What's in a vaccine?
Would you give your child a vaccine? While the scientific community agrees on the benefits and safety of vaccines when compared to the risks of contracting a disease, there is still a good share of public opinion that is not so convinced. Besides the belief that some vaccinations may cause autism (repeatedly debunked by scientific studies, therefore not further discussed in this article), some have concerns on the impact that certain vaccine ingredients may have on the health of the patient.
Looking at the list of ingredients on a vaccine, from formaldehyde to neomycin, it not immediately clear what they do. This article will go through the various components, explain what they are doing there and examine the current literature regarding their safety. To start with though... why do we need vaccines?
Battle stations
When a disease enters your body for the first time, you rely on your inner defense mechanism, the immune system, to destroy it before it destroys you. However, although a branch of our immune system bursts into action almost immediately, a "first aid" generic reaction, weeks are needed before the full force of your immune system is deployed. This is due to a few reasons. Firstly, the immune system must pass checkpoints, such as making sure it is not in fact attacking a product of the body. It must also engineer specific proteins called antibodies, which are created by white blood cells called B lymphocytes. These are programmed to recognise the intruder and stick to it, like pieces of a jigsaw, hindering its movements and attracting more white blood cells which can 'eat' the infectious agent.
In some cases, however, the body does not have a few weeks to wait, and the disease can cause irreparable damage, or even death, before the immune system has managed to get into gear.
Once our immune system has defeated an invader it will remember it for next time, and be ready to immediately launch into an all-out offensive. That is because some B lymphocytes that have already met their target can persist in our body for several years and, upon second contact, proliferate extremely rapidly, with each cell secreting antibodies at very high rates (up to 10,000 molecules/second!). In most cases, this response is strong enough to eradicate the recurring infection in very little time. Vaccines allow us to effectively skip the dangerous first infection.
Types of vaccines
With the administration of a vaccine, our body is exposed to a weaker, dead or dismembered form of the infectious agent. In this way the immune system has all the time to develop an effective and specific response so that, if and when the infectious pathogen enters the body a second time, our reaction will be ready to go.
 |
|---|
Historically, the antigen contained in a vaccine can be a diminished or inactivated pathogen, or a part of it (see below). However, thanks to the application of the biotechnologies, more types are emerging. For an extended list of the types of licensed vaccines, please consult reference [1].
An attenuated vaccine contains a pathogen that, although living, is made non-pathogenic through the introduction of some modifications during the manufacturing process. Generally, the pathogen is let replicate for several generations on certain cell lines or tissues so that it evolves to survive easily in these "unfamiliar" conditions. Thus, the more the pathogen is kept in these conditions, the more it becomes adapted to this comfortable situation, and therefore less adapted to human cells. As a result, the debilitated infectious agent is still able to infect human cells, but it spreads within our body slowly enough to give our immune system all the time needed to develop effective reactions [2, 3].
Some of these attenuated vaccines are those against rubella, mumps, measles or chickenpox, as well as against some bacterial pathogens (e.g. typhoid or BCG vaccine).
Because there is a risk -although quite small- that the agent reverts to normal virulence (i.e., normal rates of replication), in some attenuated vaccines pieces of the microorganism's genome are "cut out" with molecular techniques to further weaken the pathogen [2, 3].
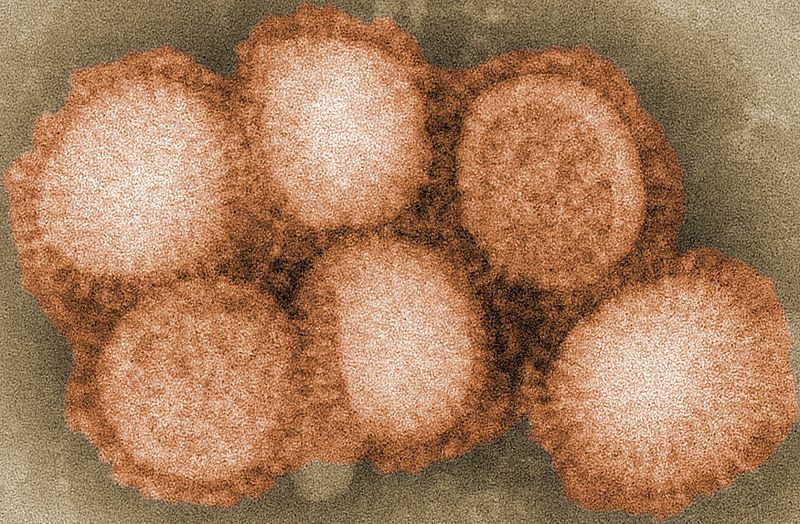
An inactivated vaccine includes microorganisms that are first grown in culture and then killed through heat or chemical treatment with formaldehyde or other agents. Being dead, these particles have completely lost their ability to replicate.
