The Science of Hepatitis
Interview with
Ben - Any new therapies will ultimately descend from a greater understanding of the science of hepatitis. So I met with Professor Jane McKeating, who is head of the hepatitis C Research Group at Birmingham University. Her lab has been responsible for some groundbreaking hepatitis C discoveries, although the disease itself was only discovered relatively recently.
Jane - So hepatitis C was discovered about 20 years ago by Michael Houghton and his colleagues at Chiron.
Ben - And since it was first discovered how much have we found out about it?
 Jane - Oh my gosh, a lot! Over the last twenty years there have been huge, really big, jumps, I would say. This doesn't happen very often but in the hepatitis C field there have been jumps over the last twenty years from discovering the viral genome, to then showing that that virus was capable of actually infecting animals and causing hepatitis, then was the ability to grow the virus in the laboratory and that immediately led to the development of new antiviral therapeutics so I think that really it's a textbook of showing how good basic science can lead to rally big strides forward in understanding a human disease.
Jane - Oh my gosh, a lot! Over the last twenty years there have been huge, really big, jumps, I would say. This doesn't happen very often but in the hepatitis C field there have been jumps over the last twenty years from discovering the viral genome, to then showing that that virus was capable of actually infecting animals and causing hepatitis, then was the ability to grow the virus in the laboratory and that immediately led to the development of new antiviral therapeutics so I think that really it's a textbook of showing how good basic science can lead to rally big strides forward in understanding a human disease.
Ben - And through the understanding that we've developed, we've already been able to wipe out hepatitis C from blood transfusions but we still don't have a working vaccine or a treatment that we know will wipe it out. How far away do you think these might be?
Jane - Let's say that currently the accepted therapy is an interferon/ribavirin combination. Now in some viral genotypes that's quite a good therapy and we're getting about a 70% response rate. When we say response rate, those individuals are now, clinically, cured. We can't detect the virus in the blood anymore; we can't detect it in the liver. We would hope that within the next five years that we will see a huge battery of new therapeutics coming on line, will be routinely used, targeting the viral enzymes. And I think that we'll envisage that in five years time, we'll start to be at a stage where we are with HIV; in that you will give tailored drug therapies so that you want to give the best possible combination of therapeutics to an individual that respond to the virus they're infected with. That's maybe more in the ten year window but, certainly, there will be a real change over the next five years.
Ben - So how does it initially get into the liver?
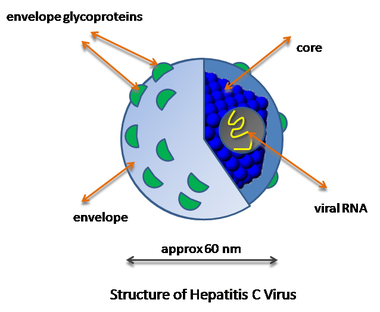
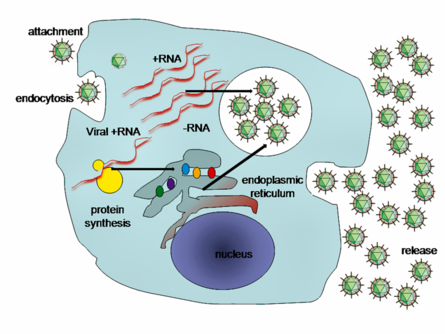 Jane - We envisage that it will be blood-borne and that most things naturally will migrate to the liver. Firstly it will come into contact with the sinusoidal endothelial cells. Now they are interesting as they express a number of the receptors which we think the virus engages but they're not permissive to viral infection. And so we think that they may be important for, maybe, antigen uptake; that they may be important for tolerising the immune response that may be initiated in the liver; we then get movement of the virus into the hepatocytes. That's the primary cell-type within the liver where the virus is replicating. At the moment we know that there are four molecules we believe are important. The first two molecules were CD81 and scavenger receptor B1, which is important for cholesterol metabolism. Now both of those molecules, I think we could safely say, could be classified as receptors in that they interact with the virus. We then have two other molecules; claudin-1 and occludin, which are members of the tight-junction protein family, which, so far, may actually be a facilitator of entry in that they are required but they may not interact with the virus directly. So we have these four molecules which, interestingly, are expressed in other places of the body but it's how these four molecules work in a very unique way to the hepatocyte that we are currently trying to understand in how that's taking it into the virus and we are looking for antibodies and small receptor mimics that can actually target these molecules and, therefore, prevent entry.
