Superbugs and hospital acquired infections go under the microscope on this weeks Naked Scientists. We find out why Clostridium difficile has become such a problem, how to keep bacteria away from surfaces and see if there's a vaccine for MRSA on the horizon. Plus, we discover where fat cells hide out, why fungi fire spores at amazing speeds and how plant sugars can make perfect petrol. And in Kitchen Science, Ben and Dave launch a liver-powered rocket!
In this episode
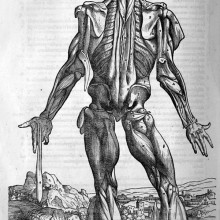
Stem Cells Muscle In
Scientists have shown that, contrary to prevailing wisdom, muscles contain stem cells that can repair, replace and strengthen injured tissue. Writing in Nature Stanford researcher Helen Blau and her colleagues have identified a collection of chemical markers that can be used to identify a population of muscle stem cells.
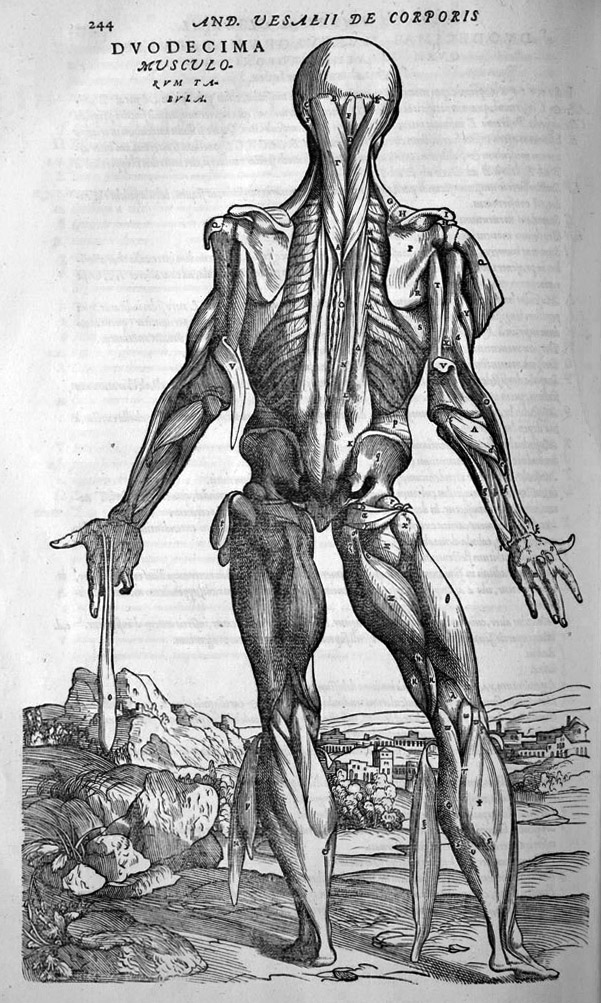 Dubbed "satellite cells" because these small round bodies usually loiter at the edges of muscles, when injected into an injured muscle they can rapidly begin to divide, producing more stem cells and new muscle tissue.
Dubbed "satellite cells" because these small round bodies usually loiter at the edges of muscles, when injected into an injured muscle they can rapidly begin to divide, producing more stem cells and new muscle tissue.
The team made the discovery by genetically labelling the cells with a coloured marker protein before injecting them into mice with damaged leg muscles. This technique enabled the researchers to follow the progress of the same mouse over a period of time by using a sensitive camera that could pick up the increasing intensity of the coloured stem cells as they grew.
"We were able to show that the injected cells increased their own numbers, contributed to existing muscle and also produced entirely new muscle in these mice," points out Blau. The results are very exciting because now researchers are able to readily identify the muscle stem cells they can turn their attention to discovering ways to activate them in people with muscle-wasting diseases, or use them to repair muscles in trauma patients.
"That's the next step," says Blau.

‘Baby’ Fat may Beat Obesity
It's something that many of us struggle with - fat. But where does it come from? Researchers in Dallas have finally tracked down the location of immature fat cells, which hide out waiting for the extra calories that turn them into flab.
