How the Intestine Informs the Immune System
Interview with
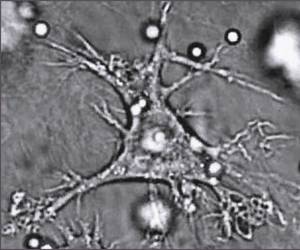
Chris - This week, how the intestine tells harmless food items from potentially harmful bacteria and parasites has been revealed by researchers in the US. Professor Mark Miller at Washington University in St. Louis was using a technique called two-photon imaging to study the intestines of living mice. These animals were special because one class of their immune cells had been made to glow, so they could be seen easily. These are cells called dendritic cells or DCs and they're known as antigen presenting cells because their job is to educate the immune system about what it should attack or ignore. But when Mark then fed these animals samples of sugars that had glowing labels so that he could follow how those food components got moved across the intestinal wall and introduced to the immune cells, he wasn't quite expecting to see quite what he did...
Mark - The surprising finding was that the cell that does this is a highly secretory cell. It's called the goblet cell and its primary function is believed to be secreting mucus that provides a barrier or protection to the epithelial layer. What we found is that these cells, as they secrete, they also allow some of the luminal contents to be transported across the epithelium. So this is different from the process by which you would absorb nutrients or food. It's a way to deliver very concentrated amounts of an antigen to antigen presenting cells, and it's a new function that we've discovered for the goblet cell which has been studied for a very long time.
 Chris - Now you looked at one particular tagged antigen. Obviously, it's slightly more complicated when we're eating a balanced diet and there are lots of things coming in. So, have you got any idea as to whether or not those goblet cells discriminate between the good guys and the things we want to educate our immune system to ignore, and the bad stuff that we actually want the immune system to attack or do those goblet cells transfer everything and the immune system makes that decision?
Chris - Now you looked at one particular tagged antigen. Obviously, it's slightly more complicated when we're eating a balanced diet and there are lots of things coming in. So, have you got any idea as to whether or not those goblet cells discriminate between the good guys and the things we want to educate our immune system to ignore, and the bad stuff that we actually want the immune system to attack or do those goblet cells transfer everything and the immune system makes that decision?
Mark - That's a fascinating question. What we think is that their transporting mostly small soluble peptides, so these can be parts of a protein or intact proteins. It can also be things like sugars, so we're using dextran as one of our model antigens. So I think if there's any discrimination, it's that it would prevent something large like maybe an intact bacterium from getting across but allow these small soluble antigens to actually get across. But on the other hand, once the antigen comes across the epithelium, the antigen presenting cells themselves have specific receptors to take up sugars or certain proteins. So, even if there's a lack of specificity at the goblet cell step, the dendritic cell itself will be better at taking up certain substances and that could also lead to a different outcome in terms of an immune response.
Chris - If I have a healthy gut and I'm just presenting normal food stuffs then I can understand that being an absolutely perfect mechanism. But what about when I get a dose of Delhi belly or Montezuma's revenge, I get bacteria there that I shouldn't have or an overgrowth of even a parasite. Surely, there will then be antigens going across the wall of the gut. How do you stop the immune system saying these are friendly? How do you make the immune system on that occasion decide to attack that foreign antigen?
Mark - It's interesting that we've seen that this function of goblet cells appears to be downregulated when you have a pathogenic infection, so it's as if the barrier, the mucosal barrier, tightens up. So that's one response, but the fact that the antigen is coming in with a pathogenic organism will cause inflammation, pathogen associated molecular patterns will stimulate dendritic cells in such a way that they promote an inflammatory immune response. So again, that would happen at the level of the dendritic cell.
Chris - And what about in allergy states and other disease states? We know that there's an association if you give very young kids big doses of broad spectrum antibiotics that clear out lots of the bacteria that should be there then they're much more likely to develop allergy and diarrheal states later in life. Have you got any clues from the mechanism you've spotted how that sort of thing might actually be manifest and why it happens?
Mark - Yes, we do. So for example in the paper, we used germ-free mice that lack the normal flora that would colonise the small intestine. And in that case, we saw quite a lot of antigen being transported across. So, that experiment is showing that the normal flora or the bacteria in the gut may very well regulate this process. So depending on what species of bacteria are present or whether or not it's pathogenic or non-pathogenic, that could tie in very closely with how much of that antigen is delivered across the epithelium and change the character of the subsequent immune response.
Chris - And are you in a position now to manipulate this system? Do you understand what the trafficking system is, so that you can go in and intervene, and stop things that might provoke an allergy or indeed in someone who has an established allergy, stop it presenting itself to the immune system, so that person's allergy goes away?
Mark - We are definitely working in that direction. It turns out that we think this transport function is directly related to goblet cell secretion. And of course, we have both agonists and antagonists to either induce secretion or inhibit secretion. So, we are looking in various models right now to see how either shutting down this goblet cell mediated antigen transport or upregulating it may affect outcomes in models of inflammatory bowel disease for example.










Comments
Add a comment