This month we've got a special bonus-length podcast commemorating twenty years since the birth of Dolly the Sheep, the first mammal cloned from an adult cell. Her birth changed the scientific world, and led to the development of other transformative technologies. Plus, our gene of the month is keeping a straight face.
In this episode

01:04 - Ian Wilmut - Cloning Dolly
Ian Wilmut - Cloning Dolly
with Ian Wilmut, MRC Centre for Regenerative Medicine
Kat - I was at university when I first saw the issue of the journal Nature sporting a rather surprised-looking sheep on its cover. Announced to the world in February 1997, the birth of Dolly the sheep rocked the world. Her birth actually came a few months earlier, in July 1996, so to celebrate, the Roslin Institute in Edinburgh - where she was cloned and born - and the MRC Centre for Regenerative Medicine decided to throw a party, or rather a scientific symposium in her honour. I was lucky enough to be able to go along, and even more lucky to be able to speak with Sir Ian Wilmut, who led the team responsible for the creation of Dolly. I started by asking him to explain the history of the research leading up to her birth.
Ian - The very earliest experiment was trying to answer a biological question as to whether essentially, all of the cells retain the same DNA during the course of development. Because there was a suggestion - a hypothesis - that development was brought about, differentiation was brought about by the loss of sequences which were not important for a particular tissue type. A series of very simple experiments were done to address that question and the answer was, there was no evidence of DNA being lost.
Kat - So this is the idea that somehow cells are shedding genes as they're making decisions to become brain or muscle, what was the key experiment that showed that couldn't be the case?
Ian - The nuclear transfer experiments which were done by Briggs and King and subsequently by John Gurdon demonstrated that you could take differentiated cells from tadpoles and produce adult frogs from them. So that clearly showed that those differentiated cells still had all of the information necessary to control development.
Kat - But they never managed to go from an adult cell to another adult.
Ian - That's a really intriguing point, but I think you can only suggest that there must be something different in the way in which gene expression is regulated and that whereas we have methods which overcome these now for early stages of development, we haven't yet got that for adult frogs.
Kat - So, that was frogs and you thought, "Okay, let's try this in sheep." Why sheep? What was the background to that?
Ian - We got started because I heard that Willadsen had cloned from blastocysts in cattle. What I was looking for was a way of having cells at which we could culture for a while to allow you to make precise genetic change and then use its nuclear donors. It seemed, if he was growing cells from blastocysts and the cloning from them then maybe we were reaching that point.
Kat - So that's taking cells from a very, very early embryo, putting them into an egg and making another animal. So the idea was, can we do this from cells in a petri dish?
Ian - Yes, exactly.
Kat - Tell me first then about Megan and Morag because those were actually sheep before Dolly. Where did they come from?
Ian - They came from cells which had been cultured with the hope of getting embryo stem cells by my colleague Jim McWhir. What he found was that not that the cells multiplied vigorously and differentiated but the cells that we were looking for simply ceased to be there. They just disappeared. So we did an experiment taking cells from different days of culture to try to see whether we could confirm this interpretation by having success with probably about day 9 embryos. But if we went through to day 10 and 11, then they've lost the ability to support development because they've either disappeared or changed.
Kat - So Megan and Morag were sheep that were cloned from this very early embryo cells. What about Dolly? Tell me about her biological history.
Ian - Well, the classic thing for developmental biologists to do when they're studying these sorts of mechanisms is to look at very early stages, foetal tissue and then adult tissue. So we always had it in mind that we would progress along that sequence of development. As you say, we'd worked with early stages, we worked with foetal cells. Because we'd been successful with those early stages, we started with adult tissue.
Kat - What was the adult tissue that you used to clone Dolly?
Ian - It was mammary tissue. Our collaborators, PPL Therapeutics, you remember the project to make sheep that producing their milk proteins needed to treat human disease. They were growing mammary cells in the lab as part of that project so they knew how to grow them. They knew that they had a normal karyotype and were likely to be suitable nuclear donors.
Kat - So then to create Dolly, just if you can really briefly explain the process, how does it work? What is cloning? How does it work with an adult cell?