Although these vaccines are overall safer than the attenuated, they activate the immune system in a weaker way, making it a necessity to administer the vaccine repeatedly throughout time. The polio and influenza vaccines represent examples of inactivated vaccines against viruses [2, 3].
 |
|---|
Last, subunit and synthetic vaccines aim to elicit immune responses against a given infectious agent without the administration of the whole pathogen but only parts of it. In particular, subunit vaccines (e.g., Hepatitis B vaccine) aim to administer and elicit a response only against a portion of the pathogen that is most exposed and therefore vulnerable to the immune system. Synthetic vaccines, which are still under development, would take this principle even further, with the administration of only the fraction of the protein that is targeted by the immune system with the highest effectiveness [2, 3].
What else goes in a vaccine?
Besides the pathogen, vaccines contain other compounds that stabilise and maintain the preparation, or boost the immune response.
Preservatives
A preservative is a substance that can be included in products like food and drugs to prevent deterioration due to fungal or bacterial growth. The use of preservatives in some vaccines has been approved since the 1930s to prevent contamination, and the Center for Disease Control (CDC) now lists a total of three possible molecules that can be included in vaccine preparations for this purpose: phenol, 2-phenoxyethanol, and thimerosal [4]. However, some trace amounts of other molecules can remain in the vaccine from the manufacturing phase (e.g. formaldehyde, see below).
As a large quantity of information (both true and false) has been circulating about thimerosal, raising public apprehension due to its content of mercury, I will spend a few lines to review some of the large amount of information found in the literature about this component of vaccines. [5, 6, 7, 14]. Thimerosal is a mercury-containing organic compound that has been used for many years in Europe, as well as in the United States and other countries. In the human body, thimerosal is quickly broken down into two products: ethylmercury and thiosalicylate. While the presence of ethylmercury precursors in vaccines has raised some debates due to the structure chemically related to the compound methylmercury, it is important to remember that the two molecules affect the human body very differently. Methylmecury, a compound naturally formed in the presence of mercury and found in fish or other foods, has the potential to accumulate and harm the nervous system. In contrast, ethylmercury (the one found in vaccines) is quickly processed and cleared out of the body. Due to its fast elimination, the accumulation of ethylmercury is very difficult at the doses present in some vaccines. Therefore, this compound is considered safe for people. However, due to unproved (note, unproved) safety concerns moved by associations and worried members of the public, thimerosal is no longer included in vaccines. Thimerosal is still used to prevent contamination of multi-dose influenza vaccines [5], however these preparations are rarely used.
Very tiny amounts of thimerosal are also present in two non-flu childhood vaccines, as a residue from the manufacturing process (DTaP and DTaP-H1b combination vaccine), similarly to what happens for formaldehyde (see below).
Stabilisers
Stabilisers [7, 8] are added to the preparations to make sure that the vaccine maintains its properties during transport and handling. The main factors that can corrupt the preparations are heat and variations in acidity. This may result in loss of antigenicity and/or infectivity in case of vaccines containing live, attenuated viruses. Among the most commonly used stabilisers are MgCl2 (Oral Polio Vaccine), MgCl4 (Measles and Respiratory Syncytial Virus vaccines) and gelatin (Influenza, MMR, Varicella, DTaP vaccines) [8].
