Finding Flu Fast
Interview with
It's time to find out about a revolutionary new way to diagnose our winter bugs in two hours rather than two weeks. It's going to lead to numerous benefits in treating flu and other respiratory viruses. We sent Meera to Addenbrooke's Hospital to find out more.
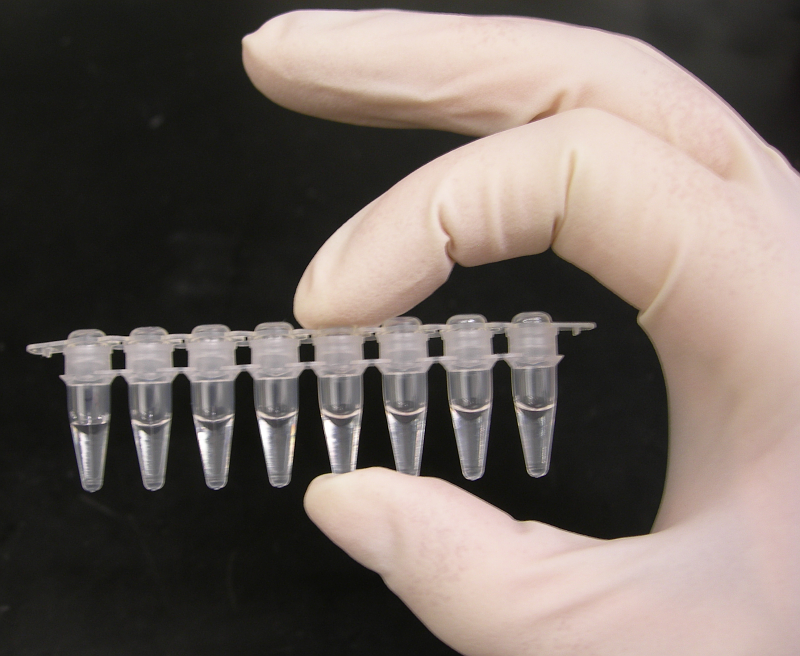
 Meera - Know how that feels? I'm sure you do. Each year, we're all hit with either the flu, or if we're lucky, just the cold but it always seems to take ages to recover and even longer to get a clear diagnosis from the doctor about which bug is causing us to feel so unwell. Part of the problem is that there are hundreds of different viral infections. They all have slightly different characteristics which means they're difficult to identify on their own. To do it scientists either have to grow the offending virus in the laboratory or study the antibodies being made in the patients blood to find out what viruses they're fighting off. In both cases the process is really slow and patients have either recovered or deteriorated significantly by the time the diagnosis is made. Of course, these delays make it difficult for doctors to know how best to treat severely ill patients and to tell who should be isolated to prevent cross-infections in hospitals or out in the community. Now, a new technique developed by researchers at Addenbrooke's Hospital in Cambridge can identify some of the most common respiratory infections in less that two hours potentially solving many of these problems. It works by copying the nucleic acids, or in other words the DNA, or a related chemical called RNA within 8 of the most common virus infections that strike in the winter time including the flu virus. To detect which viruses are present in a patient's sample the researchers also add coloured probes which glow when they detect DNA from a specific virus. As the viral genetic material is copied it glows more and more brightly. By using different coloured probes to recognise different viruses all the team have to do is read off the colour of the solution to see which virus is there. If more than one virus is present it can tell that too. Martin Curran is one of the scientists behind the work.
Meera - Know how that feels? I'm sure you do. Each year, we're all hit with either the flu, or if we're lucky, just the cold but it always seems to take ages to recover and even longer to get a clear diagnosis from the doctor about which bug is causing us to feel so unwell. Part of the problem is that there are hundreds of different viral infections. They all have slightly different characteristics which means they're difficult to identify on their own. To do it scientists either have to grow the offending virus in the laboratory or study the antibodies being made in the patients blood to find out what viruses they're fighting off. In both cases the process is really slow and patients have either recovered or deteriorated significantly by the time the diagnosis is made. Of course, these delays make it difficult for doctors to know how best to treat severely ill patients and to tell who should be isolated to prevent cross-infections in hospitals or out in the community. Now, a new technique developed by researchers at Addenbrooke's Hospital in Cambridge can identify some of the most common respiratory infections in less that two hours potentially solving many of these problems. It works by copying the nucleic acids, or in other words the DNA, or a related chemical called RNA within 8 of the most common virus infections that strike in the winter time including the flu virus. To detect which viruses are present in a patient's sample the researchers also add coloured probes which glow when they detect DNA from a specific virus. As the viral genetic material is copied it glows more and more brightly. By using different coloured probes to recognise different viruses all the team have to do is read off the colour of the solution to see which virus is there. If more than one virus is present it can tell that too. Martin Curran is one of the scientists behind the work.