For a while, researchers have suspected that immature fat cells, known as progenitors, were hiding in or around the blood vessels that feed fatty tissues, but their precise location wasn't known. Working with mice, the researchers engineered fat progenitor cells with a gene that makes them glow green, so they could be followed in the body. They discovered that the progenitor cells are embedded in the walls of blood vessels that run through fatty tissues, and are an integral part if the vessel wall.
The researchers think that the cells are there because it enables them to sense the levels of nutrients in the blood. When they get a whiff of excess calories, they can drift out of the blood vessels and mature into big fat cells.
The green label also meant that researchers could separate the immature fat cells from other cells, and grow them in the lab for further study. The team hopes that they will understand more about the mechanisms behind fat growth, which could lead to ways to cut obesity and metabolic diseases such as diabetes in the future.
As well as potentially helping people who struggle with their figure, the research could also point to ways to reactivate immature fat cells -for example, to fill in damaged tissues such as after injury or breast cancer surgery.
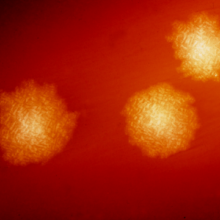
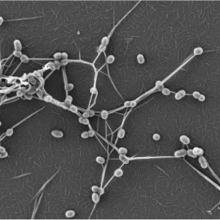
Fungi are world's fastest fliers
Scientists have discovered the fastest fliers in nature and, somewhat surprisingly, they're fungi!
 Ohio-based researcher Nicholas Money and his colleagues at Miami University made the discovery by using ultra-fast cameras capable of taking 250,000 frames per second. Down the lens they were studying members of two fungal families - the ascomycetes and the zygomycetes - that do the essential but unsalubrious job of breaking down animal dung. These fungi rely on their spores passing harmlessly through the guts of grazing animals so that they land, quite literally, in the remains of their lunch. But animals generally avoid grazing in areas where another animal has defaecated, leaving fungi like these with a problem. Their solution is to have evolved the mycological equivalent of a "super-soaker" squirt gun - they fire their spores from tiny fluid-filled fruiting bodies so that they land in patches of uncontaminated grass ready for the next browsing ruminant. But although scientists realised that the fungal launchpad must be incredibly powerful, it was too fast and too small to surrender its secrets, at least until now.
Ohio-based researcher Nicholas Money and his colleagues at Miami University made the discovery by using ultra-fast cameras capable of taking 250,000 frames per second. Down the lens they were studying members of two fungal families - the ascomycetes and the zygomycetes - that do the essential but unsalubrious job of breaking down animal dung. These fungi rely on their spores passing harmlessly through the guts of grazing animals so that they land, quite literally, in the remains of their lunch. But animals generally avoid grazing in areas where another animal has defaecated, leaving fungi like these with a problem. Their solution is to have evolved the mycological equivalent of a "super-soaker" squirt gun - they fire their spores from tiny fluid-filled fruiting bodies so that they land in patches of uncontaminated grass ready for the next browsing ruminant. But although scientists realised that the fungal launchpad must be incredibly powerful, it was too fast and too small to surrender its secrets, at least until now.
Writing in this weeks PLoS ONE the team have successfully made fungal ballistic measurements of spore trajectories to reveal that these organisms are firing their microscopic projectiles, which measure just a fraction of a millimetre across, at speeds exceeding 25 metres per second and at rates corresponding to 180,000 times the acceleration due to gravity. This is sufficient to propel the spores up to 2.5 metres away from the parent dung pile.
The team were also able to get a handle on how the organisms achieve their fungal feat. A concentrated mixture of sugars, alcohols and other metabolites inside the fungus and its fruiting body pulls in water by osmosis, priming the gun at a pressure about four times that of the atmosphere. At the right moment the structure ruptures and the pressure drives out the spores. According to the researchers the images of these fungal ejaculations are so pretty that they've set them to music and plan to post them on YouTube!

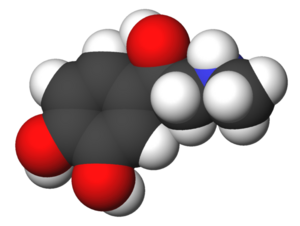
Plant Sugars Provide Petrol
We all know that the days of fossil fuels are limited, so researchers are trying to find alternative fuels. Biofuels have risen in popularity in recent years - fermenting plant material to make ethanol is already being used to produce fuel in several countries around the world. But ethanol is a long way, chemically speaking, from the petrol (or gasoline for our US listeners) and diesel that are currently used in car engines.
