This week, we investigate infertility and In-Vitro Fertilization (IVF). We find out how a new high resolution temperature monitor conceived in Cambridge can help couples get pregnant, and explore new ways to improve the success of fertility treatment. Plus, a new extra-fast and super-cheap way to sequence the human genome, the science of eating slowly, and fish dining out at the Shark Cafe. Also, we find out how newborns cry with an accent and examine the inner workings of an egg...
In this episode

Gobbling your food could make you overeat
If your mother ever told you not to eat your food too quickly it turns out she was probably onto something. Scientists have discovered that when people eat slowly, more appetite suppressing hormones are released than if they quickly scoff their food. This makes slow eaters less likely that they will want to keep on eating and eventually overeat.
 The team from Imperial College in London and Athens University Medical School in Greece published this study in the Journal of Clinical Endocrinology & Metabolism. They recruited a group of volunteers, who were asked not to eat anything for 10 hours, then come into the lab and eat 300ml of ice cream - a good bowl-full. On two separate occasions, they were asked to eat the ice cream either in 5 minutes, or to nibble at it slowly over half an hour by dividing them into smaller portions that were taken out of the freezer every 5 minutes.
The team from Imperial College in London and Athens University Medical School in Greece published this study in the Journal of Clinical Endocrinology & Metabolism. They recruited a group of volunteers, who were asked not to eat anything for 10 hours, then come into the lab and eat 300ml of ice cream - a good bowl-full. On two separate occasions, they were asked to eat the ice cream either in 5 minutes, or to nibble at it slowly over half an hour by dividing them into smaller portions that were taken out of the freezer every 5 minutes.
Before the experiment began and then for the following three hours, the levels of blood hormones in the volunteers were measured, called ghrelin, PYY and glucagon-like peptide, or GLP-1. These are produced in the gastrointestinal tract in response to food being eaten and all act on a part of the brain called the hypothalamus and are known to play an important regulatory role in mediating feelings of hunger and fullness and so effect the amount of energy intake.
The volunteers were also asked standardized questions about how full or hungry they felt at different points during the study.
Levels of the two hormones, PYY and GLP-1 were both higher in the volunteers who ate slowly, compared to the fast eaters. So, it seems when you eat more slowly, your guts are better at telling your brain that it's time to stop eating.
And the slow eaters all reported feeling much more full after eating their ice cream than the gobblers.
Other past studies have suggested a link between fast eating a body weight in adults and children so now this study has provided the first evidence for the link between the two.
So, perhaps it pays to listen to you mother, and we could all benefit from enjoying eating our food slowly rather than wolfing it right down.
Low cost genomics
As we discover more genes that make us susceptible to developing certain disease or reacting the wrong way to certain drugs, the race is on to come up with very fast systems that can read DNA sequences and at very low-cost.
 It's fair to say that prices have come down a bit since the 100 million US dollar spend that was required to complete the official human genome project, but US $2000 to do the same thing seems almost unbelievably cheap. But that's roughly the price quoted in a paper published in the journal Science from a California-based company called Complete Genomics, who have developed an ingenious method of sequencing genetic material very quickly and very accurately.
It's fair to say that prices have come down a bit since the 100 million US dollar spend that was required to complete the official human genome project, but US $2000 to do the same thing seems almost unbelievably cheap. But that's roughly the price quoted in a paper published in the journal Science from a California-based company called Complete Genomics, who have developed an ingenious method of sequencing genetic material very quickly and very accurately.
Their teachnique involves first cutting DNA into short segments about 400 genetic letters long and then linking small numbers of the segments together using special "adapter" sequences, which are artificial pieces of DNA containing a specific sequence of genetic bases.
The result is a collection, known as a library, of small circular DNA molecules representing the entire genome. Next, a single strand of the DNA is copied using an enzyme called Phi29 polymerase, which generates long coils of DNA called "nanobundles". One billion of these nanobundles are then dotted individually across a special chip about the size of a microscope slide. The surface of the chip is prepared in such a way that it binds to the nanobundles, locking them in place.
Then, to read the DNA sequence, a series of special colour-coded probes are added to the slide. These contain sequences that recognise and bind to the adapter DNA and to the adjacent genomic DNA. When a probe matches one of the genetic letters in the genome it lights up and is "read" by a laser before being washed off and the process repeated to read the next letter.
In this way, one by one, different probes are used to interrogate the DNA sequence letter by letter. This process is repeated many times to read the DNA sequences in the millions of nanobundles. As this is going on, a computer programme is logs the emerging genetic messages and working out which bits overlap with which to piece back together the complete genome.
The result is a highly accurate genome sequence that can be produced rapidly and cheaply.
The team have checked the technique by sequencing three human genomes. According to Cliff Reid, the CEO of Complete Genomics, "We've demonstrated that it's possible to accurately and affordably sequence and detect variants across entire human genomes.
This high-quality, cost-effective approach to genome sequencing will allow researchers to study complete genomes from hundreds of patients with a disease to advance the understanding of the genetic causes of that disease, with an end to preventing and treating common human ailments." Dennis Ballinger, vice president of Complete Genomics, also highlighted the speed and cost effectiveness of the platform. "The nearest competitor to what we're doing currently costs $40,000 per genome and takes 8 weeks. That's twenty times more expensive and 8 times as long as us."

Hanging out at the shark café
Scientists have come a step closer to understanding the mysterious lives of some of the oceans biggest predators - the Great White Sharks - in a 10-year study that tracked nearly 200 sharks as they swim around the eastern Pacific Ocean.