Some concerns were raised after the description of rare allergic reactions to the gelatin contained in vaccines. However, patients with immediate hypersensitivity reactions to gelatin generally have a history of allergies to gelatin-containing food. For instance, a 17-year-old girl in California in 1993 had a severe reaction within 5 minutes of receiving a MMR vaccine. The girl then claimed that was "kind of like what happens when I eat Jell-O". Still, these events are so rare that in a large study that monitored the occurrence of anaphylactic reactions after the administration of 7.5 million doses of vaccines, the total estimated possibility of developing such responses was defined between 0.7 and 1.5 cases/million doses. That means that the patient would be 50 times more likely to be struck by a lightning in his or her lifetime [16]! Nevertheless, health care providers should be prepared to provide immediate medical assistance in case an allergic reaction occurs [7, 15].
 |
|---|
Adjuvants
As not all the vaccines can elicit an immune response strong enough to induce immunity against a given pathogen, some vaccines (especially those that contain only parts of the agent) include substances that aim to increase the immune response against the disease: adjuvants [9]. Alum, containing aluminium salts, is the most commonly used adjuvant. It is found in vaccines against hepatitis A and B, diphtheria, tetanus and pertussis, haemophilus influenza type B, human papillomavirus (HPV) and pneumococcus. Monophosphoryl lipid A is another adjuvant that is found only in the vaccine Cervarix for the prevention of HPV [9, 10], while squalene has been approved by health agencies in several European Countries [17].
Although some people raised safety concerns over the presence of aluminium salts in vaccines, it is important to note that aluminium is an extremely abundant and widely distributed element easily found in rocks, the soil, water (as much as 0.1 mg/liter), as well as air and food. As a result, everyone is constantly exposed to some levels of this metal during their life [9]. As with most elements and molecules, exposure to high doses of aluminium can cause harm. However, the very small amount of aluminium found in vaccines (~ 0.85 mg/dose) is nowhere near an intoxicating quantity, especially considering that the average person in the United States eats from 7 to 9 mg of aluminium per day in their food (especially coming from flour, baking powder, colouring agents and anticaking agents). In any case, most aluminium in food, water and medicines leaves the body quickly in the feces. The quantities that enter the bloodstream will rapidly leave the body in the urine.
In Europe, the European Medicines Agency (EMA) has also approved squalene as an adjuvant for vaccines. Squalene is a natural substance that is found in plants, animals and humans too: assembled in the liver, this compound circulates naturally in our bloodstream, at many times the concentrations found in vaccines. This is why it is not possible to assess with certainty how much the levels of squalene in blood change upon administration of vaccines containing this adjuvant [18]. For pharmaceutical productions, squalene is extracted from fish oil, and an emulsion of this substance has been included in an influenza vaccine (FLUAD by Chiron) at about 10 mg/dose since 1997 in Europe. Although mild local reactions can be observed at the site of injections, squalene emulsions are considered safe [17].
Manufacturing residues
Some substances, although not intentionally inserted into the final product, can still be present in the vaccine in trace amounts from the manufacturing phases. Among them, formaldehyde, neomycin and albumin.
At room temperature, formaldehyde is a colourless gas with a pungent and distinct odour. Most commonly, it is a product of combustion and manufacture. However, formaldehyde is also found naturally, especially in the fruit and sometimes in rainwater. In addition, the human body itself produces formaldehyde, which is a product of its natural metabolism rapidly expelled through urine and breath. Although high levels of exposure can be intoxicating, no hazard for the public health has ever been linked to the trace amounts that are injected through vaccination [12]. To give an idea, the quantities of formaldehyde in a vaccine are so low, the amount of the chemical is 50-70 times higher in a newborn than the highest amount possibly found in a single dose of vaccine [11]!
Antibiotics can also be present in trace amounts (e.g. 25 µg/dose, that is down to 25 millionths of a gram) [8], as they are commonly added during the manufacture phase to prevent bacterial contamination. Because certain antibiotics can elicit allergic reaction in some individuals -generally manifested as hives, throat swelling, drop in blood pressure-, the antibiotics most likely to cause allergic reactions are not used during the manufacture phases of vaccine production [14]. Instead, the choice falls on neomycin, polymyxin B, streptomycin and gentamicin.
However, the quantities of antibiotics contained in vaccines are so small that they were never found to correlate with severe allergic reactions in vaccine-receiving patients. Therefore, the possibility of the antibiotics contained in vaccines to cause severe allergic reactions remains purely speculative [13].
Do I really need to vaccinate?
To conclude, many components are present in vaccines besides the substance that aims to mimic a circulating pathogen: stabilizers, preservatives and adjuvants that stimulate an optimal immune response. While it is understandable that a parent would want to know more about the components of vaccines, it is also true that a huge amount of false information circulates especially throughout the web, with people spreading unproved or debunked theories. In this article I reported peer-reviewed information supported by official resources and developed through the thorough application of no less than the scientific method.
