Every second your DNA is under assault - not just from chemicals in our environment or food, but from the hurly-burly of life within our own cells. We'll be finding out how DNA gets damaged and repaired, and how researchers are exploiting this to find better treatments for cancer. Plus, liver from skin cells, DNA from ancient teeth, and a scary little gene of the month.
In this episode
01:18 - What are carcinogens?
What are carcinogens?
with David Phillips, Kings College London
Kat - "Carcinogen" is a word you might hear in the media, but it basically means "something that causes cancer", and usually refers to things such as chemicals in our environment or food, or even things like UV radiation from the sun and sunbeds or ionising radiation such as X-rays. To find out more about these damaging agents, and how researchers are figuring out exactly how they cause cancer, I spoke to one of the UK's leading experts - David Phillips, professor of environmental carcinogenesis at Kings College London.
David - We know that most cancers have an environmental component to them. That something in the environment is causative or a causative factor in the disease. Evidence for this goes back to the 18th century when a London physician noticed that chimney sweepers frequently got cancer of the scrotum and he attributed this to their exposure to soot.
And in the intervening several hundred years, we've come a long way into understanding why, because soot contains chemicals that are carcinogenic and these have been identified. In the meantime, we've identified a lot of other environmental carcinogens, i.e. chemicals to which we're exposed environmentally which at least have the potential to cause cancer.
Kat - There's a big book on your desk and it looks like a huge thing listing all sorts of chemicals. Is it possible to put a number on them or can we broadly group carcinogens into different types?
David - Well, we can do both. There's probably several hundred chemicals which are known to be carcinogenic and this can be broadly categorised into various types. For example, tobacco smoke is a very complex mixture of chemicals, but at least 60 of those present are carcinogenic. Air pollution contains some of the same carcinogens, ionising radiation, non-ionising radiation, ultraviolet...
Kat - So, sunlight basically.
David - Yes, sunlight. It's a cause of skin cancer. Some products that are naturally present in plants, some that are produced by fungi, and many others.
Kat - If say, you were to look at the kind of damage caused by say, tobacco smoke and ultraviolet radiation from the sun, would it look the same or can you distinguish it?
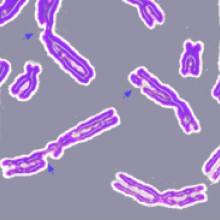
David - Well, there are signatures because when the DNA is damaged, that can lead to errors of replication, when the cell divides and replicates its DNA. And that will lead to changes in the sequence of the DNA which we call a mutation. If a mutation occurs in a critical gene, this can initiate the carcinogenic process. Cells have defence mechanisms against DNA damage. DNA repair mechanisms but sometimes these are bypassed or overwhelmed and mutation can result.
So for example, we now have the ability to sequence the DNA of tumours and it's been found over the last 15 to 20 years that tumours are full of mutations. The challenge now is to try and identify what those mutations have been caused by. Now, with the advent of whole genome sequencing to a practical level, it's now possible to sequence the entire genome of an organism whether it's a tumour or a test cell in the lab, and look at the mutations that have occurred across the whole genome. This may give us a more complete picture and a more diagnostic picture of the patterns of mutation caused by particular agents.
In the last year or so, work at the Sanger Institute in Cambridge has sequenced more around 7,000 different human tumours. They've come up with a broad categorisation that there are 21 particular types of mutation pattern that they've identified. In many of these cases, we don't know what's caused but we hope now, that if we can experimentally reproduce these patterns by taking some of the chemical carcinogens that we know or suspect of being carcinogenic, and seeing what type of patterns they produce across the whole genome in a test system, we may be able to identify the actual causative agent in more cases of human cancer.
Kat - So, you're going to take human cells, you take the chemical, you chuck it on it, then you look in the DNA and say, "Oh! That's signature number 13. That's what must be linked to that exposure."
David - Well essentially, it boils down to an experiment that's as simple as that, but obviously, it will turn out to be a lot more complex I'm sure. But in principle, yes, that's what we're hoping to do.
Kat - It seems like an incredibly powerful approach because often, you sort of hear people say, "Well, this type of cancer, we just don't know what caused it" or "Maybe it was this. Maybe it was my job. Maybe it was something I ate." Do you think we will be able to narrow down to an individual person's cancer what might have caused it?
David - That's the hope, yes. There's already a proof of principle here because it's now known that many cases of urothelial cancer worldwide can be attributed to ingestion of a plant carcinogen called aristolochic acid. This is present in plants that are accidentally ingested for example in the Balkans, but it's also a compound that's been widely used in Chinese traditional medicines. So, large numbers of people have been exposed to this. This produces a particular mutagenic mutation signature in urothelial cancers. Because we know a fair bit about the actual biochemical properties of aristolochic acid itself in experimental system, we can definitively say that in some cases, this pattern is what is seen in the human cancers.