 The problem is that plant sugars have lots of oxygen atoms in them, which aren't found in fuels like gasoline. Now scientists at the University of Wisconsin-Madison have developed a biofuel that is identical, at the molecular level, to gasoline.
The problem is that plant sugars have lots of oxygen atoms in them, which aren't found in fuels like gasoline. Now scientists at the University of Wisconsin-Madison have developed a biofuel that is identical, at the molecular level, to gasoline.
Writing in the journal Science, the researchers have found a technique for turning complex plant sugars, called lignocellulose, into molecules that can be "upgraded" to make petrol, diesel and airplane fuel. They do this by turning the plant sugars into molecules with fewer oxygen atoms, which can then be converted into high octane gasoline.
To create the new fuels, the scientists add a solid catalyst to a solution of the plant sugars. After a reaction, an oil-like substance is produced, that can be skimmed off the top of the solution. In this oil are acids, alcohols, ketones and other molecules, which are the precursors to gasoline. They can then be used in further reactions to make gasoline.
This is a much more efficient way of using lignocellulose for biofuels than previous techniques - the oil created by the team retains around 90% of the energy content found in the original sugars. Although this technique is still at an experimental stage, it might be the key to solving the oil crisis in the future.

10:04 - Surprise Attack - Stopping Bacteria from Sensing your Immune Response
Surprise Attack - Stopping Bacteria from Sensing your Immune Response
with Vanessa Sperandio, Southwestern Medical Centre, University of Texas
Chris - Some bacterial infections, like E. coli 0157 which is a cause of food poisoning and can also damage your kidneys, seem to get a lot worse when you give patients antibiotics, instead of getting better. It seems that this is because the bacteria enter a sort of high-alert state in response to the treatment. They fight back by becoming a lot more virulent. Researchers at the Southwestern Medical Centre, University of Texas have come up with a drug that can stop the bacteria from sensing the chemicals in your body that tell the bacteria your body's gearing up to fight them. Dr Vanessa Sperandio is in Dallas and she joins us to tell us a bit about this research. Hello...
Vanessa - Hello Chris.
 Chris - How do bacteria home into the fact that we're on to them?
Chris - How do bacteria home into the fact that we're on to them?
Vanessa - They sense two stress hormones that you have: adrenaline and noradrenaline, and they use those two hormones as cues to know they are inside of you. When they sense that through a receptor in the bacteria they activate production of the virulence trait. By doing that they can actually make you sick and turn on everything that will cause disease.
Chris - It's intriguing to think that these bacteria are eaves-dropping on our own inflammatory signals. They've learned or evolved, I should say, to detect the signals our body uses to fight them.
Vanessa - Yes, and those are very primal types of signals. That's at the core of your immune system and it's the core of gauging how well - how healthy or not you really are and how stressed you are.
Chris - How did you get a handle on what the bacteria were doing and then try to work out how to stop them?
Vanessa - We figured out many years ago that they were using the signals and then in 2006 we were able to identify one of the bacterial receptors for this signal. What we've done now is to develop drugs that will bind to the bacteria receptors and prevent the receptors from seeing the host's stress hormones. In this way the bacteria passes blindly through the host without being able to know where it is and activate it virulence traits.
Chris - So you've managed to come up with a drug molecule that can block up the ability of the bacteria to see adrenaline or noradrenaline so the bacteria don't effectively know they're in the body.
Vanessa - Yes.
Chris - How could this molecule be used and is it safe?
Vanessa - So far the molecule is safe. Of course, this is in the lab of proof of principle. We did do some preliminary toxicology in mice and so far it looks to be safe. It also does not signal to human adrenergic receptors, which is important. It can be used either to treat infections or hopefully we want to try to use this to prevent infections.
 Chris - Which sorts of bacteria will be vulnerable to this? You've done tests on a number of different classes of bacteria but where do you see it actually being most useful?
Chris - Which sorts of bacteria will be vulnerable to this? You've done tests on a number of different classes of bacteria but where do you see it actually being most useful?
