Hit and Run Viruses Leave Tumours in their Wake
Interview with
Chris - Now for many years, scientists have known that viruses are the direct causes of some cancers and probably the best described example is HPV, that's the Human Papillomavirus which is linked to cervical cancer. But recently, researchers at Cambridge University uncovered evidence that viruses might be involved in the causation of a much wider range of cancers than we first thought. One of the scientists behind that discovery is Dr. Stacey Efstathiou. He's with us now. Hello, Stacey.
Stacey - Hi, Chris.
Chris - Firstly Stacey, how do scientists actually think that viruses cause cancer in the first place?
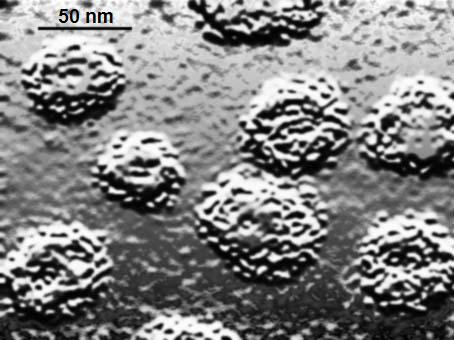
Stacey - Well, there are a number of different ways that viruses can cause cancer. From a historical perspective, if we look back maybe 100 years ago, it was first shown that if you took tumours from chickens - sarcomas - you could mash them up and take a filtrate which lacked anyof these cells, inject it to a normal chicken, and it would develop a tumour. And it was subsequently shown that the virus responsible is a retrovirus and retroviruses are special viruses, that as part of their life cycle, they integrate into the host genetic material. In that particular case, the virus encoded its own oncogene which had captured historically from a cellular oncogene...
 Chris - An oncogene, being a gene that make cells grow, causing cancers.
Chris - An oncogene, being a gene that make cells grow, causing cancers.
Stacey - Causing proliferation of the cell. So, that's one example that viruses causing cancer, the capturing of an oncogene and subsequent expression in a cell.
Chris - And they knew from that experiment that it had to be a virus because if you mashed up the cells to destroy the cells then the only thing that could survive that process presumably is a virus, otherwise it's too small.
Stacey - Absolutely. So that was a landmark discovery and that it was filterable agent, a very small entity, a virus which actually transmitted the tumour from chicken to chicken.
Chris - What's the benefit to a virus of transforming, making a cell become malignant in the first place?
Stacey - Well, I guess you'd say that there isn't much of a benefit. I mean, these are accidents that happen when a virus can't complete its normal lytic cycle, and as by-product of that, a tumour occurs. So, many viruses encode genes which will push the cells into replication and cause those to proliferate, to help the virus be produced. But normally, the outcome of that is death of the cell. It's only in specific circumstances where you haven't got complete lytic destruction of a cell by a virus that a tumour can arise.
Chris - So in other words, the viruses are making things that make cells grow more because the cell that's growing more is good for a virus to grow in because growing cells are more metabolically active.
Stacey - Absolutely.
Chris - But occasionally, an accident happens and something goes wrong genetically which damages that cell's DNA or re-arranges it in some way, so it can become potentially malignant.
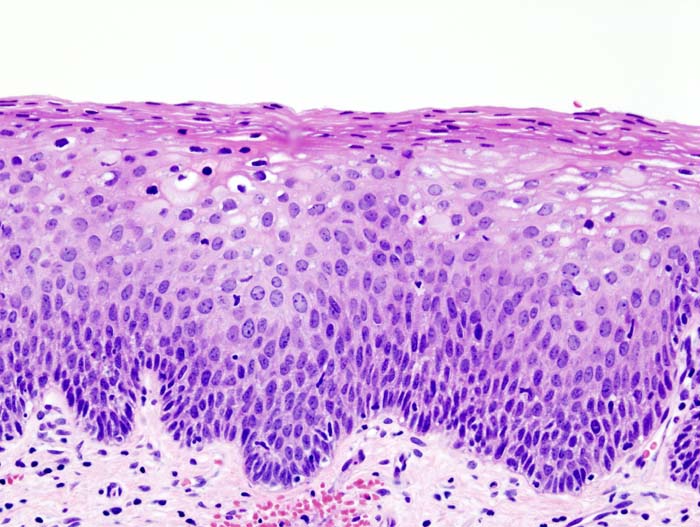
Stacey - Absolutely and a classic example of that - you mentioned already - is Human Papillomavirus which causes cervical cancer. It's a real rare event where one gets an integration of and papillomavirus which is not a normal part of the viral life cycle and when integration happens, you can get expression for one or two of the viral genes which cause cells to proliferate. But because the virus is integrated, it can't complete its longer life cycle and the consequence is proliferation and tumour formation.