In some cases, it may turn out that the pattern does not match that of the agent. In which case, one can say that that particular cancer, even though we suspect it might be due to the exposure, we can actually rule out that exposure. So, it can work both ways. We may be able to identify what's caused somebody's cancer, but also, in other cases where we suspect something that have caused it, actually say, "No, it didn't."
Kat - That also opens up some cans of worms. You can imagine if someone finds out their cancer has a signature of this chemical, maybe they could sue the person that exposed them to it, or made it, or put in the environment. Do you think there are implications for those kinds of public health issues?
David - Yes, I'm sure there are because one of the problems you have with identifying a cause of somebody's cancer, if it's down to something environmental or occupational, is that it's many decades from potential exposure to disease. And actually, tracking back and saying whether this was in fact the cause of the cancer can be extremely difficult. So, this may actually be quite helpful in actually pinning down whether an occupational or environmental exposure has been the cause or not, yes.
Kat - Working in a field like this where you're talking all the time about carcinogens and nasty chemicals, does it make you paranoid at all?
David - I wouldn't say paranoid, but I'm as concerned to live in as clean an environment as I can as the next person. So, from that point of view, I'd like to think that I try to avoid, where it's a matter of personal choice, exposure to carcinogens. But of course in many cases, it isn't. I live and work in London. London is a mega city. Mega cities have air pollution, so I'm concerned about the level of air pollution in cities certainly, and I would wholeheartedly support efforts to reduce the level of air pollution in the cities for example. That can really only come from governments and local councils implementing policies that will reduce this level of air pollution for example in urban environments. But these things are at least possible. If not, easy.
Kat - That was Professor David Phillips, from Kings College London.
09:47 - How DNA gets damaged
How DNA gets damaged
with Prof Dan Durocher, Samuel Lunenfeld Research Institute, Toronto
Kat - It's not just things in our environment that can damage our DNA - the damage can come from within too. Professor Daniel Durocher, from the Samuel Lunenfeld Research Institute at Mount Sinai Hospital in Toronto, Canada, explains more about how DNA damage is caused and how it gets repaired.
Daniel - DNA can be damaged as a consequence of our own metabolism. When we age, we'll produce for example reactive oxygen species which are small chemicals that are very reactive and they can interact with DNA and damage DNA. Actually, there's a theory of ageing that suggests that it's this chronic accumulation of damage of DNA that causes ageing.
Kat - But obviously, we need oxygen to be alive, to breathe and to make energy. So presumably, there's nothing we could really do about avoiding this kind of damage.
Daniel - Absolutely. That's why cells have evolved repair pathways to counteract those. They're in effect, the fountain of youth in some ways.
Kat - So, our DNA is always going to get damaged, so we have to repair it. How are some of the ways that cells figure out that they've been damaged and then repair them?
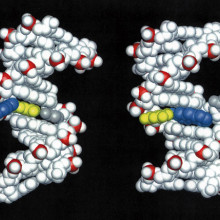
Daniel - That's exactly what my lab is interested in. And we're very interested in actually, the more severe form of damage which is the breakage of DNA. So, when the DNA double-helix is broken, it needs to be detected and then repaired. Just like those alarm signals that gets triggered when DNA is broken, this alarm signal will bring in the repair man. One that's very topical at the moment in the fields is that there are many different ways to repair breaks and the selection of the right repair pathway or the right set of repair men has a profound consequence on survival of the break and also the integrity of the chromosome - the fidelity of the repair.
Kat - So, it's not just recognising that you had a problem and repairing it. It has to be the right kind of repair. So, how many different ways can these breaks be repaired?
Daniel - So, there are two main ways that are mutually exclusives. There are also minor pathways, and they're very fundamentally different. For example, the tumour suppressor BRCA1 which is mutated in the familial breast and ovarian cancer, its function now appears to be to actually direct the repair path which was one type of repair by essentially antagonising the other ones. So, there seems to be a tussle between the different repair pathways that operates and it seems important in breast cells that it's the pathway promoted by BRCA1 that wins.
Kat - So, this is the gene that's faulty in many inherited types of breast and ovarian cancer.
Daniel - Absolutely.
Kat - And then what's the other type of pathway then that's important, maybe in other types of cells?
Daniel - One pathway that's very important is a process that has a very big name called non-homologous end joining (NHEJ). This actually is very simple, conceptually, it's taking the broken DNA molecules and gluing them together.
