Can antibodies cause schizophrenia?
Interview with
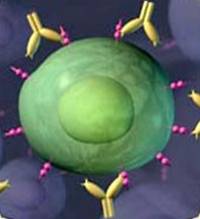 Could the immune system cause schizophrenia in some cases? Oxford scientist Belinda Lennox is finding antibodies targeting certain types of nerve cells in some patients. Blocking the immune system, or flushing out these antibodies, causes the disease symptoms to subside, as she explains to Hannah Critchlow...
Could the immune system cause schizophrenia in some cases? Oxford scientist Belinda Lennox is finding antibodies targeting certain types of nerve cells in some patients. Blocking the immune system, or flushing out these antibodies, causes the disease symptoms to subside, as she explains to Hannah Critchlow...
Hannah - So, there seems to be new computer animation therapies for Schizophrenia, but could there also be a biological treatment that could tackle the underlying causes of the disorder? Could some cases of Schizophrenia simply be down to the immune system attacking the brain? This is exactly what Oxford University's Psychiatrist Belinda Lennox works on. Hi there, Belinda.
Belinda - Hi, Hannah.
Hannah - Can you tell us a little bit about this hypothesis that some cases of Schizophrenia could be down to the immune system getting into the brain and attacking bits of the brain?
Belinda - The story really starts in the world of neurology and neuro oncology in particular. So, in the last 10 years or so, there've been an increasing number of cases of catastrophic encephalitis, or brain inflammation, have been found to have antibodies that are attacking parts of their brain by identifying these antibodies and by removing the antibodies, these patients who were often critically unwell are dramatically improved and sometimes cured. But it was recognised right from the first descriptions of these patients with encephalitis that they actually presented with symptoms
of psychosis. So, our research was taking this work forward in saying, "Would there be some patients with more circumscribed psychiatric presentation to their illness also with these antibodies and therefore, as an extension, maybe there are some cases that we can actually treat the psychosis as well."
Hannah - So Belinda, this sounds very exciting that you could simply remove psychosis, delusions and hallucinations. Have you done any clinical trials with patients with schizophrenia rather than this brain inflammation encephalitis?
Belinda - Well, the first thing we did was to screen some patients presenting with the first experience of psychosis, just to see whether we could find any of these antibodies in those patients. We found in our initial 47 patients, we found 3 patients that were positive for these antibodies so, just over 6%.
Hannah - But where are these antibodies actually coming from from this 6% of the patient cohort that you were looking at?
Belinda - We don't know. When we identified these patients, we brought them back and gave them a good looking over with neurologist colleagues as well because our first thought was actually, have we misdiagnosed these patients? Did they actually have encephalitis? Did we miss something? But on screening, we couldn't find anything that distinguish them in particular. They had all receive diagnoses of Schizophrenia in the time that they'd been followed up under psychiatric services and we looked to see if there is any reason for them producing these antibodies, whether there was a tumour that might be associated with them, but we couldn't find any particular reason. So, our assumption is that it's an autoimmune disorder, that it's the body reacting against some external trigger that we don't know what that is.
Hannah - So, which parts of the brain are these antibodies actually attacking?
Belinda - The most common antibody that we found is the antibody against the NMDA receptor which is a particular interest as Paul was describing because there's an association from many different directions with disturbance of the NMDA receptor and Schizophrenia.
Hannah - So, ketamine kind of blocks these NMDA receptors in the brain and then induces these hallucination, delusional experience and then also, some patients with Schizophrenia have actually got their immune system attacking these NMDA receptors as well and kind of degrading them. So, in that case, can you almost clean the immune system of these patients with Schizophrenia to get rid of their symptoms of psychosis? Have you come up with a new treatment?
Belinda - That's the really exciting prospect. So, since our initial cohort description, we've been screening patients as they come through the first episode psychosis service and when we've identified patients with these antibodies, we've been treating them with immunotherapy as though they had an encephalitis with these antibodies. And that involves a very different set of treatments to the ones that we're used to in Schizophrenia. So, we treat people with steroids, with plasma exchange where they come and have their blood filtered basically to filter out the antibodies from
their blood, or we treat them with intravenous immunoglobulins, which directly get rid of the antibodies in their system.
Hannah - And what kind of success rate are you getting with this immunotherapy treatment?
Belinda - I'm cautious to claim any grade results because it hasn't been done in a randomised control way. But we have treated about 20 patients now and each patient has improved with the psychiatric symptoms so far.
Hannah - So how long have they got to stay in a hospital for and if they've got to continue having this immunotherapy?
Belinda - We're treating them again as with other patients with encephalitis. So, we give them a course of intravenous immunoglobulins over 3 to 5 days. We give them 3 days of very high dose steroids and then we continue treatment with either steroids or a steroid sparing immunosuppressant. So again, a very sort of different drugs that those that we used in psychiatry. We follow people up for at least a couple of years to make sure that they stay well.
Hannah - I mean, other disorders of the brain like for example, dementia or Alzheimer's, could they possibly be implicated in this immune system attacking the brain as well?
Belinda - There are some research groups that have also been looking at this area. There's got to be some caution in that in older people or particularly if there is other sort of known brain pathology going on. You quite often find a lot of antibodies being produced against all sorts of targets. So, actually separating out not clinically relevant antibodies, is quite a task. So, there have been these NMDA receptor antibodies described for instance in cases of Creutzfeldt-Jakob disease and in some cases of sort of rapid dementing illnesses where it's quite difficult to untangle what's causing what. So, I suppose there is lots of work still required.
- Previous Chatty Dolphins
- Next Cartoon avatars stop schizophrenia










Comments
Add a comment