Published by the Royal Society in their Series B journal, the study by a big team of researchers led by Salvador Jorgensen from Stanford University in the US unpicked some great white secrets, including pinpointing their favourite mid-ocean hang out: a spot of sea between Hawaii and the Californian coast nicknamed the shark 'Café'.
The team used a combination of cutting edge satellite tagging technology, acoustic tags that are detected by sensors placed around the Pacific Ocean and DNA analysis of samples taken from wild sharks
Jorgensen and the team discovered that every winter the sharks regularly migrate away from coastal waters off California and head out 4000 km to the warm waters of Hawaii, before heading east again the following summer.
The big question is, why do great white sharks bother swimming so far every year, backwards and forwards, using up so much energy?
And the answer - unfortunately - is that we don't really know. But, researchers think the sharks are probably visiting Hawaii every year to feed since the tags showed the sharks regularly diving down deep probably hunting for prey.
And as for the mid-ocean shark café? It's likely that the great white sharks are feeding and also mating there too. The tagging studies showed males and females mingling in the shark café, at around the right time ahead of females giving birth in likely nursery grounds in coastal waters further east. Great white females gestate foetuses for 12 or possibly even 18 months before they give birth.
The study also revealed that sharks keep on returning to the same area of coastal habitat off the American coast. It's possible that sharks hunt more successfully when they know the area well.
The study also showed that great white sharks in the northeast Pacific are a distinct population from other sharks in Australia and South Africa. This is vital information for conservationists, because even if many people are still scared of these toothy predators they are, sadly, facing an uncertain future because of overfishing. Their large fins are highly prized for the trade in sharks fin soup.
Studies like these are revealing vital details about the lives of great whites, highlighting that they are not simply mindless killing machines milling around aimlessly, but they undergo complex migration that we are only just beginning to understand.

12:51 - Babies are born with their mother's accent
Babies are born with their mother's accent
with Dr Kathleen Wermke, University Hospital of Wurzburg
Chris - Scientists at the University of Wurzburg in Germany have teamed up with their colleagues in Leipzig and also in Paris and they found that the cries that young newborn babies emit actually mirror their mother's accents. And to tell us how they discovered that, we are joined now by Kathleen Wermke who is the head of the Centre for Pre-speech Development and Development Disorders and she's at the University Hospital of Wurzburg. Hello, Kathleen.
Kathleen - Hello!
Chris - Welcome to the Naked Scientists.
Kathleen - Thank you.
Chris - What's this study actually show?
 Kathleen - The study actually showed an extremely early impact of the surrounding language, of native language, a foetus was exposed to in the womb. This is, of course, new because we knew since many researchers and investigators that during the last year, that infants are sensitive to prosodic features of the native language long before they are born and that they memorize those patterns as a newborn. But it was not known that they are capable so early also, not only to memorize, but also to reproduce those patterns in their own cries.
Kathleen - The study actually showed an extremely early impact of the surrounding language, of native language, a foetus was exposed to in the womb. This is, of course, new because we knew since many researchers and investigators that during the last year, that infants are sensitive to prosodic features of the native language long before they are born and that they memorize those patterns as a newborn. But it was not known that they are capable so early also, not only to memorize, but also to reproduce those patterns in their own cries.
Chris - How did you do the study?
Kathleen - We recorded the cries of the newborns in Paris and in Berlin in Germany, and then we came back to our laboratory acoustic lab, and we analysed the frequency, spectrogram and the melody contours of the cries, normalized cry time - because not every cry has the same duration - and then we looked for what time point the pitch maximum, the melody maximum was reached. Was that more at the beginning or more at the end of a cry? So we compared between the groups of German and French infants according to their melody contour, having either rising or falling contour.
Chris - Shall we have a listen to some of them?
Kathleen - Okay.
Chris - Well, you sent us some of the recordings you made. So first of all, I'll play the rising cry.
Newborn's Rising Cry
Chris - And here's a falling cry.
Newborn's Falling Cry
Chris - So that's basically one that goes down at the end rather than going up as it goes along. How does that mirror the native language spoken by the mothers of those babies?
Kathleen - It mirrors it because French intonation is characterized by a pitch rise towards the end of several kinds of prosodic units, words or phrases; whereas German, typically, exhibits a falling melody contour.
Chris - And so, why do you think that the babies, when they've got a lot going on in their lives when they're newborns, why should they prioritize being able to mimic mum in this way? Why does this give them benefit?
Kathleen - We think that this observed behaviour is just simply a reflection of the special aptitude human infants have to acquire language. They're hard-wired to acquire language and we know that they have a special sensitivity from melodies and rhythms already being a foetus and then also being born. So we think this is just showing how early language development starts in human infants based on their brain mechanisms and genetic programs, really to acquire language.
Chris - Is this language that they're acquiring in utero? So while they're inside mum and towards the end of pregnancy, they're listening to the sounds and vibrations from her voice being transmitted to them while they're inside and that's where they learn to mimic before they've even been born?
Kathleen - Yeah. That's what we guessed because they are able to listen for three months at least being in the womb and they had only one or two days after delivery. But, of course, we're not sure. Maybe these one or two days after delivery were enough to learn the specific intonation patterns of their surrounding language. We are not sure but we guess that most important are the three months prenatally.
Chris - And in animals?
Kathleen - In animals, it is well known that they have already a lot of prenatal auditive learning. But I'm not sure if anybody checked already the postnatal - the very, very early postnatal impacts of those prenatal learning processes but I'm sure it should be observable in animals too.
