The Genetics of Eyesight
Interview with
Ben - Hi, Robin. First of all, what is inherited retinal degeneration?
Robin - It's a diverse group of conditions caused by defects in any one of 150 different genes. They give rise to deterioration of vision very early in life. It may result in almost absent vision or it may affect individuals in early adulthood or middle age. Whatever the gene defect the result is the loss of receptor cells through apoptopic cell death and further deterioration of vision.
 |  |  |
| Human eyesight with Retinitis pigmentosa or tunnel vision | 'Normal' human eyesight | Human eyesight with Age-related Macular Degeneration |
Ben - Is this a bit like AMD where we lose a particular region of the retina. In particular with AMD we lose our central vision so our peripheral vision is still good but we lose the really important, high-detail bit in the middle. Is inherited retinal degeneration the same or is it a bit more broad?
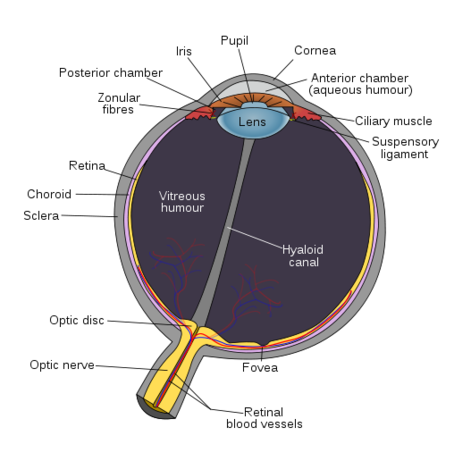
Robin - It's much broader than that because there are at least 150 different forms of inherited retinal degeneration. Some forms - and again it's a group of conditions - called retinisis pigmentosa have defects in genes that affect primarily the rod photoreceptor cell. The patients experience a loss of nightvision and peripheral vision. Often because of the deterioration of their rods their cones start to degenerate later in life. They then start to lose central vision. In other types of inherited retinal degeneration caused by defects in genes that function in cone photoreceptor cells the central vision isn't affected. The condition might resemble the sort of vision loss one would experience in age-related macular degeneration. The cause is quite different but it would be the loss of that central high-definition vision.
Ben - I see. Just to clarify - the rod cells are the ones we use for night vision. They see really in black and white.
Robin - In different light. They don't perceive colour and one uses rod vision in the periphery.
Ben - And the cone cells are the ones that pick up our full tricolour vision. They're more focussed in the macular, the high-detail area.
Robin - Yes, for reading and recognising faces. That's all tone-mediated vision.
Ben - You've mentioned that there are 150 different genes for 150 different types. How have we found the genes? How do we know which genes are going wrong?
 Robin - It's been a huge challenge and you will be aware that the genome project and human genome project was important for the central identification of thousands of disease-causing genes. Essentially it starts with identifying a family that's affected and pedigreed mapping of the genes through crucial genetics and then using molecular genetics to hone down the region to a molecular level. And then, eventually when some candidate genes are found proving that they're the lead-causing and often demonstrating that through production of an animal model that's defective in that particular gene.
Robin - It's been a huge challenge and you will be aware that the genome project and human genome project was important for the central identification of thousands of disease-causing genes. Essentially it starts with identifying a family that's affected and pedigreed mapping of the genes through crucial genetics and then using molecular genetics to hone down the region to a molecular level. And then, eventually when some candidate genes are found proving that they're the lead-causing and often demonstrating that through production of an animal model that's defective in that particular gene.
Ben - So, for example a knock-out mouse.
Robin - yes.
Ben - So we know what genes are causing the problem, can we treat it?
Robin - Well we're starting to make major advances in developing treatments. I have to stress at this point there is no effective treatment for inherited retinal degeneration but my group's been involved ver the last 15 years in developing gene therapy for these sets of conditions. Earlier this year we published the first set of results from a clinical trial of gene therapy from one particular form of inherited retinal degeneration. The results were encouraging and were built on the work of the last decade showing that we could improve vision and slow degeneration in a variety of animal models. But this time earlier this year we showed that we could use the same technology to improve vision in patients.
Ben - Fantastic. Is this using a retrovirus?
Robin - It's not using a retrovirus. It's using a viral vector but it's using a vector based on a virus called adeno-associated virus, which is a different type of virus which is essentially a nonpathogenic palmar virus that is very common in humans. It's not known to be associated with any disease and we've engineered the virus to carry the missing gene and put that gene back into cells of the retina.
Ben - So this has to be applied directly to the retina. You can't give this systemically and just hope that it gets taken in to the right place and the gene is expressed in the retina.
Robin - The vector is administered through a quite complex surgical procedure that localises the viral suspension very precisely between two layers of cells in the retina. Between the photorecoptor cells and the retinal epithelia. In this particular condition the gene defect is in the gene that is expressed normally in the retinal epithelium. We target the virus to that cell there. The virus is taken up by the cells and the gene expressed in the cells and produces the normal gene product in that cell.
Ben - It sounds incredibly promising. Do you think you're likely to have similar gene therapies for other diseases in the retinal degeneration spectrum or things like advanced age-related macular degeneration?
Robin - Well I think the technology is certainly very promising. It's taken us fifteen years to move from the bench into the clinic. We expect that the next disorders that we'll treat we'll be able to do so much more rapidly. The time for development is going to be diminishing just because we've learnt so much more about the safety profile and the technology that's required for efficient gene delivery to the eye. We have now a programme that includes the development of gene therapy. Not only for the disorder we're treating at the moment which is a type of Leber's congenital amaurosis due to a defect in RP65. But we're looking at three or four other rare inherited disorders as well as developing a gene therapy approach for age-related macular degeneration. For AMD we had to take a slightly different approach. The approach would involve replacing defective gene but using a gene therapy vector as a way of delivering a medicinal product. Instead of having to use repeated injections of an antibody to target blood vessels growing in the retina we might be able to use a gene therapy vector to deliver a gene that will have the same result. The advantage of that is a single administration.
Ben - I've no doubt that multiple injections into the eyeball will make quite a lot of our listeners quite squeamish.
- Previous The Benefits of Blinking
- Next Laser Eye Surgery










Comments
Add a comment