Vanessa - It can be very useful for something like E. coli 0157 which, right now, has no treatment. We also did look at this drug to treat salmonella infections which can cause gastroenteritis and typhoid fever. We looked into tularaemia which is a bioterror agent. In between these bacteria there are several important pathogens that have this sensor. This could be used hopefully to treat some of the communal infections especially for patients in ventilators. Bacteria like klebsiella, acinetobacter, pseudomonas who are important in this class of patient'swhich do not have a lot of treatments and antibiotics against and are quite resilient to the biotic treatments. They all posses this signalling system.
Chris - When do you think that we might be seeing this going into humans in clinical trials?
Vanessa - We've got money from the National Institute of Health to develop this drug to pre-clinical in five years which means in five years we want to be able to have everything pre-clinically, toxicology and safety done. Hopefully in five years we'll start the first safe trials in humans.
Chris - Thank you Vanessa.
22:02 - The Problem with Clostridium difficile
The Problem with Clostridium difficile
with Sani Aliyu, Addenbrookes Hospital
Chris - Dr Sani Aliyu is a consultant doctor at Addenbrooke's, one of Cambridge University's teaching hospitals. He's with us this evening. Hi, Sani. Welcome to The Naked Scientists.
Sani - Hello, Chris.
Chris - So C. difficile, what is it?
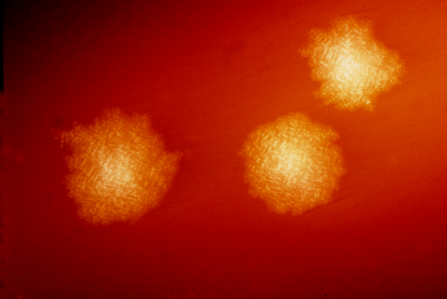
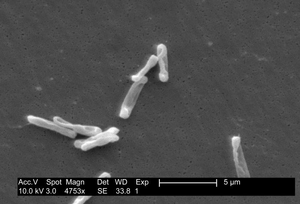 Sani - Clostridium difficile is a gram-positive anaerobic organism. By anaerobic I mean it doesn't really like oxygen. It produces spores. When it vegetates, in other words when it proliferates, it produces toxins that cause quite severe damage to the large bowel. Sometimes you can have patients coming in for one reason or the other end up on antibiotics and end up having this infection.
Sani - Clostridium difficile is a gram-positive anaerobic organism. By anaerobic I mean it doesn't really like oxygen. It produces spores. When it vegetates, in other words when it proliferates, it produces toxins that cause quite severe damage to the large bowel. Sometimes you can have patients coming in for one reason or the other end up on antibiotics and end up having this infection.
Chris - Where do we tend to get it then? Does everyone carry C. diff?
Sani - Well, no. As an organism it's quite ubiquitous. In other words it survives in the environment. The spores themselves are quite hardy organisms. You can acquire them from the normal environment as well as from domestic and animals and farm animals. More frequently it tends to be in hospitals because you have patients that already have this infection and they're producing a lot of the organism and are contaminating the environment. Patients can easily pick up the infection from that. Is it just gut infections it causes or can it also get to other bits of the body?
Sani - Well, predominantly gut infections what happens is the gut produces a lot of inflammation within the gut. As a result it can result in quite severe damage to the bowel, perforation, dehydration, severe diarrhoea and subsequently end-organ damage: including death.
Chris - Because it's triggering diarrhoea I presume it's so easy for it to spread because it's making people go to the toilet a lot. Every time they go to the loo they're shedding more of these tiny spores into the environment and that makes it very hard to treat.
Sani - Absolutely. Patients with diarrhoea can excrete as much as up to a million bacteria per gram of faeces. It can be quite profuse, really.
Chris - Once you've got the spores coming out into say, a hospital ward or a toilet how do you get rid of them?
Sani - Predominantly by good cleaning, really. The spores themselves are quite hardy organisms. We know that they respond - they are quite sensitive to chlorine-based products. Using alcohol, for instance - alcohol gel - in hospitals wouldn't get rid of the spores.
Chris - Why is it mainly old people who tend to suffer with this? Why is it people our age - I know that as a percentage of the population there's fewer of us lot in hospitals - but when you look at people in hospitals the proportion of old people getting C. diff is usually higher. Is that just because they're more vulnerable anyway?