Chris - One of the things you say in your paper is that if the baby sounds like mum, she's more likely to bond with it. That seems reasonable.
Kathleen - Probably, yeah. Of course, we don't know but according to the theoretical implication of this study and other studies, it might be that this really fosters bonding between the newborn and the mother, but it seems to be rather unintentional - being just a reflection of the capabilities this human infant has from his genetic programmes and behaviour mechanisms.
Chris - We must leave it there. Thank you very much, Kathleen. That was Kathleen Wermke who's at the University of Wurzburg. She was explaining how babies perceive the general tone of their native language and mimic it even before they're born.

18:08 - Temperature Tips to Conception
Temperature Tips to Conception
with Oriane Chausiaux & Shamus Husheer, Cambridge Temperature Concepts
Chris - Now most people have probably heard the claim that body temperature changes when women ovulate. But can this be actually used as an effective fertility aid? Well, there are a couple of scientists here in Cambridge. They are Doctors Oriane Chausiaux and Shamus Husheer and they're from a relatively new Cambridge-based start-up company. It's called Cambridge Temperature Concepts and they say that temperature can be used to do that and they've come up with a way to measure it. Welcome to both of you. Good to have you with us.
Guests - Hello, Chris.
Chris - Hello. So Oriane, let's talk to you first. If you could, just tell us what's the situation with temperature and the menstrual cycle? How does it change?
 Oriane - So early in the cycle, a woman's temperature would be quite low but just after ovulation, her body will release an hormone thats called progesterone and that hormone has an effect on body temperature, it makes it rise and thats the - that rise of temperature - that we are detecting with our fertility monitor.
Oriane - So early in the cycle, a woman's temperature would be quite low but just after ovulation, her body will release an hormone thats called progesterone and that hormone has an effect on body temperature, it makes it rise and thats the - that rise of temperature - that we are detecting with our fertility monitor.
Chris - Why do you think the temperature changes in this way? Anyway, what's the benefit of that actually happening? Why should these hormones have those effects? Do we know?
Oriane - They have an effect on the blood vessels that are located near the skin and that is the reason why temperature changes. Now, I don't know if there's a benefit to it or not, but that's the situation.
Chris - Is that why when women are pregnant, they tend to get a glow. They get this sort of chloasma is the name, isn't it? They tend to get a sort of glowing face and also, the neck tends to be more red. I've heard this is because of enhanced blood flow.
Oriane - Yes. That's quite possible indeed.
Chris - So, when you say temperature is low or temperature is high, how high and how low are we talking?
Oriane - The difference between low and high can be as little as 0.3 of a degree...
Chris - Degrees C?
Oriane - Yeah, degrees C and can be as high as 1.5, depending on the woman.
Chris - And so, just talk us through the menstrual cycle then what's happening to various points and how you would go about using that to predict on the basis of temperature, what stage of the cycle the woman at?
Oriane - So if we take a textbook cycle, which is 28 days - obviously, that isn't the case for most people, but let's stick with that for now - and the first 14 days is when the temperature is low and that's when the body is getting some follicles ready for ovulation.
Chris - This is in the ovaries where you're maturing future eggs.
Oriane - Yes, that's the case and then one of the follicles, will be ready to release an egg and that's the time of ovulation. Just after ovulation occurs, the body will start secreting progesterone for the following 14 days and that will allow the body to get ready for potentially fertilized egg to implant and that would be the start of pregnancy.
Now, if pregnancy doesn't occur, temperature will go low again because progesterone will drop at the time of the period.
Chris - And so your proposal is that, if you measure body temperature very accurately, you could potentially predict when that ovulation is. Why is it helpful to know that?
Oriane - So the highest chance to get pregnant for a couple are the days around ovulation and most couples don't know when that happens. And so allowing them to have that information increases their chance of conception by about three times so that's what we found that's very useful to provide them with that information.
Chris - Now, you've used what you called a very artificial menstrual cycle 28 days. You said most people are, I mean, most women are a little bit longer than that, aren't they? But what about many women who have irregular periods?
Oriane - Yes.
Chris - Does the temperature work there?
Oriane - It would. You have some information that you can use, some patterns that are specific. It happens just before ovulation. You some time have a little dip of temperature just before hand. But it's quite specific woman to woman so the monitor that we've designed, the DuoFertility monitor, will actually learn from the temperature patterns from a specific woman and use that cycle after cycle to help her find out when she's most fertile.
Chris - So, basically, what you're doing is you're building up a profile of that person's temperature and how it probably relates to their fertile window. So that with the machine learning, you learn from experience and you can now begin give information to that person about when it's probably a good time.
Oriane - That's completely correct. The other advantage we have is the device connects to the internet and so the data of one cycle can be compared to the one of all the other users who is using the product, which increase the accuracy by a lot.
Chris - Wow, you can actually sum data from a very big population of users to extract trends. So, actually, this is not just a sort of personal tool for the users. It's actually a research tool as well in that respect.
Oriane - Yeah, completely.
Chris - So the company is learning.
Oriane - We are.
Chris - How many people are taking part? It seems like a good time to ask Shamus because you're actually the guy who - you did a lot of the engineering on this.
Shamus - Yeah. I'm the inventor of the little sensor that collects all the data. To answer your question, we did a trial throughout the EU of about a 100 couples between December and May of this year. That gave us our, sort of, initial database of ovulation cycles to look at and there are several hundred units in the field right now collecting data and calling back home and depositing that data with us.
