even a human thigh, but nothing much larger. So, when an orca, accidentally swallowing a human especially when sporting a scuba tank is akin to saying, you accidentally swallowed a watermelon whole. It's just physically impossible.
Tim - Well, that's reassuring. But I can see a few bigger whales swimming around. What about those sperm whales?
Joy - Sperm whales are certainly bigger, but their throats are relatively small. However, a large adult may be big enough to swallow us and baleen whales certainly have a mouth big enough to engulf a human, but their throats are just not big enough to swallow one. But it's really unlikely that a toothed whale would even attempt to swallow a human. To date, there are no records of such an event happening. Rarely, humans have been killed by whales, but not accidentally eaten.
Tim - Now, let's take a look at the stomach of a whale. If we just shrink ourselves and slide down the oesophagus, what's going to happen to us?
Joy - The digestive enzymes of a killer whale have no problem digesting other mammals. And so, our human flesh will be just as easily digested.
Tim - Yeah, I can feel them eating away at my skin. Shouldn't the wetsuits protect us?
Joy - Well unfortunately, there are leaky gaps in our wetsuits which is why it's called a wetsuit. So, let's change to our dry suits.
Tim - Okay, done!
Joy - Wetsuits and dry suits are both made from the same artificial rubber used to make oil-resistant and acid-resistant protective gloves. And so, it wouldn't be digested by the stomach enzymes. But if a whale can't digest something then it'll try to pass it out.
Tim - Joy, there's a stomach rumbling. It's making me a bit nervous. Are we going to get thrown up?
Joy - Well, there's no record of orcas vomiting solid remains from their prey and I suspect it would be unlikely that they will throw us up.
Tim - Wonderful! Now, let's get out of here. With feet firmly on the ground, Joy decided to write us an article, all about being swallowed by whales which you can read at nakedscientists.com. next week, we will be answering this question from Paul Gen...
Paul - I was on an interminable flight from New York to Hong Kong a few days ago and I don't understand why airplane manufacturers aren't working on increasing the speed of air travel.
- Previous Insulin: Chemistry in its element
- Next Robots in Society









Comments
Add a comment