Chimp Viruses Vaccinate Against Hepatitis C
Interview with
Chris - Two papers were published this week in the journal Science Translational Medicine discussing a promising new vaccine for hepatitis C. Now this is a virus that spreads from blood to blood contact and in over 80% of people who contract it, it sets up a persistent lifelong infection that progressively damages the liver and leads to cirrhosis and in some people, liver cancer. Now over 170 million people are infected with this worldwide and at the moment, there is no effective vaccine.
But now, scientists may have found a way to protect people by adding parts of the hepatitis C virus to a harmless cold virus called an adenovirus that actually normally infects chimpanzees. This modified virus triggers the immune system to mount a strong response against hepatitis C and that can prevent a person from developing a chronic infection if they're exposed to the virus for real at a later date. Ben Valsler spoke to Oxford University's Professor Paul Klennerman about the work.
Paul - The specialty of hep-C is that it sets up chronic infection in humans. So, even if you've got a relatively intact immune system, you don't seem to normally be able to mount an immune response that gets rid of the virus. If people do become chronically infected, some people handle that pretty well and in fact, they have very little inflammation in the liver which is the major consequence. But some people have much more inflammation in the liver and as a consequence, much more scarring on the liver tissue and so over time, they can develop end-stage liver disease, so cirrhosis and also liver cancer. It's turned out to be one of the main reasons people need transplantation in this country and in the western world. Having said that, the other interesting feature of hep-C is that a fraction of people end up clearing the virus on their own. That was actually very attractive from the point of view of a vaccine since we already know there's some form of immunity which is efficient.
Ben - What sorts of target have we been looking at for actually making a 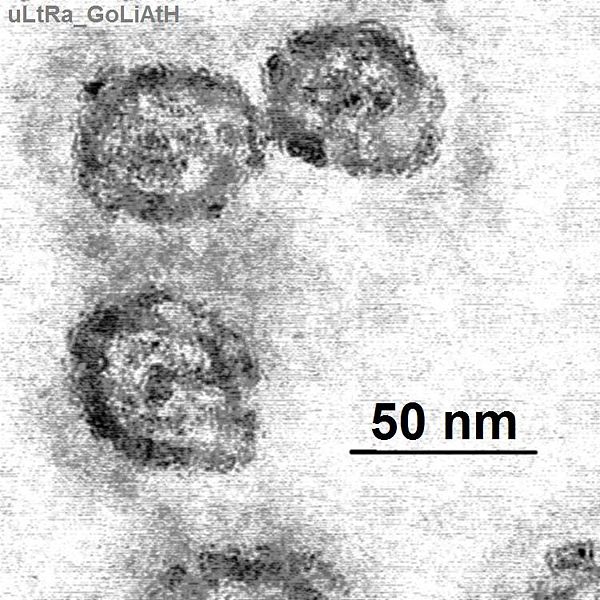 vaccine?
vaccine?
Paul - Broadly, the way you might think about making a vaccine is to make either an antibody response or a cellular immune response, so that's mounting a white cell response that targets the infected cells directly. The problem with hep-C in terms of antibody response is that the envelope of the virus is quite variable. So the alternative approach is to try and target the virus as it's replicating within cells and that really relies on mounting a T-lymphocyte response.
The T-cells will actually look at proteins which are generated during the process of viral infection, so that can be proteins which are part of the machinery of viral replication. If the T-cell really can recognise those cells, it will secrete chemicals, cytokines, which are directly anti-viral and will limit the viral infection and they can also kill the infected cells, so actually destroy the virus within it.
Ben - What are you now doing to target that and where are your "weapons" coming from?
Paul - The trick seems to be to stitch in the bit that you want - in our case, as I said, the internal proteins of hep-C - into something that's really going to get the immune responses fully activated. In our case, we've used an adenovirus. This combination of using an adenovirus with the hep-C internal proteins seems to produce very strong immune responses of the type that we see in people who naturally clear the infections.
Ben - Aren't we already immune primed against adenoviruses?
Paul - Yeah, that's a very good point. So I think one of the reasons adenoviruses are good is that the body is very used to seeing them, but exactly for the same reason, we already have immunity. So, we've gone for an approach using vectors which people won't have seen before or at least will have rarely have seen. So one of these is a human adenovirus, but just a rarer strain, and the other is a completely novel vector which comes from a virus found in a chimpanzee.
Ben - What sorts of results are you seeing? Are you actually getting the immune response that you expect?
Paul - There were two interesting bits of the trial. We exceeded our expectations with the priming. So if you take someone who's not got any immune response against hep-C, give them the vaccine, they generated very big responses. The levels were higher than we expected but we were pleased to see that also, they targeted a lot of different parts of the virus, because that's really important if you're going to overcome the variation that's already embedded within the viral genome. They did the kinds of things that we'd like the T-cells to do; so they proliferated well and they made the cytokines that I mentioned and they look like they would kill an infected cell.
The second stage is where we're trying to boost with the alternative adenovirus - we had two viruses and we gave a group of patients each one but in different orders. This boosting effect was a bit less than we'd expected and we think that's probably because of what we were just discussing, that once you've seen one adenovirus, you start to make immune responses against it. But the net result, which I think is the important one, is that after six months or a year, so well after the vaccination, we still had very big populations of cells which still seem to have the qualities that we'd really like in a protective response.
Ben - Is it safe to be using viruses that have adapted for other species?
Paul - We went through a number of safety committees to try and make sure this was as safe as possible. I think the key thing is that the viruses are made so they're replication incompetent. A large chunk of genetic material is removed and it's really not possible for the thing to repair itself to become an infectious virus. You can't really expect to make progress in this field if there's any even small hint of a risk from these things because you would be giving them to completely healthy people in very large numbers. So you have to eliminate as many risks as you can possibly imagine.
Ben - So, you've done everything you can to make it safe. It seems to be very effective. What's the next stage?
Paul - It's nice to see these responses but they're all in the test tube, so any vaccinologist would really want to know whether they were protective. What we'd have to do, and what we're planning to do with collaborators in this States, is to look at people who are at high risk of infection. In Baltimore, there's a very well established group of intravenous drug users where, because they use needles, they're putting themselves at risk of hep-C. So, they've designed a trial where they imagine that the rates of infection are sufficiently high that we could really see an impact from this vaccine. So that's planned to go ahead now that we've developed the vaccines to this stage.










Comments
Add a comment