 Chris - What do people say, how do people react to the fact that you're basically logging their menstrual cycles? I mean, obviously, it's an interesting thing and they can probably see the benefit for others. But do people feel a little bit tetchy about the fact that their own personal body rhythms are being beamed off over the internet to your company?
Chris - What do people say, how do people react to the fact that you're basically logging their menstrual cycles? I mean, obviously, it's an interesting thing and they can probably see the benefit for others. But do people feel a little bit tetchy about the fact that their own personal body rhythms are being beamed off over the internet to your company?
Shamus - To be honest, we haven't had that single person being concerned about that because one of the key benefits is that that data can be flagged up, if there's anything unusual going on. And our in-house fertility experts can look up that data and then come back to them with a question say, "Were you ill last Tuesday?" Or if not then, you know, this is the peak of your cycle in most way. Perhaps you could talk to your doctor about this interesting feature.
Chris - That's interesting. So if they get swine flu, which many people probably are, you're probably going to record that as well, aren't you?
Shamus - We haven't built alghorhythms to detect swine flu due to a dearth of data on our database for swine flu but in the event that we have thousands of people calling saying that's what they've got then, in theory we could develop ourselves if it's a swine flu detecter on the back of it.
Chris - But if someone does have a feverish -a fever-related illness anything that causes the temperature to go up, that presumably is going to mask an effect that you would be able to see that month.
Shamus - It changes the temperature but it changes in a very different way than ovulation does. When you get a fever, the change tends to be very rapid and very much greater than the change due to menstruation. And of course, it doesn't happen around the same time as the other indicators that we're looking for, suggesting that ovulation might, unless you're incredibly unlucky and you get a fever on the day of ovulation. So it's usually very easy to spot the difference between some other sources of temperature change.
Chris - So there's basically a thermal fingerprint or a thermal profile that goes with ovulation and you can dissect that out with the other background thermal data that you're recovering so you can still be relatively accurate no matter what.
Shamus - That is the essentially the heart of the algorithms that we run. Yeah.
Chris - Now, this is the first time today I've seen your unit and I have to say this is amazing. I'll just describe this to the people at home. If you imagine a mouse that you could operate on your computer with, it's about palm size and there are two colours, pink and blue. I presume they don't actually discriminate between the sexes.
Shamus - We've actually found that people seem to prefer, actually, the non-gender specific colours of white, lavender and green.
Chris - This is accompanied by a tiny thing which - it looks like a miniature bath plug but it would be about a half the size of the bath plug. What actually is this?
Shamus - It's about 25 millimetres wide and 5 millimetres thick. It's the sensor itself. Now that's worn under the arm and worn with an adhesive to keep it there continuously. What that device does is it measures temperature very, very precisely. It actually got two temperature sensors inside, across a non-thermal barrier.
What that allows us to do is measure not only the temperature but the heat flow. So if you're under the blankets in bed and it's warm on your skin surface that would be a different heat flow than if the blankets weren't there. The amount of heat leaving your body would be different. That allows us to measure the core temperature very well while you're sleeping. It also contains a movement detector so that we can tell when you're sleeping compared to when you're awake because you really want -
Chris - Presumably, the accuracy and the precision of measurement during sleep is much less variable and therefore, well, the temperature is less variable therefore your measurements are more accurate.
Shamus - And the physiological thing that you're trying to measure is the deep sleep temperature. So what we're doing is automatically detecting when you're asleep when your body's in a good thermal environment and then making corrections for all the external changes that could be going on so we can get a good handle on what's going on internally.
Chris - And how does the tiny sensor tell the mouse size based station which is presumably the thing that then collects all data.
Shamus - Yeah. So -
Chris - How do you talk to each other?
Shamus - What you've got is - the device has a single button and little track wheel sort of like a little consumer electronic devices, iPods and things we have today. What you do is you simply turn the device on by holding down your middle button, hold that down and will then start looking for the sensor. You bring it close to the device and it reads out the data.
Chris - It's a radio link...
Shamus - So it's a wireless radio link and so it doesn't emit any radio while it's being worn. The radio link is actually from the handheld radio to the sensor. What that does is it downloads all of that data and performs statistical analysis on it in the background.
Chris - So how do I then see that data?
Shamus - So after it's finished reading out, it will give you a display, indicating your fertile days for the prediction in advance. So it has a one indicator that says that what's today's level is and the brightness of each day segment tells you how likely you are to conceive. Now that takes into account both the male factors for the couple which may change the likelihood of conception before ovulation and female factors, which may change the likelihood of conception after ovulation.
Chris - And how does the data get to you? Because obviously this is not a computer, this is a handheld device. How does it connect to the internet to tell you about the temperature profile?
Shamus - Yeah. So in the side of the device, you'll spot a small USB connection like you have in cameras and things like that. You plug that into your PC. And then it looks as though that the world like a flash disk. Like one of those little USB thumb drives. That contains some PC software that you can run, which will show you a historical display of all of your data and your future prediction for up to six days in advance, which is what the monitor displays as well. Most importantly it will then connect to our servers over the web, transfer that data and allow us to perform a correlation between your data and as we say, all the other women using the system.
So we find those women with similar cycle pattern to yours. If you have a very stable cycle, there will be a group of women there that share a very stable, similar cycles to you. If you have a condition like say, polycystic ovarian syndrome which is about one-third of women who have infertility difficulties or very irregular cycles, it will find other woman with similar hormonal responses to ovulation to the size of that temperature change and cycling variability. And we'll bundle up those people that are similar to you and use that information to improve the predictions on the reader for you, put you in particular.