Kat - So, just any old ends, it'll just stick this together.
Daniel - Exactly, but that's actually the main repair pathway that we have in most of our cells. If you are not proficient in this pathway, you will be very sensitive to DNA damage. But also, you'll be immune-deficient because one thing that's remarkable is that our B-cells and T-cells use DNA repair to generate diversity in our immune system. And defective NHEJ leads to essentially very severe immune deficiency.
Kat - This is a great bit of multitasking then by the cells that the same process that's bad and damaging. Breaking and sticking back together is actually how we generate some of our immune responses. How far are we to actually understanding this process of DNA damage, detection and repair, and how it's involved in diseases like cancer and immune diseases?
Daniel - We've made great inroads in the past 15 years, but we're still a long way to go. I think we've identified the lot of the main players and the main components. Now, it's really trying to understand how this choreography of alert signals and repair factors come in and interact with each other and how all this is integrated in the larger physiology of the cell.
Kat - What's the really big unanswered question for you? What do you really want to know now?
Daniel - Really, I think the really remarkable result recently was, the function of BRCA1 tumour suppressor which is defective in familial breast and ovarian cancer. One of its main functions is to really act almost as a traffic policeman, directing repair in one direction or the other. Exactly, how this works is completely unknown. It's very germane for our understanding of familial breast cancer. I think that is at the moment, the biggest question in the field.
Kat - Do you think this is going to prove to be a really fruitful pathway for these kinds of treatments in the future?
Daniel - I think it will be because at the core, cancer is a disease of genetic alterations. These genetic alterations come from faulty DNA repair. So actually, using our knowledge of DNA repair will allow us to really target the core defect of cancer cells.
Kat - That was Professor Daniel Durocher from the Mount Sinai Hospital in Toronto.

15:21 - Liver from skin
Liver from skin
A breakthrough from researchers in California could provide a solution to the desperate shortage of donor organs for liver transplants in the future. Writing in the journal Nature, the scientists managed to turn skin cells into fully functioning liver cells, using reprogramming techniques. Previous research aimed at generating liver cells has focused on turning skin cells back into very basic stem cells, known as induced pluripotent stem cells. But liver cells made from these stem cells don't grow in the lab, so they can't create new liver tissue in the amount that would be needed.
In this new paper, the researchers didn't turn skin cells back so far. Instead they used a cocktail of molecules to convert them into a more advanced type of stem cell called an endodermal progenitor. These progenitor cells could then be programmed into liver cells that grew in the lab and in mice when they were transplanted into them. Two months after the transplant, it looked like the cells were becoming mature, functional liver cells, and nine months later they were still going. It's still early days for the approach, but one day it might be a viable alternative to an organ transplant for people with liver failure.

16:32 - Gene for butterfly wing patterns found
Gene for butterfly wing patterns found
US researchers have discovered that a single gene controls the complex wing patterns in female swallowtail butterflies - animals known for their mimicry of other toxic butterfly species, to avoid being eaten - publishing their findings in the journal Nature. The gene, called doublesex, is already known for being involved in controlling sex differences in insects, but the scientists have found that it's responsible for the butterflies' wing patterns too.
The discovery is surprising as such complex patterns might be expected to be the result of many genes working together, rather than just one. To find the gene, the researchers carefully mapped the DNA of more than 500 butterflies, and sequenced the genomes of 30, looking for specific genes linked to mimicking wing patterns. Further experiments showed that the gene is switched on exactly in the same places as the resulting pattern on the butterfly's wings. It's particularly interesting that the gene is involved in wing patterning and sex differences, as only female swallowtails show mimicry, so there may be a broader importance for the gene in determining the difference between male and female butterflies.
17:37 - Ancient tooth microbes
Ancient tooth microbes
A team led by scientists from Switzerland, Denmark and the UK have unearthed a so-called 'microbial Pompeii' on the teeth of 1,000 year old skeletons. Publishing in Nature Genetics, the researchers found that ancient humans' teeth were plagued by the same kinds of bacteria that bug us today, despite major changes in diet and dental hygiene.
By studying bacteria and food particles buried in plaque on the skeletons' teeth, the scientists were able to figure out what these people may have eaten, and more about how they might have lived and died. Today, more than one in ten people around the world are affected by gum disease - just as these ancestors were - and it's linked to major illnesses such as stroke and type 2 diabetes. So understanding more about how the bacteria in our mouths have grown with us might yield important information for human health in the future.

