Sequencing an Infection
Interview with
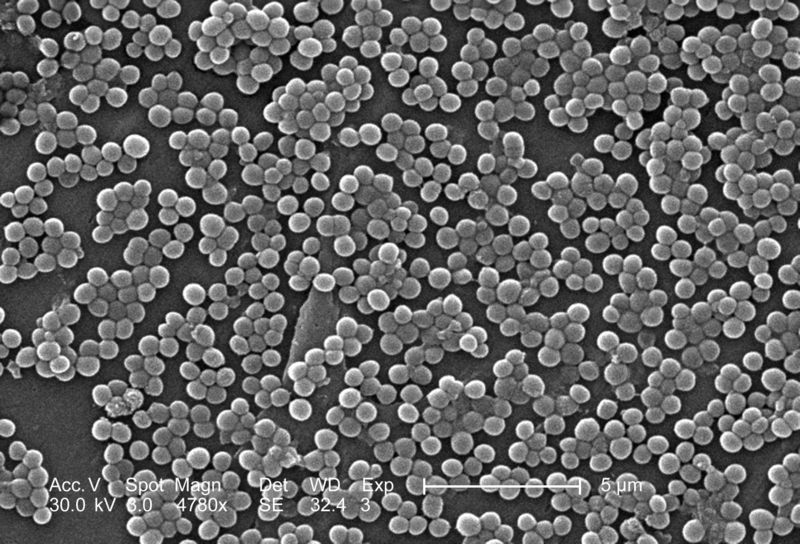
Kat - DNA sequencing technology is developing at a phenomenal rate. Decoding the genetic sequence of the bacterium now takes just hours and costs a few hundred pounds. Ten years ago, this price tag was in the millions. This means that researchers can now begin to marry up the genetic code of an infecting bacterium with how it causes diseases and what treatments might work best. At Addenbrooke's Hospital here in Cambridge, microbiology consultant Dr. Estee Torok is using this technique to try to understand more about MRSA or as it's more formally known methicillin-resistant Staphylococcus aureus. Hello, Estee. Thanks for coming on the show...
Estee - Hello, Kat.
Kat - So, let's track back a little bit and find out what tests do we currently do when someone has a bacterial infection?
Estee - Okay, so the current tests that we do are, we normally take either a swab, or a sample of pus, or a sample of tissue from the patient. That's put in a little pot or a container, taken to laboratory where it's streaked out onto an agar plate and then that plate is incubated in an incubator at 37 degrees for 24 hours, and after that, we look at the plate to see if there are bugs growing on it. Once we see that there are bugs growing on it, we then have to do further tests that are usually biochemical tests, both to identify the bacterium and also to test it for susceptibility to antibiotic drugs. So the whole process takes at least 24 hours to culture the bug and then 24 to 48 hours to identify and get the full susceptibility results.
Kat - So this could be quite crucial if someone's is very, very sick...
 Estee - Absolutely, so when someone comes in the hospital and you suspect they have a bacterial infection, you obviously can't wait for the results of the microbiology test because your patient may not survive 48 to 72 hours, so what we tend to do is give patients empiric antibiotics, so we guess what the bug might be and what it should be susceptible to and then give them what we think is the right antibiotic. But we don't always get that right.
Estee - Absolutely, so when someone comes in the hospital and you suspect they have a bacterial infection, you obviously can't wait for the results of the microbiology test because your patient may not survive 48 to 72 hours, so what we tend to do is give patients empiric antibiotics, so we guess what the bug might be and what it should be susceptible to and then give them what we think is the right antibiotic. But we don't always get that right.
Kat - Why would it be useful to know what's actually in a bacterium's genes? What sort of genes do affect how bacteria infect us and what they do to us?
Estee - In terms of the bacterium, the genetic code will code for things like the structure of the bacterium, for factors that contribute to their pathogenesis, so how they attach to human cells, how they invade human cells. Also, they code for toxins that can cause detrimental effects to the host cells and obviously, they can code for antibiotic resistant genes.
Kat - Which is obviously a hot topic that we'll come to. So, you and your team are working out how to do genome sequencing on bacteria and tell us exactly what sort of technology this is? How quick is it to do a whole bacterial genome?