Chris - Thank you, Shamus. And just quickly Oriane, this has obviously been on the market now for a little while, what is the data look like? Is it successful? Is it working?
Oriane - The data is quite successful so far. And early on, especially during the trial we had a couple who had great problems, infertility problems and we have been able to help quite a few of them to increase their understanding of their cycle and a few of them managed to get pregnant as well in a short period of time so we're very pleased with that.
Chris - Thank you very much to both of you.
31:09 - In Vitro Fertilization
In Vitro Fertilization
with Julian Norman-Taylor, Chelsea and Westminster Hospital
Now to explain a bit more about the process of IVF and why some people need it, we're joined now by Julian Norman-Taylor. Now he's a consultant gynaecologist at the Chelsea and Westminster Hospital in London and he also runs IVFChelsea. Hello, Julian.
Julian - Good evening.
Helen - Hi. Thanks for joining us at The Naked Scientists. Now to start us off, could you perhaps describe to us what happens when someone's referred to see you because they're having problems with their infertility? How do you approach that case and start to work out what the problems are?
 Julian - Well, we take a full history from them and there's a couple of things we want to check out first before we get to the fertility aspects and that would be their general health. Are they diabetic or have any other problems and are they generally fit and ready for pregnancy? Importantly, have they been immunized to rubella and are they taking their folic acid vitamins? But beyond that, we start taking a history directly related to fertility.
Julian - Well, we take a full history from them and there's a couple of things we want to check out first before we get to the fertility aspects and that would be their general health. Are they diabetic or have any other problems and are they generally fit and ready for pregnancy? Importantly, have they been immunized to rubella and are they taking their folic acid vitamins? But beyond that, we start taking a history directly related to fertility.
So the obvious thing is, are they in a relationship where fertility is possible? It's not all that unusual for people to come and see me and they actually don't live in the same country, which obviously presents the problems.
But beyond that, we're looking really to see if the lady is making some eggs, whether the chap has some sperm and whether the anatomy is in correct functioning order. And so to do that, we take a full history from the woman and the most important thing really would be her age and the regularity of her menstrual cycle. So a woman with a regular menstrual cycle is generally ovulating okay and quite often they've done little tests such as one from your previous contributor where they measure their temperature or check the urine for hormones to see if they are indeed ovulating.
Helen - So the problems often will come down to a lack of eggs or something going wrong with the sperm? I suppose it has to be one or two of those things, hasn't it?
Julian - Or besides where the anatomy of the female is incorrect. That's right.
Helen - And what we're looking at is the common causes for some of these problems. What sort of things do you see going wrong?
Julian - Well, it divides up roughly equal to about a quarter of the patients have some sort of ovulation problem, a quarter have some sort of male factor, others has some anatomical problem and then another significant proportion - we never actually get to find out what the problem is and that's group called unexplained infertility.
Helen - So there's still quite a big question mark covering over some people who just aren't able to conceive?
Julian - Yes. Clearly, there is a problem but as I say to the patients it's not that the problem doesn't exist. It's just that we as scientists and doctors can't work it out yet.
Helen - You haven't yet got the answers to that one. Now how many people in general does this tend to affect - this problem of general infertility?
Julian - Well, the oft quoted figure is one in seven couples will consult a doctor. Though not quite that many would actually require treatment but it's a remarkably common thing and numerous people will know people who've had treatment.
Helen - Yes. We all hear about an IVF - in vitro fertilization - as one of the possibilities we have for treating infertility. What's going on with that? What happens when a couple goes to have that treatment?
Julian - Well, that's - is a very common treatment and it's usually when the fallopian tubes have been damaged, most commonly by Chlamydia or something called endometriosis and other common reason is the male factor - the sperm just aren't so strong.
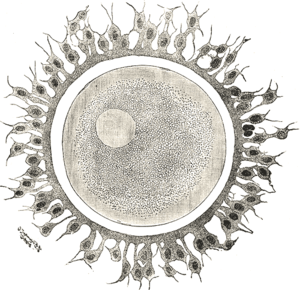
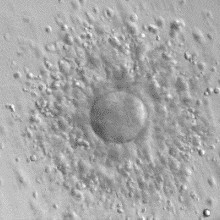
And what we do there is the hormone that drives the ovaries, it's called FSH or follicle-stimulating hormone and when a period begins, we give the patient or give the woman some extra FSH. And so, instead of just the one egg they would normally grow, over a period of 11 days or so and they end up growing maybe 8 or 10. And that's monitored by ultrasound and then we do a small procedure where we put a needle into each of the follicles that have grown in the ovary and suck the eggs out and we have those in the lab. Then the gentleman produces a sperm sample, we fertilize the eggs in the lab and then, hey presto, with any luck, 48 hours later, we have some embryos and we put one or sometimes two of those back into the female.
Helen - And is there any effect on the health of the babies conceived this way with IVF or is it from that point onwards? Is it just the same as the natural pregnancy?
Julian - More or less, there's a particular type of fertilization called ICSI or intracytoplasmic sperm injection where there is a male factor problem and we take a single sperm and inject that directly into the egg and therefore bypassing all the natural selection procedures you might imagine that would happen. And for years, we did worry that's ICSI children would come out as somehow abnormal. There's a very reassuring though there's a small increase in abnormalities in those children.
Helen - What success rate do you have with IVF these days as presumably been going on for quite a while? How likely is this going to help someone?
Julian - I'm afraid it's very much an age-related question so if you happen to have a simple problem like your tubes are blocked and you're age 28, you have a very good chance of conception per cycle - more than 60%. Once you get over 35, that's dropping significantly and then over 40 and only perhaps 10% of people will get pregnant and over 45, it doesn't work unfortunately.