Martin - It uses fluorescent oligonucleotide probes that are mirror images of what you're amplifying: a little short stretch. Each of these have different labels on them. You can have a red, green, a blue or orange. So what happens is you can put these in to different viral targets and if you are amplifying specifically the virus of interest that will actually bind and you'll get a certain fluorescent reading from that. We can use different probes with different colours on and in effect do four or five different reactions in a single tube. We call that multiplexing: to screen for the thirteen or fourteen different viruses that can cause respiratory infections.
Meera - What kind of samples are you getting from patients in order to look for these viruses then?
Martin - We get a whole range - sometimes we get nasal-pharyngeal aspirates which are swabbed off the back of the throat. We get nose swabs or throat swabs. Certainly, we get some BALs (bronchoalveolar lavages) that are deep washes from deep down in the lung.
Meera - How do you get from these samples to actually putting them in a machine for analysis?
Martin - We get the samples and we strip off all the protein and all the virus and just purify the nucleic acid whether it's RNA or DNA. Then that sample will go into the real-time PCR.
Meera - What have the benefits been so far?
Martin - Previously, the sensitivity was poorer. You might only find 30% of your samples positive whereas with this new technology it's far more sensitive and our positivity rate for the samples that have come in is sitting at about 75%.
 Meera - So we know how it's possible to get such a speedy and more accurate diagnosis. Has this made a difference in practise? I asked Tim Wreghitt, a consultant virologist, if there have been any benefits.
Meera - So we know how it's possible to get such a speedy and more accurate diagnosis. Has this made a difference in practise? I asked Tim Wreghitt, a consultant virologist, if there have been any benefits.
Tim - They've been quite substantial. First of all, it means that we can diagnose infections quicker. With the previous techniques we had which was largely virus culture it could take a week to get a result. If you're saying that patients need to be treated, for example, for influenza within 48 hours if you just did culture that would completely rule out them being treated.
Meera - I guess also a reduction in the amount of time will reduce the amount of spread of it.
Tim - Absolutely and that's very important. If you have, for example a patient in an intensive care unit you need to make sure that if the patient does have influenza you pick it up quickly. You can then make sure staff are vaccinated and that patients nearby are given prophylaxis. Equally, if we can identify the case quickly then we can review their treatment so if they're on antibiotics and there's no proven bacterial infection we can maybe take them off antibiotics and make sure they're on a proper antiviral and we have had cases here where that's happened. Patients have got better quite quickly.
Meera - I guess there's also a large benefit of taking people off antibiotics if they don't need them because they can develop resistance to things like that, can't they?
Tim - Absolutely, not only resistance but also they can develop side-effects. If you give certain antibiotics to people, particularly if they're older, then they are likely to develop very profuse, watery diarrhoea. The fewer people we have on antibiotics the better.
Meera - Since this technique has been in use in Addenbrooke's have there been any interesting findings?
Tim - There have. For example the increase in sensitivity means we have detected far more infections in patients with symptoms. So now as we're looking with more sensitive techniques we're beginning to understand the patients aren't necessarily infected with one virus. They may be infected with two or three. It's fair to say we're currently working through those to try and understand better which viruses are causing the symptoms.
Meera - The reason why some colds are worse than others could be because we're being hit by more than one bug at once. This real-time PCR technique can now rapidly identify some of the most common problem viruses allowing doctors to prescribe the right medication much more quickly and also to isolate patients more promptly preventing spread of infections. Gone are the days of just being sent away by the doctor with the line, 'it's a virus,' because in future you'll know which one and whether you really do have a good reason to take a day off work.
- Previous Influenza - Flu Facts
- Next Virus Vaccination










Comments
Add a comment