 Sani - Yes. As you get older your normal immune system really doesn't work that well. As a result it means when you acquire the organism, when you ingest the organism, as a young person your immune system will probably be able to keep the immune system at bay. At the same time we know about the concept of colonisation resistance. In other words you have bacteria in the large bowel that tend to protect you against acquiring the organism. As you get older this resistance isn't really as good as it should be.
Sani - Yes. As you get older your normal immune system really doesn't work that well. As a result it means when you acquire the organism, when you ingest the organism, as a young person your immune system will probably be able to keep the immune system at bay. At the same time we know about the concept of colonisation resistance. In other words you have bacteria in the large bowel that tend to protect you against acquiring the organism. As you get older this resistance isn't really as good as it should be.
Chris - In other words your body's own bacteria effectively take up the available space. There's nowhere for the C. diff to fit in. If you kill those bacteria with a dose of antibiotics or just because that bacterial flora changes with age anyway it makes openings or niches that C. diff can then get into more easily?
Sani - Yes. In fact the normal bowel flora as we call it prevents the overgrowth with C. difficile by depriving the organism of micronutrients which means it can't establish an infection.
Chris - In terms of why it's such a problem now, because ten years ago it was a few cases, now we've got 7000 deaths a year. Why'sthe graph going up exponentially like that? What's happening?
Sani - It's partly due to improved reporting. Over the last few years we've put in place mandatory reporting processes which means that if you have a case of C. difficile you have to report it. The testing has also changed. In the past we used to test in individuals that are over the age of 65 but nowadays anybody having diarrhoea above the age of two. You have a more virulent that first emerged in Canada about 5 years ago and has since occupied the niche that used to be occupied by the more sensitive strains.
Chris - When you say more virulent what do you mean by that?
Sani - More virulent in terms of producing more toxin, causing more diarrhoea, causing more illness and probably more deaths as well.
Chris - Do we know why this has come about? Is it just because it was a random mutation? It just appeared and because it was so much more prolific in terms of its production of diarrhoea and its ability to spread that it just went all over the world?
Sani - I think it's fairly different from other strains of Clostridium difficile in that it has a deletion in the gene. There's a gene that negatively regulates toxin production. This particular ribotype called the autosomal ribotype has a deletion in that gene which means it can produce much more toxin and it can germinate for a longer period of time than other ribotypes of Clostridium difficile. Therefore you tend to have more spread as well, more environmental contamination as a result of a more severe disease.
Chris - What can we do about it?
Sani - In the first place we can restrict antibiotic use. A lot of times we use a lot of antibiotics in the community as well as in hospitals that we probably don't really need. That's one. Secondly, by improving cleaning and making sure that you interrupt the transmission process from patient to patient either by washing our hands, isolating patients promptly, putting them inside rooms, avoiding contamination of hospital equipment - that will go a very long way to reduce the infection.
Chris - Lastly, how long do you think it's going to take before we get a handle on this problem and can bring it under control?
Sani - I think we will. It might take another -being on the optimistic side - another five years. There are new things coming up like vaccines which we hope will probably reduce the incidence of infection. We're having new agents as well coming in which at the moment look quite promising.

29:25 - Keeping Bacteria Off Surfaces
Keeping Bacteria Off Surfaces
with Professor Joanna Verran, Manchester Metropolitan University
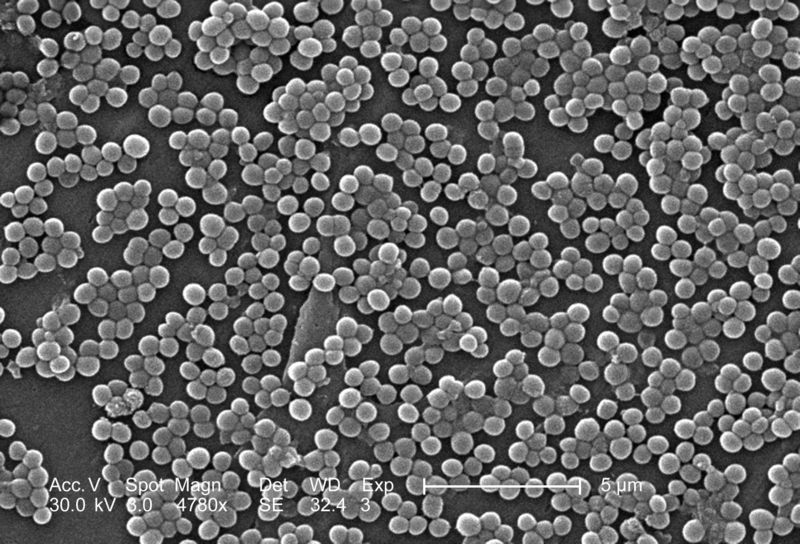
Kat - Whether or not bacteria stick around in your local hospital isn't always down to local conditions or cleaning. Sometimes it's the microscopic structure of the surface you're cleaning that dictates whether you'll manage to get the bugs off. If we can understand better how bacteria stick to surfaces we could make food factories, bathrooms, kitchens and hospitals much cleaner. A team at Manchester Metropolitan University have been looking into this. Professor Joanna Verran joins us now. Hello. Why is a wipe down with a bit of bleach not enough to get rid of bacteria?