Helen - So it really is a case of time on that one. Well, thank you very much, Julian, for getting us into the basics of what's going on in infertility and the use of IVF. That was Julian Norman-Taylor. He's a consultant gynaecologist at the Chelsea and Westminster Hospital in London.
37:10 - Improving IVF
Improving IVF
with Professor Alison Murdoch, Newcastle Fertility Centre
Meera Senthilingam went along to meet Alison Murdoch who is the Professor of Reproductive Medicine at Newcastle Fertility Centre where she's been working ways to improve the chances of IVF actually working.
Alison - You have to start really from where IVF began. The first IVF treatment, it was over 30 years ago now and although it has improved, it's not made it a treatment that is going to be guaranteeing that every single woman who comes along is going to achieve a pregnancy. We're now expecting about a quarter of people who have one go at IVF to become pregnant. If women come along when they're a lot older, when their eggs are no longer of good quality, I'm afraid there's very little that we can do to help. But there's a lot that we can do, I think, to try and improve the techniques for IVF that we have at the present time.
Meera - So what are some of the limitations with regard to the IVF treatment itself when it comes to the creation of embryos or the health of the embryos?
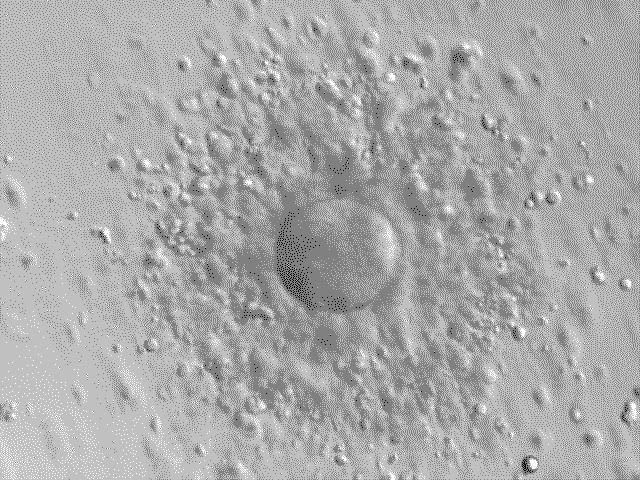 Alison - I think there's a lot that we can do to try and improve the way that embryos are actually grown within the laboratory. The standard techniques in the laboratory really haven't changed over the past 30 years. They involve handling embryos on a small dish, looking at them in a microscope, and then walking across the room with them putting them back into the incubator. Now obviously, potentially, the embryo is going to be harmed by being cooled as you walk across the room. Traditionally, people have said it's impossible to do it any other way. But the embryologists led by Mary Herbert in Newcastle have actually worked very hard at this and found that it is possible to provide an isolator system. That means basically, when the sperm that goes into an enclosed cabinet at the beginning of the IVF procedure, all the manipulation that are done, the checking of the embryo, the checking of the fertilization, the ICSI procedures, are all done within an enclosed system. So, that the embryo that comes out two days later has never been in contact with the air at all. It means that we can control its environment totally.
Alison - I think there's a lot that we can do to try and improve the way that embryos are actually grown within the laboratory. The standard techniques in the laboratory really haven't changed over the past 30 years. They involve handling embryos on a small dish, looking at them in a microscope, and then walking across the room with them putting them back into the incubator. Now obviously, potentially, the embryo is going to be harmed by being cooled as you walk across the room. Traditionally, people have said it's impossible to do it any other way. But the embryologists led by Mary Herbert in Newcastle have actually worked very hard at this and found that it is possible to provide an isolator system. That means basically, when the sperm that goes into an enclosed cabinet at the beginning of the IVF procedure, all the manipulation that are done, the checking of the embryo, the checking of the fertilization, the ICSI procedures, are all done within an enclosed system. So, that the embryo that comes out two days later has never been in contact with the air at all. It means that we can control its environment totally.
Meera - So, how does this new technology work exactly? So what are the various stages of it? And what are the conditions that you're controlling during this?
Alison - The core part of the conventional technology is an incubator that where the embryos grow for most of the time and a workstation where we do the manipulation, the insemination and checking the embryos. Conventional technology as these two are separated - in the new isolated technology, they're actually directly joined to each other so you can move from the working area directly to the incubator and directly back into the working area again. That means that the air in which the embryo is growing is constant. It never changes. It doesn't matter what's happening in the outside air. It will stay exactly the same. So we can control the temperature, we can control the gas concentration that's in the media. We can make sure that it's absolutely clean at all times.
Theoretically, that might make better embryos and the results that we've had because we've been working with this technology now for over 18 months, does seem to suggest that we'll likely to get better embryos because we're getting more pregnancies.
Meera - So, what is the temperature then that you operate at? And what are these gases that you're controlling? And how are these benefiting the growth of the embryo?
 Alison - Normal body temperature would be 36 to 37 degrees. We did some experiments in the conventional system where you put a little micro probe to measure the temperature within the dish while it's sitting under the microscope. Under those circumstances, it's on the heated block and there's heated air, but there's a cooling effect. And within two or three minutes, the fluid that those embryos are lying in will cool down to maybe 32 degrees, that's very cold for body temperature. That's why embryologists have to work really quickly when they're looking at the embryos. They want them out with as little time as possible and get them back. That doesn't give them time to spend the time looking carefully at the embryos to grade them more accurately. So, by controlling the temperature the whole time, they can take as long as they want to make sure that they got - they're doing exactly the absolutely the right thing for the embryo.
