Scanning for Osteoporosis
Interview with
Chris - Every year, about 75,000 people suffer a hip fracture in the UK and a majority of those will be down to the condition osteoporosis, that's the underlying cause of their bones being too weak. This is basically bone thinning as we age. Dr. Ken Poole is with us now. He's a rheumatologist at the University of Cambridge where he's studying how bones weaken and change with age, and then some new ways that we can try to use to combat the problem. Hello, Ken.
Ken - Hello, Chris.
 Chris - Thanks for joining us on the Naked Scientists. First of all, just fill us in, what actually is osteoporosis?
Chris - Thanks for joining us on the Naked Scientists. First of all, just fill us in, what actually is osteoporosis?
Ken - Well, exactly as you say. They're porous thin bones that fracture when they shouldn't. So, a lady walking along, falling over from a standing height shouldn't break a wrist, but in osteoporosis, you might, bending to tie the shoelaces fracturing a vertebra. So the little old lady, why is she little? Because of vertebral fractures, the bones collapsing. In the case of hip fracture, a trip or a stumble, or a fall, enough to break a hip.
Chris - If you were to take a piece of bone from someone who has got osteoporosis, how would it compare if you looked at it both macroscopically, just by eye, and then microscopically down a microscope with someone who's got normal bone?
Ken - Well, we do things like this in the clinic. So, when we take a piece of bone normally from people's pelvis, the bone has a thick outer shell and an inner honeycomb which is a mesh full of struts. In a young person, the outer shell is nice and thick and the honeycomb mesh is also thick, providing lots of support, like the inside of a Crunchy bar. If you have an osteoporotic patient, then the outer shell is very much thinner and the mesh of struts may not even be there at all or where they're there, they're thinned and they don't connect properly.
Chris - Do we actually know why this happens? I mean, are some people pre-destined to get this because of family reasons? Is there a genetic cause or is it purely just down to how much exercise you have or haven't had, or what your diet's been like earlier in your life?
Ken - Well those are all good points and fractures are multifactorial. So you have the low bone strength from the osteoporosis, but you also have falls, you also have genetic factors. One interesting factor is that if your parents have had a hip fracture, a mother or father, then your own risk of a hip fracture is higher as well. And coming into that, things like reflexes as well, so your ability to deal with the fall which gets worse as you get older.
Chris - What can we do about it? So someone is diagnosed with osteoporosis. They have a fracture of a wrist or something, they slip on the ice, what can we do once you've picked it up?
Ken - Part of that job is greater awareness and things like the National Osteoporosis Society is great at doing that. A risk fracture in an older woman is not something that you can leave, and you can ask some questions of that person and find out whether they've got very low bone density that can be improved by drugs. And we've got plenty of drugs now that actually help and as we've discussed earlier, the exercise will help too. And it's also dietary and even sunlight, things that can help with your bone strength.
Chris - Okay. Well, talk us through then, when you put someone on therapy, how are you monitoring them and taking this forward in the research domain, what are you actually doing to try to work out how to optimise therapy for this?
Ken - So, one of the things that we use at the moment is DEXA scanning. A lot of people have heard of this bone density scanning. That is where we put people onto a bed, look at their spines and hips, and work out how dense the bone is and compare it to a normal range. But we also know that half of people with hip fractures have a normal bone density result or one that doesn't come up as the osteoporosis threshold. So, one of the things we need is better ways of picking people up, and also, monitoring their treatments.
Chris - And how are you doing that?
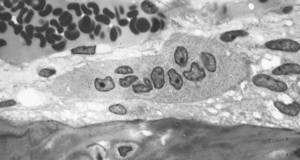
| Osteoclast: |
 |
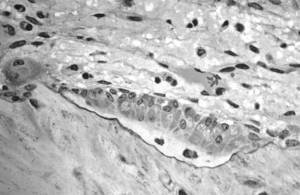
| Osteoblasts: |
 |
Ken - Together with some of the engineers at the University of Cambridge, we've developed a technique which is
based on the CT scans that Ruth dealt with earlier. It was actually interesting to hear that because we're using CT which is computer tomography scans of patients. We can now map the outer shell of femurs, the femoral bone, and produce a colour map of how thick the bones are, and it's very interesting to see that in older people, they're often as thin as an eggshell. My wife says that when you get old, your hips go pink because we use pink for less than 0.3 mm which is eggshell thin. We've done a recent study that shows that one of the commonly used osteoporosis drugs called teriparatide which actually makes bone grow, that's actually able to put bone in places, just like Tim described where you have peak strain in the femur which is a good thing because that's where they often tend to break.
Chris - Because that's where you want the bone to grow.
Ken - That's right.
Chris - Yeah. So, I mean, that was going to be my next point, which is - people who've got osteoporosis have lost bone mass, have actually lost bone substance. You want to put it back. How do drugs and doctors attempt to make people who've got thin bones grow new bone, and why don't people just do that anyway?
Ken - Well, there's drugs called bisphosphonates which are a lot of people are on, which are once weekly drugs usually, and they actually don't make new bone grow. They're the most commonly used drugs, but then you actually stop it being broken down.
As Tim said earlier, there's a process going on all the time of cells called osteoclasts, digging pits in bone, and osteoblasts, filling those pits back up. In osteoporosis, that's out of sync and we called drugs called bisphosphonates which actually stop the osteoclasts from digging pits, and allows the bone that's there to harden off, and that actually prevents fracture, and they're very effective. But right down on the other end of the spectrum, the osteoblasts that cause the bone to grow, there's a drug called teriparatide which is given to patients who are really in a bad way with osteoporosis at the moment. So they've got multiple fractures and our studies showed that when you give this teriparatide, a daily injection, it causes bone to grow in these particular sites of interest.
Chris - One of the stories I mentioned at the beginning was making hearts regrow and scientists are trying to make a heart that's in an adult, think it's in an embryo again because then it will regrow lost tissue. Could we do the same thing for bones and fool bones into thinking that they're back in a baby so they begin to grow new bone, and thereby, get rid of the osteoporosis problem?
Ken - Well, Tim said earlier about the vast amounts of material that might be unnecessary to carry around if you had, say a gene; And in fact, there is a gene, the sclerostin protein which is a funny name, but it's from a disease called sclerosteosis, and by examining that disease, scientists have been able to find just that, the off switch for forming bone. By giving people a monoclonal antibody against this protein, you can actually make bone form at amazing rates in all sorts of places, and that seems to be the most likely approach to make new bone in all sorts of situations where it's needed.
Chris - But that sounds a bit dangerous because you could end up growing bone where you don't want to grow bone, as in where you don't need it.
Ken - And that is actually one of the features of the condition, sclerosteosis, so bone is beautifully regulated and held back from doing silly things, and one of the silly things that it can do is, if it closes off the inside holes called foramen inside the skull, that's a bad place to have bone. The patients who have this disease actually close off things like their facial nerve cavity, their ear canals, and even the very large foramen magnum that carries the nerves, and they can die from this condition. So, it's all things in moderation and a lot of work has to be done to make those safe.
Chris - And just to finish off briefly, Ken. I suppose if you've got systems now that are enabling us to track where new bone is being laid down, if you could work out what the signals are that are active in that site, and then tell this gene which is the bone growth off switch to activate just in that site, then you'd have a way of thickening up the bone where it needs to be thicker, and leaving other sites like the sensitive ones you mentioned unharmed.
Ken - Working out those processes is absolutely key.
Chris - Ken, thank you very much. That was Ken Poole. He is an arthritis research UK clinician scientist at the NIHR Biomedical Research Centre in Cambridge.









Comments
Add a comment