Jane - We envisage that it will be blood-borne and that most things naturally will migrate to the liver. Firstly it will come into contact with the sinusoidal endothelial cells. Now they are interesting as they express a number of the receptors which we think the virus engages but they're not permissive to viral infection. And so we think that they may be important for, maybe, antigen uptake; that they may be important for tolerising the immune response that may be initiated in the liver; we then get movement of the virus into the hepatocytes. That's the primary cell-type within the liver where the virus is replicating. At the moment we know that there are four molecules we believe are important. The first two molecules were CD81 and scavenger receptor B1, which is important for cholesterol metabolism. Now both of those molecules, I think we could safely say, could be classified as receptors in that they interact with the virus. We then have two other molecules; claudin-1 and occludin, which are members of the tight-junction protein family, which, so far, may actually be a facilitator of entry in that they are required but they may not interact with the virus directly. So we have these four molecules which, interestingly, are expressed in other places of the body but it's how these four molecules work in a very unique way to the hepatocyte that we are currently trying to understand in how that's taking it into the virus and we are looking for antibodies and small receptor mimics that can actually target these molecules and, therefore, prevent entry.
Ben - And how does it get from one liver cell to the next one, does it have to go via the blood again?
Jane - That's a good question, something that we're working on quite actively at the moment. It looks now that that there are two pathways. Particle assembly is essential and you can get release from one liver cell and re-infection from the cell-free particle route which is the traditional way and that's dependent on all the receptors I've just described. Or the more recent data we're finding is that the virus seems to move through cell-cell junctions and, therefore, is resistant to complement and antibodies that you will find in the peripheral blood.
 Ben - Many different viruses are also good at hiding from the immune system. Does hepatitis do the same thing?
Ben - Many different viruses are also good at hiding from the immune system. Does hepatitis do the same thing?
Jane - Yeah, we published earlier this year that hepatitis C virus can actually internalise into B cells and we've also documented it going into T cells, very much akin to what's been published for the HIV, that you can actually move around the body and hijack a B cell and that B cell doesn't support the replication of the virus but it can deliver it to a hepatocyte. The fact that I said earlier that the virus actually utilises tight-junction proteins; these proteins are actually very important for maintaining epithelial cell barrier function and the hepatocytes of the liver form very tight barriers and what we find is that when they become infected that barrier breaks down and you get a reorganisation of localisation of tight junction proteins which, interestingly, allows lymphocytes to get into areas of the liver where hepatocytes are, which we would perceive may actually promote the fact that the virus is actually internalising into a B cell and for that B cell to then deliver the virus to a hepatocyte, so it's quite a neat trick.
Ben - So the virus infects a cell and then not only primes that cell to allow that cell to pass the virus to neighbouring cells of the same type but also actually encourages immune system components in that it can then infect to use as a vehicle...
Jane - Yeah, that's pretty new information, yeah, from what we are seeing at the moment. What we don't know as yet, is that a route that you could actually use to infect host to host as well. But we know it is a blood-borne virus, whether the blood is actually within a cell or in a cell-free form and whether being within a B cell actually maintains the virus half-life is an interesting thought and we are literally doing those experiments at the moment.
Ben - You've mentioned HIV which has obviously had an amazing outpouring of resources and a great deal of study. Can we learn from the research that's gone into HIV, ways to avoid the resistance that's been seen in HIV?
Jane - I trained as a HIV [researcher], this is where I did my PhD and studies so I think there's a huge amount we can learn from HIV. We certainly can see it's an RNA virus so we immediately with a multi-drug therapy we will see resistance patterns. And we know we are going to resistance patterns in hepatitis C treatments, so I think it's set the stage, we know we are going to have to go with combination therapy, and HIV is leading the way on tailored therapies so there is much we can learn and we mustn't reinvent the wheel.
Ben - So what's the next step for you and your team here at Birmingham?
Jane - The next step. We're really still trying to understand the viral entry process. Why does the virus only really infect the hepatocyte and, importantly, how we can design studies to understand the pathology? How does the virus get into the liver but, more importantly, does the virus itself cause the damage to the liver or is it the immune infiltration that is actually causing the damage? Now, classically for many years, hepatitis is seen to be something where the damage is driven by the immune system. But that was before we had a virus in a lab which we could grow and a virologist can't really do much in the lab until we have a virus. So now that we have one we are beginning to see that the virus is contributing to the pathology also so I think we really want o understand those interactions and how the virus can modulate the lymphocyte recruitment and movement into the liver.
Ben - So as we discover more about the hepatitis C virus we are learning more about how it evades and takes advantage of our immune system. Although we've only had twenty years to study the virus, the science has come on in leaps and bounds and many potential routes for clinical development lie ahead of us. That was Professor Jane McKeating.










Comments
Add a comment