Alison - Normal body temperature would be 36 to 37 degrees. We did some experiments in the conventional system where you put a little micro probe to measure the temperature within the dish while it's sitting under the microscope. Under those circumstances, it's on the heated block and there's heated air, but there's a cooling effect. And within two or three minutes, the fluid that those embryos are lying in will cool down to maybe 32 degrees, that's very cold for body temperature. That's why embryologists have to work really quickly when they're looking at the embryos. They want them out with as little time as possible and get them back. That doesn't give them time to spend the time looking carefully at the embryos to grade them more accurately. So, by controlling the temperature the whole time, they can take as long as they want to make sure that they got - they're doing exactly the absolutely the right thing for the embryo.
Meera - And now you mentioned also that the gas concentrations are controlled, so which gases are controlled? And what effect can this have on the embryo growth?
Alison - All gases are controlled. We need to make sure, first of all, that the carbon dioxide level is accurate. This is because the acidity in fluid is controlled by carbon dioxide. And if we have the wrong concentration of carbon dioxide, the fluid that the embryos are in can become too acid and can harm them. We also need to make sure the oxygen tension is right. In the body, the oxygen concentration might be about 5% whereas, in the air, it's 20%. We really don't know what harm that change would have in culturing embryos. But within an enclosed system we kind, of course, control that precisely and make absolutely sure that we have as near body concentration as possible.
Meera - There must be, I mean, there's obviously a slight exposure to the natural environment between having made these embryos and then implanting into the women but I assume that's a very small gap then and that will be accounted for too.
Alison - Yes, obviously, when the embryo comes out of the incubators for it to finally to go back into the patient, it's got to happen that way. What we do though is we put the embryos into a very fine catheter. The embryologist is sitting next to the patient. It's handed to the doctor or the nurse to put back into the patient and it literally will take a few seconds as it crosses the room. So I don't think that's an area we could do much about.
Meera - And so, how much is this technology in use at the moment so, and is it likely to expand and be used in more clinics?
Alison - Well, it's still is very new and ours is the is the first system but there are other units now in Europe as well who are buying and investing in it. I think this is the way it will go because, intuitively, it has to be better. If you had an embryo, your embryo, would you want it to be subjected to the external environment or would you want it to be in an enclosed system where you can control it completely? And any embryologist would say, it has to be theoretically better. It's early days to see the impact on the quality of the embryos and pregnancy rates. We'll publish the data when we've got it completed.
Chris -Alison Murdoch who's from the Newcastle Fertility Centre and she was talking to Meera Senthilingam at the fertility show in London earlier this week.
Can temperature change the sex of an embryo?
We put this to Oriane from Cambridge Temperature Concepts:Oriane - No. I've never heard of that for a woman, unfortunately but sorry.Chris: - It would be quite good if they would though. There'd be all these people putting their women in the freezer or in the oven according to what they wanted, wouldn't they?Shamus: - That wouldn't be good.
How does monitoring temperature in the 21st century differ to methods of the 80s?
We put this to Shamus Husheer from Cambridge Temperature ConceptsShamus - That's exactly the same technique that my parents used to have me. It was very common on the 70s and 80s. But unfortunately, it's not highly prescribed to everyone. The DuoFertility monitor, which we've created, ensures primarily that you have no missed measurements which can cause the data to be uninterpretable. And it's much more reliable because it measures up to 20,000 temperatures per night and your movement to get the sleeping temperature because when you wake up, the body changes in temperature very rapidly.So if you change the time that you measure, you can introduce a lot of noise on that data. That means if you're one of these women with a 0.3-degree temperature change on your cycle, you can completely lose that. If you're lucky enough to have a one and a half degree change in your cycle, you're probably going to be okay. So it comes down to the accuracy measurement in the noise and also the statistical analysis of that data, rather than waiting for three days after ovulation to determine that you have seen the rise using the old method. We can spot that within a day, which means the egg is still alive, and you still have time to conceive that cycle.

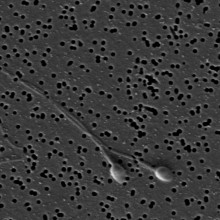
How fast do sperm swim and how do they find the egg?
Chris - Well the answer is about 5 mm per minute, and it's in fact, five body lengths of the sperm per second.
So if you scaled them up to the size of a salmon, that would be the equivalent of the salmon swimming along at 500 miles an hour, or a whale doing 15,000 miles an hour.*
So the sperm are pretty snappy. They get to the egg pretty fast, certainly within a day or so.
How do they find the egg? They recognise it by two means: one is a thermal gradient. They follow temperature so they know that the body gets warmer the further in they go. So they follow the thermal gradient. The second is that the egg oozes out various attractive molecules, in the same way that various inflammatory things attract the immune system in. This pulls the sperm towards the egg because they follow their noses, quite literally...
[*Thank you to the visitor who pointed out that this is a slight exaggeration!]
Is having identical twins hereditary?
We put this to Oriane from Cambridge Temperature Concepts:Oriane: - Well, there's not much information about identical twins being something you can pass on generation from generation. However, if your mum has a non-identical twin, then your chances of having twins are quite increased as well.Chris: - Why is that?Oriane - Why is that? The first one is identical twins which results from one sperm meeting the egg and then the egg dividing into two embryos instead of just one as would occur normally. In the case of non-identical twins, you'll have the two eggs that are produced and each meets a separate sperm, and that is something that can be passed on generation to generation.
What happens to sperm that isn't ejaculated?