Ian - You need two cells. you need an egg from which you remove the genetic information, the chromosomes, and you need a nuclear donor which will provide the nucleus that controls development. So in the case of Dolly, this was a mammary cell which was in culture which was used and proved to be able to control development.
Kat - Presumably, people had tried to clone from adult cells and it hadn't worked. Why did it work with Dolly? What was special about those experiments?
Ian - I don't know if anybody actually had tried adults in mammals. What happened to people I think was that they tried with very early stages and it worked but as you began to work with cells from cells partway through pregnancy it didn't work. So there was no point in going through it to adult.
Kat - So just, it's not worth bothering trying.
Ian - It's not going to grow, yeah.
Kat - What did make the difference that seem to make it work?
Ian - What we did as preliminary work was look at the best way to coordinate the cell cycle of the two different cells. we came forward with a scheme of using cells which had donor cells which had been serum starved in order to make them quiescent.
Kat - This is kind of just put them to sleep basically.
Ian - Yeah, exactly. And also oocytes which were in metaphase 2 because we knew that they had a great potential to stimulate to transfer nucleus to enter into the cell cycle in such a way that it might well also be able to reprogram this expression of genes in the nucleus at the same time.
Kat - So you've got the donor cell that's quiet, it's all asleep, it's not doing anything, and you've got an egg cell that's really ready to go for it. That's the key.
Ian - That's exactly it.
Kat - When Dolly was born, how did you feel? That must have been incredible.
Ian - Yeah. I think we were almost shocked because it was such a novel thing. We knew how important it was going to be, both immediately from the point of view of the media and from a career point of view from the point of view of building a reputation for the group.
Kat - This may seem like a bit of a silly question but what was she like?
Ian - The best way to describe this, I live down in the borders, in amongst sheep farmers. If they have a lamb which is not being mothered either because its mother has died or she's got too many lambs, they take it into the house. It becomes accustomed to people and that's exactly what happened to Dolly. There were so many people visiting and wanted to see her, to get her to be in photographs and this sort of thing that she became accustomed to people. She came forward to people where there's no - as it were, no ordinary farm sheep would do that. It would automatically turn and run.
Kat - What happens to the rest of her life? I understand she ended up having her own lambs. They weren't cloned, were they?
Ian - She had six lambs by normal reproduction. I'm pleased to say were all healthy. One of the rules of thumb for cloning is that if an animal has an abnormality but can breed then its offspring will not inherit the abnormality because it's likely to be an inappropriate expression of a gene rather than the loss of a gene. And the reprograming will restore their function to normal.
Kat - So she became a mum and then what happened to her? How long did she live for?
Ian - Six years.
Kat - That's quite short for a sheep.
Ian - But we euthanized her because sadly, there is a virally induced cancer which occurs in sheep particularly in Scotland as it happens. The infection got into the flock and unfortunately, there is no treatment for it. So after she'd had it for a number of months, we decided it was time to euthanize her because what happens is the tumour got so large that it restricts the animal's ability to breathe then only kind to end their life.
Kat - Absolutely and where is she now?
Ian - Now, she's I think one of the most frequently visited exhibits in any British museum. She's in the National Museum of Scotland.
Kat - You are the father of Dolly I suppose, scientifically speaking at least. What do you feel has been her key scientific legacy and your key scientific legacy?
Ian - She made biologists think differently because we showed that cells can be changed. Many members of your society will know that Shinya Yamanaka who was awarded the Nobel Prize because of the work that he did to take advantage of this new knowledge to develop ways of changing cells and reprograming cells. He says himself that he was stimulated to start the project because of the birth of Dolly. And his work then led to the development of methods to produce iPS cells. So I may be the father of Dolly but I think I'm the grandfather of iPS cells.
Kat - Ian Wilmut there. And in case you're wondering, Dolly was indeed named after the country singer dolly Parton, due to her origins from a mammary or breast cell.