18:41 - DNA repair, and cancer
DNA repair, and cancer
with Professor Steve Jackson
Kat - Now it's time to look in more depth at the processes of DNA damage and repair. Professor Steve Jackson, from the Gurdon Institute at the University of Cambridge, told me more about the scale of DNA damage that goes on in our bodies and how researchers are trying to exploit DNA repair mechanisms to come up with new approaches for treating cancer.
Steve - A very important part of our cells is the DNA in the nucleus of the cell. That contains all of our genetic information that basically makes us the way we are and makes our cells in our bodies work in the way that they do. The information in the DNA is very valuable to the cell. Unfortunately, there's a lot of agents in the environment and made within ourselves and within the body that are continually damaging DNA. A good example of this is ultraviolet light from sunlight. That will damage DNA. It could produce a lot of DNA damage. But also, even the oxygen in the air at some level will oxidise DNA and then there are other reactions, other processes within ourselves that continually having effect by damaging the DNA.
If that DNA damage is not repaired, that's corrupting the genetic information. If our cells don't repair the DNA damage, they'll stop functioning correctly. And so, it turns out that over the course of evolution, our cells and the cells of other organisms have developed ways of detecting DNA damage and repairing it. In most cases, that makes the genetic information back to its original state so our cells continue functioning.
Kat - What sort of scale are we talking about this problem? Is DNA damage very common or is it something that's very rare in the lifetime of a cell?
Steve - I think people will all be aware of the fact that if you sit out in the sun too long, you can damage your cells and that's DNA damage or if you expose yourself to, let's say there's an unprotected radiation source, of course, those things will generate DNA damage. But there's a large amount of DNA damage taking place in our cells all the time. So, every cell in our body has around 100,000 DNA lesions per day at rest. So, if you sit in a darkened room away from UV light, away from radiation, still, every one of the cells in your body is having 100,000 breaks or damages to the DNA a day.
Kat - That's an incredible amount of damage. How do cells cope with this? How do they even detect that much damage?
Steve - Well, DNA has a fairly regular structure - the DNA double-helix - and most of these damages change that structure. So, there are certain specialised proteins, molecular policemen if you like, going through our cell, looking at the DNA, and not doing very much when the DNA is normal. But this surveillance pathway is basically ready to pounce on any bits of damaged DNA. So, if the structure of the DNA changes through DNA damage, these proteins bind to it and set off the alarm bells.
Kat - What sort of things are involved in sending these signals to cells? What calls in the repair men?
Steve - So, if you like, the damage is recognised by certain proteins that sit on the DNA and basically then serve as landing pads or recruitment pads for other proteins come in, and in some cases, cut out the bad bits of DNA and then fill in the right sequence of the DNA, and then basically ligate the bits back together again. So basically, like a molecular tool kit which is called in at the right time and at the right place.
Kat - What are the implications if this process doesn't happen correctly?
Steve - Well, if it doesn't happen at all, our cells will very, very rapidly die because the DNA would basically be mutated away. Most DNA damage, maybe all DNA damage is repaired, but sometimes it's repaired in an error-prone way. So, the original sequence is changed and that can give rise to a mutation. That's what a mutation is - the change in the DNA sequence.
Some of these mutations are fairly innocuous, but other ones will cause a cell to have major problems because he's not now able to do the right thing at the right time. So, that in some cases could cause a cell to die and other cells, that could stop the cell responding to the environment and that might cause it to grow when it shouldn't grow, and therefore, be one step towards being a cancerous cell. In fact, we now know that just about every cancer, during the course of its evolution into being a cancer, has got mutations.
Kat - And now, we know there are some ways that we can use these repair pathways to actually treat cancer. What's this approach?
Steve - Yeah. So normally, DNA repair is a very good thing and you wouldn't want to inhibit DNA repair with for example, a drug. But in some circumstances, you can imagine how using a DNA repair inhibitor can be very useful to help kill cancer cells. For example, combining a DNA repair inhibitor with radiotherapy or chemotherapy which are common treatments for cancer. Radiotherapy and chemotherapy would, by causing DNA damage in cancer cells and if you could slow down the repair in cancer cells, you're going to be able to kill those cancer cells more effectively.
In addition, there's another way you can use DNA repair inhibitors by taking advantage of some of the key differences that exists between cancer cells and normal cells. It turns out that most cancer cells are not particularly good at repairing DNA damage because they've lost some of their repair mechanisms. That means that a cancer cell that's lost one way of repairing DNA damage is very reliant on the other pathways that it still got. What my colleagues and I, over the last few years, have learned this that if you can come up with a drug targeting that pathway, that the cancer cell is really reliant on, you can kill the cancer cell because it can't repair its DNA whereas normal cells are not affected anywhere near as much because they have multiple ways of repairing the DNA damage.