Chris - This is a very good question; healthy testes make sperm at the rate of between 1000 and 5000 sperm cells per second. These collect in a long coil of tubes above and behind each testicle called the epididymis, where they are stored until needed. The testes hang external to the body within the scrotum to achieve an optimal temperature for sperm production. This is because sperm are made most efficiently at a slightly lower temperature than body temperature.
In the epididymis the sperm are nourished and make their way to the vas deferens, which is a muscular tube connecting the testis to the urethra up inside the male body. When sperm are ejaculated they are pushed along the vas deferens by rhythmic contractions of the musculature. Once inside the body, secretions from the prostate gland and seminal vesicles are added, producing the semen that is ejaculated from the penis.
However, although they can survive there for quite a long period within the male anatomy, a fraction of the sperm that are made are never ejaculated. Instead, they will senesce and are broken down. And of course all the things that you take into your body, cigarette smoke, other toxins and things will damage the sperm potentially. So they have a sort of recycle time. And sperm that have reached their sell-by-date get broken down in the same way that, let's say, blood cells get broken down. And, basically, any of the nutrients and goodies in the sperm just get recycled back inside the body, and new sperm are produced to make up for the shortage.
Helen: - So it's a kind of continual, sort of, replacement, really...?
Chris: - Exactly. Those that don't leave the body eventually break down, and their components are recycled.
Do pregnant women smell different?
Chris - I think that you could probably make a case. What do you think, Oriane? I think you can probably make a case that you could detect pregnancy on the basis of smell because, say mosquitoes, they could be aligned for women who are pregnant. That could be for a number of reasons. One of them is that women who are pregnant have a higher metabolic rate so they breathe more.Oriane: - They also have a higher temperature.Chris: - Yeah.Oriane: - Due to the high progesterone during pregnancy.Chris: - So it could be either of those things.Oriane - Yeah.Chris: - But if they're having a higher temperature, they're probable exuding more volatile chemicals so they probably where have a slight different smell signature. The mosquitoes can definitely home in on them. So I think probably you could train a dog in the same way that dogs can be trained to discriminate urine from people who have renal and bloody cancers, on the basis of the volatile chemicals that the cancer puts into the urine. Dogs can pick that up. I reckon you probably could train a dog, something with a very sensitive nose, on, say, a woman's urine, or on a woman's sweat in order to tell whether she's pregnant on the basis of a slight shift in the metabolism of that pregnant person.Helen - An interesting form of sniffer dogs, definitely.
What are the risks of sterilisation?
Chris: - Okay. So these are methods of sterilisation. Tubal ligation means that you go inside the peritoneal cavity in the woman, in the pelvis. You identify the fallopian tube on each side. You can see that quite easily because they're about 5 mm across, and you clamp them. You put a very large paper clip which is squashed onto the tube, and it crunches the tube closed. And the idea of that is that then what it does is basically squashes the tubes so that the egg released by the ovary cannot make its way down the tube to get into the uterus. And at the same time, a sperm cannot get along the tube to meet the egg and fertilize it. Otherwise, you might get the risk of what's called an ectopic pregnancy, the actual egg starting to be fertilized and grow outside the uterus.The risks of tubal ligation are that it doesn't work. It's a small risk but there's nonetheless a risk that you could fail to completely close off the pathway. Another possibility with any invasive procedure is, of course, that you can cause pain. You could cause bleeding. You could get a localized infection.With vasectomy, it's a very safe procedure, pretty similar though. You basically are cutting, folding back on themselves and tying off the vas deferens, which are the tubes that carry sperm from the testicle up inside the body. The idea being that then you interrupt the route that the sperm will follow after the testes. The risks are pretty similar to having tubal ligation and the fact is that occasionally there is incomplete severance. There may be a route by which sperm can still make it through. Also, you don't stop being fertile. The minute you have it done there's a flush out or a washout period afterwards.And so if someone just has a vasectomy and then assumes they're now no longer capable of fathering children, they could be in for a shock.Helen: - And presumably the same question that we had before comes up here that sperm - oh and the testicles that, if it's not got any way of getting out, it just stays there: but also is broken down over time if it's not actually released.Chris: - Yeah, you don't end up with your testicles expanding pervasively.Helen: - I did always wonder about that, actually.Chris: - With all the trapped sperm that's, sort of, left stuck there. Unfortunately, no it doesn't happen. Thankfully, I suppose. (Laughing) In fact, it's just basically broken down and those cellular constituents get recycled.

58:48 - How many children does a sperm donor father?
How many children does a sperm donor father?
We put this to Wendy Kramer, Co-founder and Director of the Donor Sibling Registry:Well, the answer to that is a little bit tricky because nobody keeps track. What we do know is that the guidelines here in the US are supposed to be that only 25 pregnancies per 800,000 of a population area should be allowed for each donor. So that would mean that what they would like to do is limit each donor to 380 children. But the bottom line is, the sperm banking industry doesn't keep track. They don't have accurate record keeping. So they really don't know how many kids are born from any one donor.For instance, we have one donor on our site that says they donated two times a week for two and a half years. And this is pretty common. Each one of his donations turned into approximately 10 to 15 vials. So he produced over 3000 vials during that time. So just for that one donor, 3000 vials were sent out. But we don't know many children were born from those 3000. You could say, maybe up to 3000, but we don't know. What we do know is that on our website we have very large groups of half-siblings. They're people born from the same donor. Many in their 20s, 30s, 40s, 50s, with the largest group that we know being just over 125.










Comments
Add a comment