Joanna - I think if you think of the surfaces that you're wiping they may well not be particularly smooth so the bugs can get wedged in defects and scratches. It's not so easy to get them off that way.
Kat - These surfaces, how big are the scratches? Most surfaces look fairly smooth. What size are we talking about?
 Joanna - A typical bacterium, a cockle bacterium, is about 1µm (1000th of a millimetre). The sorts of scratches that we're looking at are around about that sort of size. Sometimes if the scratches are huge the bacteria come out fairly easily because they've got nowhere to stick. If they can wedge their little bums in the scratches then it means that they're holding on and it's harder to get them out.
Joanna - A typical bacterium, a cockle bacterium, is about 1µm (1000th of a millimetre). The sorts of scratches that we're looking at are around about that sort of size. Sometimes if the scratches are huge the bacteria come out fairly easily because they've got nowhere to stick. If they can wedge their little bums in the scratches then it means that they're holding on and it's harder to get them out.
Kat - Is there a difference in the types of surfaces? Surfaces can be made of all sorts of things. Are there any that are particularly hard for bacteria that you've found?
Joanna - I think softer surfaces, ones which scratch more easily are going to get more rough and therefore get harder to clean but hygienic surfaces like stainless steel are actually quite hard. They don't scratch particularly badly. What we've shown actually is if stainless steel surfaces wear it doesn't really make it harder to get the bugs off of those. Part of the problem with them as well is that food material and other material gets stuck in the cracks too. Again it helps the surfaces retain soil and that helps the bacteria stick to them. It's not just trying to get the bugs off, it's actually making sure that you get all the organic material off as well.
Kat - I know that one of the things you're really interested in is titanium. Tell me about titanium and how you're trying to use it to fight off bacteria.
Joanna - There's one aspect of titanium that is nanotitanium. This isn't so much on our hygienic surfaces but it's a photo-catalyst. As you've been talking about earlier with reactive molecules, nanotitanium is very small particles of titanium dioxide. When light shines on it, it activates the titanium dioxide and particles are released from the surface. These particles react with things like oxygen and form extra active super oxide molecules. They hit the bacteria and start to break down bacteria. These active molecules can also break down organic compounds as well so they are called photo-active surfaces, light activated.
Kat - So they're essentially self-cleaning?
Joanna - That's right. There are quite a few self-cleaning surfaces with nanotitanium in them already. There are glass and lots of ceramic tiles but we were looking at paint formulations particularly. We were interested in seeing whether we could get paint formulations that you could just paint indoors which would be activated by fluorescent light. We were looking at E. coli actually, Escherichia coli - not 0157.
Kat - I know that many paints already have titanium dioxide in. Is that special or do paints not normally work in this way?
Joanna - Titanium has got different functions. Some of the larger titanium particles are just pigment so it's white. Titanium dioxide is often used in paints and cosmetics, toothpastes but we're looking at the nanotitanium because those smaller molecules are better photo-catalysts.
Kat - Would that be very expensive though? It sounds like a fantastic idea if you can paint this paint indoors. It's activated by normal fluorescent lights. Is it going to be too pricy to be practical?
Joanna - I don't really know what the prices might be. We've started looking - we looked particularly as E. coli and the reason that we started with E. coli is because that's where standard tests for testing how good these antibacterial properties are. You would want to then look at other micro-organisms as well and see whether you've got a broader spectrum of activity. I'm afraid I don't know anything about the prices of them.