Still, one may argue that they don't want to vaccinate to not run the risk of experiencing side effects, or because they are afraid that their child might experience an allergic reaction. However, is it safe not to vaccinate, or at least safer than vaccinating? Not according to the experts.
 |
|---|
Finally, vaccination comes with social implications: by agreeing to be vaccinated an individual is not only protecting him or herself from infection but is also contributing to the protection of their entire community. This is an important consideration as vaccination of some individuals is not possible, sometimes due to a particular medical condition.
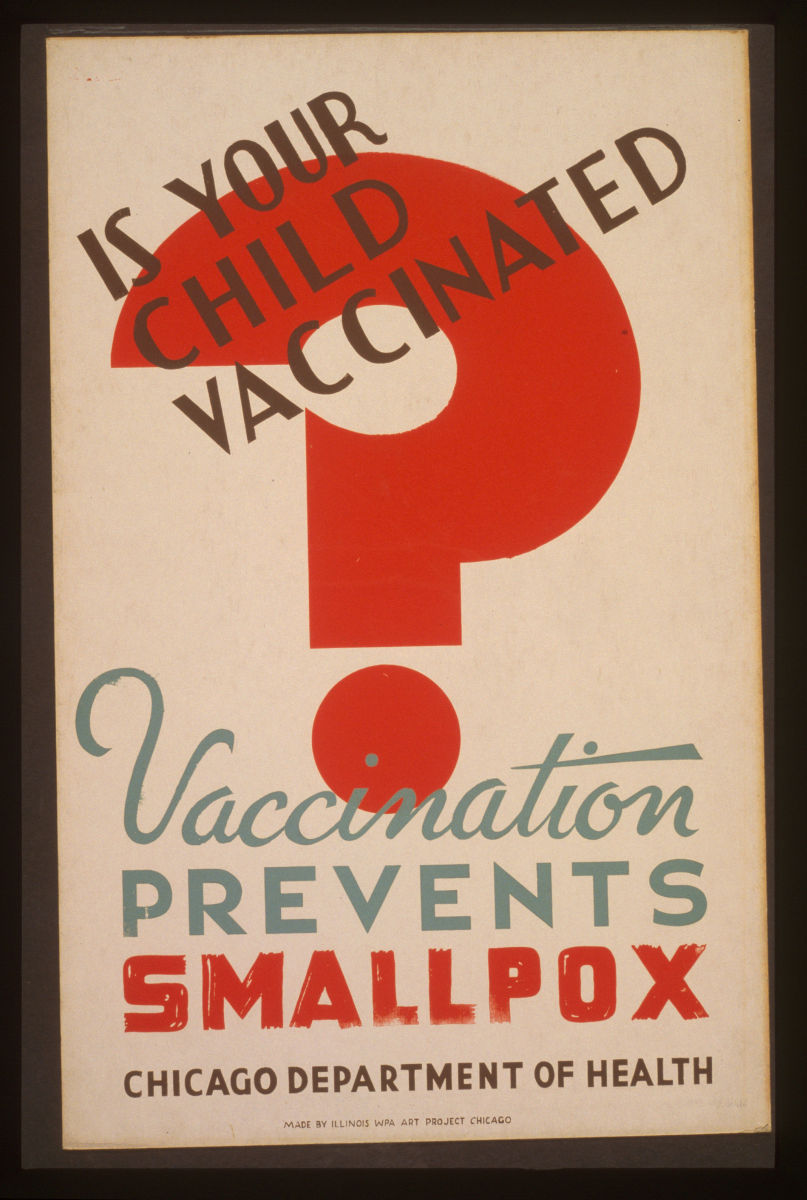
If the number of vaccinated -and therefore immune- people in the population reaches a certain threshold, the pathogen will rarely encounter new individuals it is able to infect. Although not every single person in the community is immune to infection, the remaining individuals are protected by the fact that virtually everybody they meet will not spread the pathogen. This phenomenon is known as "herd immunity". If this level of immunity persists, the pathogen will be unable to infect a sufficient number of hosts to sustain itself in the population, and will eventually be eradicated. Upon eradication there will no longer be a need to vaccinate against the pathogen. The eradication of smallpox was achieved in precisely this way, and experts believe there are many other preventable diseases for which the same outcome can be achieved, provided people continue to get vaccinations.
References
- Previous Where is my mind?
- Next Black hole jets stop stars forming





Comments
Add a comment