DNA Sequencing Stops MRSA Spread
Interview with
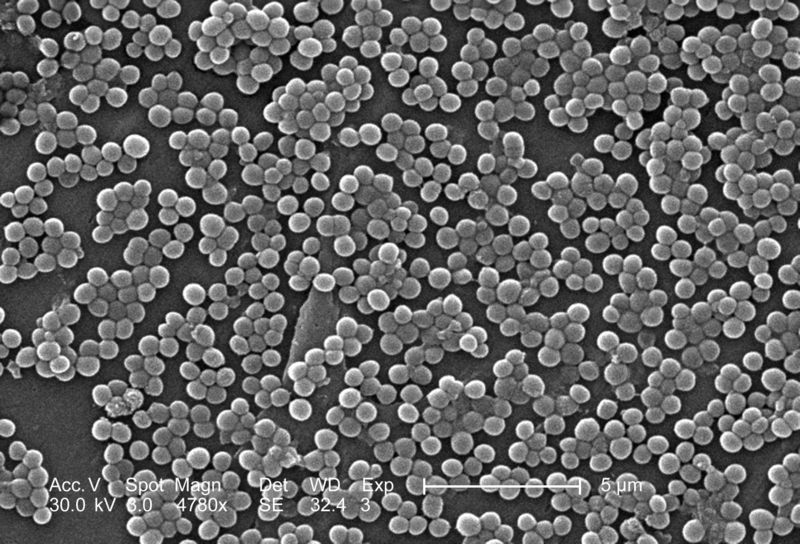
This week, the journal Lancet Infectious Diseases included a rather unusual detective story - one where rapid DNA sequencing was used in a hospital to track an outbreak of MRSA down to one unsuspecting carrier. It bears all the hallmarks of good television forensic crime drama, but it actually took place right here in Cambridge, and the research paper they released is said to be the first example of using this technique to bring an infection to a close.
Chris - The author of that study is Professor Sharon Peacock from Cambridge University. She's with us. Hello, Sharon.
Sharon - Hello, good evening.
Chris - Why did you do this?
Sharon - We want to control MRSA transmission, the passing of it from one patient to another, as much as possible because we want to contain any infections that might arise. And so, we need to see when MRSA does move from one person to another and we need to see it fast.
 The way we do that at the moment is we work out whether two patients who are MRSA positive could've got it from each other because they're in the same ward at the same time. But what we can't do at the moment is to do any sort of typing on the bacteria to see how related the two are.
The way we do that at the moment is we work out whether two patients who are MRSA positive could've got it from each other because they're in the same ward at the same time. But what we can't do at the moment is to do any sort of typing on the bacteria to see how related the two are.
If we had a tool where we could see that they're were either related or unrelated, that would be very helpful because we could work out if transmission had occurred from patient A to patient B, but those tests aren't available at the moment and that's a problem for us.
Chris - So, we know that the two patients have got MRSA, but there's more than one form of MRSA, at a molecular level, so we don't know whether they've come into the hospital independently with their infection or something in the hospital is transmitting these infections between these individuals.
Sharon - That's exactly right. You can't see the transmission pathways between patients. So, what this new technology does is to actually sequence the whole genome with the bacterium.
Even just a few years ago, sequencing a bacterial genome would've cost hundreds of thousands of pounds and taken several years to do a single one. There's new technology now available which allows you to do sequencing of multiple genomes within a day actually, very, very fast and the price has actually fallen very rapidly. That means that we can bring this technology to clinical practice quite soon. In this research study, we really wanted to test out how useful that could actually be in trying to understand better an MRSA outbreak on our Special Care Baby Unit at Addenbrooke's Hospital.
Chris - Can you talk us through how you actually did the study? What were the steps and how did you investigate what was going on?
Sharon - Well, we had access to this technology and we knew that there was a suspected outbreak of MRSA on our Special Care Baby Unit, which should be investigated by our infection control team. Now, they were not sure whether an outbreak had occurred over an extended period of 6 months. There were cases coming into Special Care who were MRSA positive, but we weren't sure if they were related. And the reason for that is because throughout that 6 months, there were quite large gaps when there were no people who were MRSA positive at all. And so, one has to ask, how has that transmission gap been closed?
So, what we did in the first instance was, we took all of those isolates and we sequence them, and we're able to say very quickly that they were all so related at the genome level that this had to be an outbreak. At the same time we extended our search to look for bacteria that are coming from GPs actually in outpatient departments. We sequenced those and we found that actually, the outbreak was twice as big as originally thought and that there were cases actually in the community, people had developed infections. We really only linked that to the Special Care Baby Unit through the sequencing.
Chris - So that meant that you were then able to say right there, there are outbreaks occurring. How did you then go and find the individual that was causing those outbreaks?
Sharon - Well, having identified that there was definitely an outbreak, we put the Special Care Baby Unit under very close surveillance to see if new carriers or people infected with MRSA popped up. Actually, 2 months after the previous MRSA carrier, we found a new MRSA carrier, an infant, and we were puzzled by this because there's obviously a very long gap when we saw no MRSA at all. And it was at this point that we thought there must be a carrier amongst a member of staff.
And so, we gathered the staff together and got full agreement that they would be swabbed and we saw with 154 staff members, we found just 1 that was a carrier. And so, of course we immediately sequenced that and it was a direct match to the outbreak strain. What we think is that this person was involved in the outbreak. What that allowed us to do was to actually treat that individual so that the MRSA carriage is removed from them and that effectively stopped the outbreak from continuing any further.
Chris - How do you know that they gave it to the kids and not the other way around?
Sharon - I think that it will be difficult to be absolutely unequivocal about that individual causing spread throughout the entire outbreak, but what we did do with the staff carrier was we sequenced lots of single bacteria from their carriage population and we got genetic matches to before the 2-month gap and after the 2-month gap. We think that that is fairly strong evidence actually that that person was at least involved in that transmission event.
Chris - This is obviously extremely helpful in terms of guiding infection control strategies, but are there any other uses for this sort of technology in guiding how we tackle bugs of all kinds in the hospital?
Sharon - I think actually that there'll be numerous applications for this. We'll need to work out exactly where, when, and how to use it, but for example, it could be really key in investigating the food-borne outbreaks to work out if there is an outbreak and to help contain that. We could use it for example to get rapid drug susceptibility testing for people with tuberculosis. So, there is a very wide range of applications for this technology and I think that we will be seeing this brought into use in the next few years.
- Previous Gene Therapy Cures Epilepsy
- Next The Rise of the Bed Bug










Comments
Add a comment