Kat - Brilliant, maybe that's something to look into.
Should we sterilize footwear in hospitals?
Sani - When you look at the issue of contamination in hospitals and transferral of organism particularly in relation to C. difficile we know that most of the contamination comes from patients that are already infected with the infection, with the disease, with the organism. The crucial thing really is to make sure that you clean the surfaces. You clean the sites where you touch quite frequently by healthcare workers. You also isolate the patient who's symptomatic. It's less of an issue in terms of people bringing it in. You're not going to bring it in from the community on your footwear, for instance.
Will soap work against superbugs?
Sani - Ordinary soap will help because you are trying to reduce the burden of infection on your hands. Ordinary soap will help in terms of C. difficile. We know even when you finish washing your hands this is talking outside of the C. difficile spectrum (in terms of MRSA infection, for instance) if you use that hand gel - if you haven't really washed your hand and you have a lot of debris that alcohol hand gel is not going to work. Yes, using soap and water is definitely a good thing.
Chris - There's a physical detachment of organisms by placing your hands with friction under running water. We know that helps to knock them off.
Could laudanum treat superbugs?
Chris - That's a morphine-based drug. The basis of that I presume is it treated the symptoms rather than the cause so it probably would make C. diff worse, wouldn't it?
Sani - Absolutely. With C. difficile you really want the toxin and the bacteria out of your system. You don't really want to give a drug to help the toxin stay in and cause more damage. Chris - That toxin, how does it work? Why is it bad for your guts?
Sani - The toxin works by inducing quite an intense inflammation. Clostridium difficile produces two types of toxins: toxin A and toxin B. These latch on to receptors and simulate production of inflammatory mediators called cytokines and this causes quite an intense inflammation with cell death and subsequent necrosis and breakdown of the normal barrier that you find in the large bowel. Chris - That presumably means you'll not only lose fluid from the body but you may also an access point for other nasty bacteria to get in as well. Sani - Yes, and you might actually perforate your bowel.
37:35 - A Vaccine for MRSA
A Vaccine for MRSA
with Gerald Pier, Harvard Medical School
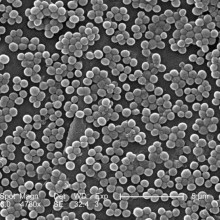
Gerry - The major work has been on infections caused by bacteria. We focussed on two specific types: Staphylococcus aureus (of which one form is MRSA) and another organism called Pseudomonas aeruginosa which is a quite common organism. It's found in water but fortunately only in certain situation does it really cause a bad infection.
Chris - Why is Staph and MRSA such a problem?
 Gerry - It's a little bit difficult to say why it has become a bigger problem recently. Some of the issues seem to be greater exposure. More people seem to be carrying MRSA. It's basically for years and years was pretty much only found in people in the hospital. Now it's clearly out in people in the community. It's spreading more.
Gerry - It's a little bit difficult to say why it has become a bigger problem recently. Some of the issues seem to be greater exposure. More people seem to be carrying MRSA. It's basically for years and years was pretty much only found in people in the hospital. Now it's clearly out in people in the community. It's spreading more.
Chris - How many people have got it?
Gerry - About 30% of people are carry Staphylococcus aureus in their nose. A smaller percentage - maybe around 2-5% carry MRSA. That's more than it used to be. Even though that sounds like a small number when you think of all the people out there it's really a large number of people overall.
Chris - What are you doing to try and stop that?
Gerry - One of the factors that has been very useful in making vaccines has been to extract the materials that bacteria put out on their outer surface. That allows us to immunise individuals and get immune responses, usually antibodies, that can cause the bacteria to be killed. We've discovered that there is a specific type of surface material that's actually a sugar molecule. Scientists call it a polysaccharide that if we chemically change it somewhat it causes a very good immune response. Those antibodies are then capable of killing the Staph and preventing infections or perhaps limiting infections so that they don't become as severe.
Chris - What you're saying is that people who don't have this vaccine - there's something about the surface of the Staph that stops you making an immune response normally.
Gerry - Correct. It turns out that one of the ways that bacteria avoid causing an immune response that would kill them is to trick your body into making the wrong kinds of antibodies. The bacteria don't care you don't have those antibodies because they don't harm the bacteria. Our job has been to try and figure out how to get the right kinds of antibodies that will kill the bacteria.