Estee - I'm working in Professor Sharon Peacock's group at the Department of Medicine, and what we're interested in is to see whether we can bring whole bacterium genome sequencing into the heart of a diagnostic microbiology laboratory. Genome sequencing has been going on, for example at the Sanger Centre, or at reference laboratories, but this has taked quite a long time and cost quite a lot of money in the past. What we're trying to do is to see if we can take some of the newer machines and if we can use them close to the patient in order to inform both clinical care and public health.
Kat - I've seen some of these little sequencers and they're sort of the size of a printer, a desktop printer! How much would it cost to sequence an infection, one person's infection roughly?
Estee - Well it sort of depends. The big sequencers that are used at the Sanger Institute are Illumina HiSeq machines and they are very large and often when we send samples to them, it can take 6 to 8 weeks for us to get a result, and that's relatively inexpensive so less than 50 pounds or so for a genome, but obviously, you can't wait that long. With the smaller desktop sequencers or bench top sequencers I guess you should call them, they're the size of about a printer or one of those expensive cappuccino machines, and we can get a result in 18 to 24 hours, and the costs of coming down. I think you'll have to ask the companies how much they're charging but I would say it's in the hundreds of pounds as opposed to in the thousands.
Kat - This certainly starts to make it seem like something we could do. So if you could start to bring this into the clinic, what would be the benefits of knowing the sequence, the genetic sequence of the bacterium that's infecting someone?
Estee - I don't think we'll ever be in a situation where we can sequence every single bug that comes in to the laboratory, but I think we'll focus on bugs where for example, you think that the patient may be part of an outbreak investigation or where it's important to know things about virulence or drug-resistance more quickly. So, you'll need to pick which bugs you do and then focus on getting those results more quickly in order to either determine whether bugs are related or not in the case of outbreak investigation, or what antibiotics to use in the case of drug-resistance and in the case of surveying the emergence of drug-resistance.
 Kat - And in the news this week, the World Health Organisation was really expressing concern about the rise in antibiotic resistance that we're seeing. They're warning of this perfect storm that might lie ahead of us as we're using more and more antibiotics to treat people and in food production. These bugs are becoming resistant to it and we're sort of losing out in this genetic arms race. So, how can the kind of research that you're doing help to point us towards ways to help to combat this resistance, and could you actually use the information you're getting to develop better treatments?
Kat - And in the news this week, the World Health Organisation was really expressing concern about the rise in antibiotic resistance that we're seeing. They're warning of this perfect storm that might lie ahead of us as we're using more and more antibiotics to treat people and in food production. These bugs are becoming resistant to it and we're sort of losing out in this genetic arms race. So, how can the kind of research that you're doing help to point us towards ways to help to combat this resistance, and could you actually use the information you're getting to develop better treatments?
Estee - Yes, because obviously, if you have the genetic code of the organism, you have all the information that's available in terms of the antibiotic resistance genes. You can then design drugs that can be target against those in a way that you can't when you don't have the genetic codes. The other thing I think it's important is that it gives you a chance to survey the emergence of, for example, new pathogens or more drug- resistant pathogens in real time without having to send off bugs to the reference lab which can take weeks to get a result.
Kat - In terms of what you're doing now, this is a sort of "how long is a piece of string question", but how soon do you think this kind of sequencing might start to become more widespread in hospitals across the UK?
Estee - That's obviously the major challenge and certainly, that's what our group is working on; evaluating some of these new technologies to see if we can use them within a diagnostic microbiology laboratory and developing ways in which to make them a bit more user friendly. At the moment in order to analyse bacterial genome sequences, you often need a bioinformatician who's very experienced at doing that to give you the results in a way that you can understand. And over time, it is hoped that the machines that come out will have onboard computers that will actually be able to be useful to the practicing clinical microbiologist or infectious diseases doctor who will then be able to understand the data without the need for having a scientist to interpret it for them. So, optimistically, I would say 5 years or so, but I don't really know how quickly things will change. Certainly, the technology is there but the translation aspect may take a bit of time because you obviously have to train - a.) Improve the instruments, b.) Train people to use them.
Kat - Patients coming into Addenbrooke's, are they're having their bacterial genome sequenced?
Estee - Well they will be. So we're about to start a study based at Addenbrooke's which will involve sequencing all the MRSA bugs that we collect over the course of a one-year period from patients admitted to Addenbrooke's. We're also collecting bugs from the East of England and also, nationally in order to look at the geography and the diversity of MRSA in the UK and then to look more closely in Addenbrooke's at transmission of MRSA, both within the hospital and between hospitals in the UK.










Comments
Add a comment