So, if you like, we're trying to use this difference in DNA repair between cancer cells and normal cells as an Achilles heel of the cancer cell to kill the cancer cell without having very much effect in cancer patients' normal cells. That's a concept that we initially established in the test tube, in cell culture in the lab. This type of approach is now showing great promise as a real treatment for certain subsets of cancers, particularly breast and ovarian cancers.
Kat - So, in the future, do you think we could be combining treatments like chemotherapy and radio therapy with these DNA damage inhibitors to make a real difference to the effectiveness of treatment?
Steve - Yes, so of course, these things, particularly when you're combining drugs, don't take place over night. You have to be very careful how you combine different drugs. But I think there is a big potential there. There's a potential for DNA repair inhibitors being used as standalone agents, to kill cancer cells that are deficient in certain repair pathways, and then there are opportunities for combination use. All of these are now being explored in various clinical trials.
Kat - That was Professor Steve Jackson from the University of Cambridge.

Can retinitis pigmentosa be cured?
Kat - And now it's time for our monthly question. Listener Joe Devin asks, "Some years ago, it was announced in the news that someone had been cured or partially cured of Retinitis pigmentosa using gene therapy in a US laboratory, but I have never heard any follow-up to this announcement, and it seems that nothing has ever come of the stem-cell technique that was used. What has been going on in this field of research, and is there any concrete hope for a cure for the disease?" To find some answers, I spoke to Professor James Bainbridge, professor of retinal studies at University College London and consultant at Moorfields Eye Hospital.
James - There's been a lot of progress in this area over the last few years and we and others have shown that in a certain condition, it does seem to be possible to actually improve aspects of sight by providing people with normal copies of the genes that they otherwise lack.
Kat - Particularly in the case of retinitis pigmentosa, where are we with gene therapy for that particular disease?
James - So, retinitis pigmentosa is a term that describes a degeneration of the retina typically because of an inherited defect, inherited disorder. This particular term refers to many hundreds of different conditions, all of which depend on a specific gene. We are excited because there is increasing evidence that for at least one form of that condition associated with defects in one particular gene, provision of a normal gene through gene therapy does appear to confer some significant benefit. The challenge now is to try to find out how that can be extrapolated, if you like, how that technology can be used to provide a similar level of benefit or perhaps even more robust and more durable level of benefit for people who have different forms of a similar condition.
Kat - Do you think that this gene therapy approach is a hope for a cure in the future?
James - Absolutely. I think that we're very confident that this technology will offer some benefit for people with specific forms of inherited retinal disease. We don't know yet the extent to which people might benefit or for how long, and we don't know whether this particular treatment can prevent people from losing sight altogether. But it would be fantastic to think that it could protect them by slowing degeneration and perhaps protecting their sight for longer than they can otherwise expect.
Kat - What kind of timescale are we looking at?
James - So, a lot of this work has been done in the laboratory using models of these conditions. But we're very excited that we are already well into the stage where these technologies are being used in people with blinding disorders. So, there are a number of clinical trials now involving people poor sight who are already benefiting from this technology. At the moment, the people who have been included have - and it's important to emphasise this - very specific forms of the condition because we only have tools to intervene in a very limited number of these conditions. But we hope in the future, that we might be able to expand the portfolio of treatments so that more people can benefit.
Kat - Thanks to Professor James Bainbridge for that answer. And if you've got any questions about genes, DNA and genetics, just email them to me at genetics@thenakedscientists.com.
28:05 - Gene of the Month - Gremlin
Gene of the Month - Gremlin
with Kat Arney
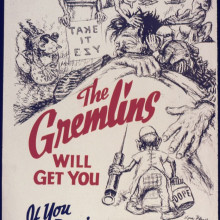
And now, it's time for our Gene of the Month - and this time it's Gremlin. Sharing a name with the cute but havoc-wreaking creatures in the classic 80s film, Gremlin was first discovered in frog embryos in the late 90s, and versions have been found in other vertebrates including mice, chickens and humans. The protein made from the Gremlin gene interferes with molecules known as Bone Morphogenetic Proteins, which - as the name suggests - are involved in shaping bones as an animal develops in the womb.
Gremlin is known to be involved in shaping the bones of hands, paws and wings, and is also involved in the development of the complex network of tubes that make up the lungs and liver. It's also implicated, along with another gene called Noggin, in the shaping the bones of the skull, and there's also evidence that Gremlin can encourage the growth of cancer cells. Unfortunately there's no data on what happens if you get the gene wet or feed it after midnight.










Comments
Add a comment