Chris - Do you know how they fought the immune system in that way?
Gerry - It's a little bit complicated because it involves looking at this very detailed structure of this sugar molecule that coats the bacteria. In general what we find is that the sugar molecule has projections from the sides and those projections are involved in causing the non-killing or bad antibodies to form. Those antibodies bind to the bacteria ok but they don't cause other factors of the immune system to stick to the bacteria. These other factors are essential for killing. It's the structure of this sugar molecule overall that gets the wrong kinds of antibodies mostly made. What we've done is we've changed the structure so we get antibodies that then bring in these other factors that are needed to kill the bacteria.
Chris - So you're just injecting people not with bacteria but with chemicals from the surface of the bacteria that drive this response?
Gerry - So far we've only injected mice, rabbits and monkeys. Although we're fortunate that there is movement towards making this into a human vaccine, optimistically we'd hope perhaps within two or three years we'll see our first humans immunised with this material. It's going in the right direction but so far we only have data from animals.
Chris - Will the same chemical trick work on other infections because it's not just Staph that make us ill, is it?
Gerry - We're fairly optimistic that is the case. We've shown with our laboratory studies that the same vaccine can be effective against E. coli which is also another common cause of infections in a hospital. The bacteria that causes whooping cough also makes this. The organism that causes plague makes it. There's a lot of other organisms that have become quite problematic in the hospital setting because they're very resistant to the antibiotic drugs that we commonly use to treat infections. In some cases we don't have any antibiotics at all. We're hoping our vaccine or perhaps antibodies we make in the lab might be effective against these microbes as well.
Chris - Do you think there's any risk that the bacteria could, once you start treating large numbers of people with this, could become resistant? Bacteria change very rapidly. They've become resistant to lots of antibiotics. Could they thwart your vaccine?
Gerry - This is always a possibility. What one tries to do when you make a vaccine is to make it our of something that the organism has to have. If it stops making it then it no longer causes infections. In our laboratory studies we've shown that if staphylococcus doesn't make this material it's much less able to cause an infection. We're hoping that'll be the case but we're still a ways away from knowing that with any certainty.
Why do bacteria stick so well to plastic surfaces?
Joanna Verran - If you don't mind I'll have to go back a little bit and talk about bugs on surfaces generally.
Bacteria generally on the planet live attached onto surfaces. Most of them are attached onto surfaces so it's where they would rather be. If you had bacteria in your mouth, if you swallow them they die but if they stick to your teeth it's much better for them. It's the best place for them to be attached to a surface. They'll stick to lots of different surfaces.
In the food industry and where we've been talking about surfaces in hospitals you're just looking at survival of organisms that have stuck onto the surfaces. Perhaps they've been put there by people touching them or with the chopping board they've come into contact with a surface through the meat or whatever it is that's been chopped. That's a sort of contact and survival. The organisms haven't attached. They've just been put there and then they're surviving. We call that attachment at a solid air interface.
If you allow the organisms to grow in a surface that's got liquid in it at a solid liquid interface we call that a biofilm. Again, although organisms are very happy to do that they'll stick onto a surface and then grow. In a roundabout way they'll stick on to anything really and it's trying to reduce their ability to stick.
The other thing with biofilms - if you think about catheters or contact lenses or dentures - any sort of plastic that you might implant in the body. The first thing that will stick to those materials is organic molecules from the liquid around them. It might be saliva or tear fluid or urinary proteins. Then the bacteria will stick to those. The biofilm will form on top of that conditioned surface too.
Will MRSA develop further resistance?
Sani - Really bacteria are quite clever as we all know. The issue is provided we keep on developing new antibiotics we'll be a step ahead of the organism. I don't believe we should just stay back and say, 'They're probably winning anyway. Let's leave them.'
Chris - The numbers of MRSA are going down, aren't they? Sani - Yes. It's partly because of intervention measures that have come in over the last few years. We're putting less intravascular devices in nowadays where we're taking much more care when putting in plastic devices. At the first sign of any infection these plastic devices are taken out. It's probably the main reason why catheter-related blood stream infections, particularly MRSA, have gone down.










Comments
Add a comment