Chris - Integration being where the virus has put its genetic material inside the cell's genome.
Stacey - Absolutely, that's right.
Chris - So that's all very well. We can go looking at tissues and we can look for the viral hallmark in the cell's DNA. You've done some work now saying that actually, if we just go looking for cells that bear a viral hallmark of having been damaged in this way, you found some, but actually, there's evidence that viruses may be underlying a lot more in the way of cancers than we first thought.
Stacey - Yes, sure. I mean, this has been a longstanding issue and in the field of virology, the so-called 'hit and run' hypothesis of a tumour formation where a virus can enter a cell, express some genes, make a change to a cell, to cause it to become cancerous, but then disappear. Actually, be lost without trace from a tumour. But of course, how do you study that? It's a very difficult question to address. And so, what we tried to do is to experimentally establish a system where we could examine whether a virus could actually undertake a hit, i.e. enter a cell and expresses something, but then be cleared, once the tumour had been initiated.
 Chris - But obviously leaving a bit of a stink behind in the form of the genetic damage you were talking about that could make that cell cancerous.
Chris - But obviously leaving a bit of a stink behind in the form of the genetic damage you were talking about that could make that cell cancerous.
Stacey - Absolutely.
Chris - And if you went looking, you'd say there's no virus there, but the footprint is there nonetheless.
Stacey - Exactly, so if the hit and run hypothesis is correct of course, it may be that viruses could actually be associated with many more cancers that we currently appreciate because there's no means of associating that virus genetically with the particular tumour.
Chris - How did you do it?
Stacey - Right. So this was actually quite a tricky experimental procedure in which we use transgenic mice which had copies of an activated oncogene, but would only be activated once a virus, which expresses a particular enzyme, which we had engineered into the virus, was expressed in that cell to mediate activation of a cellular oncogene. So, once we infected the mice, any cell that got hit by the virus when you got expression of this enzyme will then trigger this oncogene, that will induce a tumour. And so, the question was, if we follow that tumour, was the virus always retained in that cell or was there subsequent loss of the virus? And what we found was that if we looked at the tumours from animals that inevitably, the viral DNA had been lost from the tumours but the tumours brought all the hallmarks of a virus having once been there. We took this study on further by showing that one could actually vaccinate these animals prior to delivery of this viral enzyme that we cloned into the virus, and show 100% protection against the virus induced tumours. So, this was an experimental system, demonstrating hit and run oncogenesis, and showing that vaccination would be very effective in preventing tumour induction.
Chris - And just briefly, what do you think the implications are of this? This suggests that a lot of the cancers that we're seeing are caused by other things, there may actually have been the early evolution of that cancer, being a virus there, causing this problem.
Stacey - Sure and so, if one looks at certain cancers where a virus is sometimes associated but not always associated with the cancer, could it be that in those cancers where the virus has been lost that there have been an initiating event at one time in the past? And of course, the only way one can realistically prove this in the human population is to develop novel vaccines, so I think the impetus now is to put a lot more effort into the development of vaccines and to roll them out to see if we can actually prevent tumours which you wouldn't necessarily suspect of having a viral aetiology.
Chris - Stacey, thank you. That's Dr. Stacey Efstathiou. He's from the department of pathology at the University of Cambridge
- Previous The Hallmarks of Cancer
- Next Naked Engineering - Ultrasound










Comments
Add a comment