10:20 - Shinya Yamanaka - Special stem cells
Shinya Yamanaka - Special stem cells
with Shinya Yamanaka, CiRA Kyoto Japan
Kat - Also at the symposium, we heard from another pioneer of biology - Shinya Yamanaka, who won a Nobel prize for his discovery that just four molecules could convert any type of adult cell back into so-called induced pluripotent stem cells, which have the ability to become any type of tissue. And, as he explained to me, his research was directly inspired by Dolly.
Shinya - So, I was a physician a long time ago. I couldn't help many patients suffering from intractable diseases, including my own father. So that was why I changed my career from physician to a scientist. Because I thought, I believe it is basic medical science which in the future can help those patients suffering from intractable diseases. I did not expect I would work on stem cells when I started my scientific career. But because of many unexpected results of my experiments, I became interested in stem cells and here I am now.
Kat - So we're at the 20th birthday party I suppose for Dolly who was a sheep who was created by taking an adult cell, putting it into an egg cell, and then you could make a sheep. What did that tell us about cells that we didn't understand before?
Shinya - So Dolly really surprised us how flexible our cells are. Previously, we thought cell differentiation as irreversible.
Kat - Just one way - you go from egg to animal and that's it.
Shinya - Exactly. But because of the success of Dolly, we learned that it's not true. Differentiation is reversible. They can go back to the embryonic state. So by being inspired by Dolly, I started a project in which I tried to make embryonic stem cell-like stem cells. Not from human embryos but from adult somatic cells.
Kat - So, how did you start doing that? You've got these adult cells in a dish, you're looking at them going, "Okay, what do I do to you?"
Shinya - There was another previous work in which a scientist converted skin fibroblasts into muscle cells just by one factor. The factor is myoD. It's a transcription factor. By simply putting myoD, that factor into fibroblasts, Dr Weintraub was able to convert fibroblasts into muscle cells. So, that was another important lesson to me. We could convert cell fate by transcription factors. And also from Dolly, we learned that we should be able to reprogram cells back into the embryonic state. So, it's a combination of the two great previous studies which promoted me to initiate this project.
Kat - Because transcription factors, these are the molecules that basically turn certain genes on. They sit on the DNA, they turn genes on. So you've got that part of the puzzle, then you've got the Dolly part of the puzzle that tells us that you can go from one to the other. So then you just have to find the factors. How did you find those four factors, your Yamanaka factors that can turn adult cells back into stem cells?
Shinya - So, I thought those factors that can reprogram cells back into the embryonic state - ES cells. they should play important roles in ES cells themselves. So in the first 4 or 5 years in this project, I spent most of the time to identify as many factors as possible that played important roles in mouse embryonic stem cells. so then we just combined multiple factors which we had at that time and test them, and luckily, we were able to identify those four factors. So, it was a combination of our hardwork and our good luck.
Kat - How did it feel when you looked in that dish for the first time and you were like, "This has worked!"
Shinya - Actually, we thought it must have been some kind of mistake - some contamination or some kind of error. So, we repeated the same experiment many times and it worked always. So then we were convinced it must be true. Science is very tough. In many cases, we found we did something wrong. So, in this very special moment, we couldn't be just happy. We were very careful.
Kat - Something's got to be bad somewhere.
Shinya - So actually we didn't toast.
Kat - You did some toasting maybe when you got your Nobel Prize for it?
Shinya - No, not yet. When we become able to help patients, that's when we're going to have some good wine.
Kat - So you mentioned helping patients because now, we can take adult cells, you could take say, a skin cell from you or from me, you can treat it with these factors, you can turn it into stem cells. and then what can you do with them? What sort of cells can you make from these iPS cells?
Shinya - So at least in theory, we can make any types of cells that exist in our body like brain cells, heart cells, liver cells. So the potential is enormous. Of course at the moment, it is still very difficult to make completely mature heart cells or liver cells from iPS or ES cells but many scientists have been working very hard. I really hope in the very near future, we can do it.
Kat - I see some things like using 3D printing with tissues, with cells. is that the sort of thing you could do with iPS cells as well one day.
