Making Cancer Visible to MRI Scanners
Interview with
Kevin Brindle, from the University of Cambridge, has developed a way to trace the location, the growth and the activity of cancers inside the body. With a very powerful magnet, he makes the nuclei at the centres of carbon atoms, in things like sugars, all spin in the same direction. Injected into a patient, these sugars are taken up and used by tumours where the magnetically aligned spins of their carbon atoms gives them away to a magnetic resonance - MRI - scanner, so it can tell where in the body the tumours are. Ginny Smith went to see how it works.
Kevin - Conventionally, the way we assess treatment response in cancer is to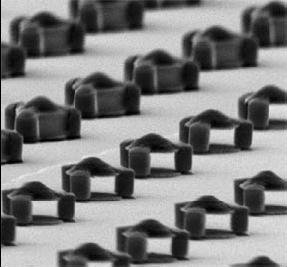 look after drug treatment, whether the tumour is shrinking. The problem with that approach is it can take many days, weeks, or even months before you see any evidence of the patient responding to treatment. What we've been interested in doing is imaging tumour biology, which can give a much earlier indication of whether a drug is actually affecting the tumour and whether the patient therefore is responding to treatment or not. With modern therapies, what we know already is that not all patients respond in the same way. And so, when you give a patient a new drug, you want to find out very quickly whether that drug is working. With the techniques that we're developing, we think we can tell within hours or certainly days whether anything is happening. Clearly, if the drugs not working in that particular patient then you can try an alternative approach.
look after drug treatment, whether the tumour is shrinking. The problem with that approach is it can take many days, weeks, or even months before you see any evidence of the patient responding to treatment. What we've been interested in doing is imaging tumour biology, which can give a much earlier indication of whether a drug is actually affecting the tumour and whether the patient therefore is responding to treatment or not. With modern therapies, what we know already is that not all patients respond in the same way. And so, when you give a patient a new drug, you want to find out very quickly whether that drug is working. With the techniques that we're developing, we think we can tell within hours or certainly days whether anything is happening. Clearly, if the drugs not working in that particular patient then you can try an alternative approach.
Ginny - So, what kind of things can you look at within a tumour to see if it's being affected by a drug?
Kevin - In our work, what we do is, we take a carbon-13-labelled molecule. We can inject that into the patient and then we can image where that carbon-13-labelled molecule goes. We can image it being used by tumours and, frequently, when we treat a tumour, we see a decrease in the rate at which they use this molecule.
Ginny - So, do you put this molecule within a larger molecule?
Kevin - We have recently used glucose but we've mainly used the molecule called pyruvate, which tumours rapidly take up and convert into another molecule called lactate. And how fast they do this tells us something about how healthy that tumour cell is.
Ginny - Now, I think you've got an example of a machine that actually creates that sample that you can inject. Can I have a look at it?
Kevin - Sure. Shall we go down and look it in there?
Ginny - Yes, sounds good. Okay, so we're walking into - well, it doesn't quite look like a normal lab. It looks more like maybe a boiler room. So, there's two big metal, shiny containers and lots of wires and hoses and things coming out in various machines with lights on. Can you talk me through what some of the intriguing looking tubes and knobs and things on it are?
Kevin - Yeah. So, what we're looking at here, this can is a magnet. It operates 3.35 tesla and to put that in context, the Earth's magnetic field is about 50 micro tesla. So, we're more than a million times stronger than the Earth's magnetic field.
Ginny - That would confuse anyone around here with a compass.
Kevin - It certainly would. Okay, so what we do is we put the sample into the bore of this magnet and then we bleed liquid helium on to the sample. So, liquid helium is about 4 degrees Kelvin minus 269 degrees centigrade. And then we put on a vacuum and that noise you can hear is the vacuum pumps running. So, by boiling off the helium, the energy that is used in that takes the temperature further down to 1.2 degrees Kelvin. And at that temperature, the spins become polarised.
Ginny - So, what exactly do you mean by that?
Kevin - For example, the spins that we're interested in - carbon-13, which is an isotope of carbon - if you put those nuclei in the magnetic field, they behave like a bar magnet. Some of them line up with the field and some of them line up against the field. You have a slight excess that line up with field. And it's that polarisation, that slight excess, which gives rise to the signal in the MRI experiment. Okay, now we have a problem. We have our sample where we polarise all these spins, but it's at 1 degree Kelvin. The key now is we need to get it out, very, very fast, and if we can do that, we can retain the spin polarisation. And that's what this device here does.
Ginny - Okay, so that's sort of a long tube with what looks like some kind of gauge at the top and another tube coming off it that looks like you might be able to connect it to something.
Kevin - That's right.
Ginny - What does that do?
Kevin - Okay, so we put what we call a dissolution fluid into here. We heat it up under pressure. Temperature goes up to about maybe 200 degrees centigrade. We then open this valve here that blasts this super heated water on to our frozen sample and blasts it out of the magnet very, very quickly, so fast that we retain the spin polarisation. So, these nucleus spins, these carbon-13 spins that are all lined up now with the field, we keep that, but we lose it quite quickly. As soon as you bring it up to room temperature, you start to lose this polarisation. So then we run over this other magnet and in this magnet, we'll have the system that we want to image. We can then inject this material and now, we have so much signal that we can image where this sample goes in the body and we can then watch how it's used by cells in the body, how it's metabolised, how it's converted from one molecule into another. We can watch that in real time.
Ginny - So, this doesn't look like the kind of MRI machine I've seen in hospitals and things. I'm assuming you don't put a human in this one.
Kevin - No, it would have to be a fairly slim human! The bore size of this is about 9 centimetres, but we have recently acquired a clinical device, which is sat next to a clinical machine up in Addenbrookes Hospital in the Department of Radiology. In a year or so's time, we hope to be doing exactly this experiment that I've just described here, in patients.
Ginny - Now, these machines, they're quite big and bulky. Is that exactly what you'd have to have in a hospital?
Kevin - The clinical device actually is fairly compact, standalone. It will stand just outside the room where the imaging magnet is, and it will spit out labelled material, polarised, that we can inject straight into the patient.
Ginny - How long do you think it'll be before we're seeing this as standard in all our hospitals?
Kevin - We hope that it will be in widespread use in 10 to 15 years.
- Previous What is it like to have MS?
- Next Cancer Screening Tools








Comments
Add a comment