Shinya - It's also possible. So, we could use like heart cells, muscle cells, other types of cells as inks of 3D printers. At the moment, it's still like a scientific fiction but after 10 years or 20 years, who knows? It may be possible.
Kat - Another thing that maybe seems like science fiction is that certainly in mice, we can take iPS cells and we can make germ cells. we can make eggs and sperm. Again, is that something that could happen in the future, your mummy and daddy could be skin cells?
Shinya - It's possible but again, we need to discuss with not only between scientists but also with the general public, and also couples suffering from infertility, regarding how much we can do our research. So our goal is to help patients but scientists alone cannot decide how much we can proceed. So it's a very naïve question.
Kat - I went to university and that first year was when the announcement was made about Dolly the sheep so my whole adult life as a scientist has been an incredible time. How does it feel to be working at the cutting edge of such an incredible and exciting field?
Shinya - Well, that's one of the reason why we do science. Science is full of surprise. It's unpredictable. In many times, it's very tough. Scientists are having a hard time almost every day but sometimes it gives us wonderful moment. So that's why we cannot stop doing science. That's the beauty of science.
Kat - Nobel Laureate Shinya Yamanaka, from the Centre for iPS Research and Application in Kyoto.

19:55 - Angelika Schnieke - From sheep to pigs
Angelika Schnieke - From sheep to pigs
with Angelika Schnieke, Technical University of Munich
Kat - You're listening to the Naked Genetics podcast with me, Dr Kat Arney, reporting back from the 20th birthday symposium for Dolly the sheep, held by the Roslin Institute and the MRC Centre for Regenerative Medicine in Edinburgh. Still to come, we'll be finding out how chickens could provide us with a lot more than eggs thanks to biotechnology. But first, it's time to hear from another member of the team involved in cloning Dolly. Angelika Schnieke is now chair of livestock biotechnology at the Technical University of Munich, where her research on pigs is helping to change our understanding of human diseases.
Angelika - Based on the technology which has been developed with Dolly, we can now genetically modify the pigs. So this is mainly used at the moment for models for serious human diseases and also xenotransplantation and now, we're also getting in an area where it's also available for agricultural applications.
Kat - So, let's unpick those three different things. Let's start with the human diseases? Why are pigs a good model for human diseases? Lots of people hear about using mice as models but why pigs?
Angelika - We have been working with mice for a long time because it was actually the only species where we could do genetic modification in for a long time. But of course, it also had been shown that a lot of results from the mouse cannot be transferred into the clinic. So still, we needed some other models and probably the best would be to work with apes which is not possible. So, what else is there which is sort of in the physiology, in the size and so similar to human, and the end product was a pig.
Kat - And are we talking about big pigs or little pigs? Mini pigs seem to be very trendy now.
Angelika - Yes. The big pigs are a little bit too big because they go into several hundred kilos when they're fully grown out. So, you work with many pigs or you can also work with F1s between them and then use somewhere in the mini pigs - 60 kilos and otherwise, sort of 80, 90 kilos, so quite human.
Kat - What sort of diseases can you study in these animals?
Angelika - Principally, all sorts of diseases which you also find in humans. So people are working on models for human cancers. They're working for cardiovascular disease, they're working on diabetes so all the main killers really. Plus, on top of it now also are rare diseases.
Kat - So, how do you go about studying a disease in a pig? How do you make a model pig?
Angelika - We look what experiences already in humans so do you know what the basis is for the disease? Have also the experiments been done already in the mice? And so, with that knowledge we can then really design our pig to have exactly the same genetic difference or alteration so that they might get the same disease as what you'll find in humans.
Kat - Can you give me a good example of that that you've managed to create in your lab?
Angelika - We work on cancer models. So, one of the most common cancer models is colorectal cancer. Another very serious cancer is the pancreatic cancer. And so, we're making models for both those cells.
Kat - Do they seem to recapitulate what the disease looks like in humans?
Angelika - What we have seen so far, we also have another model for osteosarcoma. So our colorectal cancer is just what you find in humans. It is different from the mouse but the mouse differs from human. So, we find the polyps and the tumours developing in the large intestine just like in humans and the mouse with the same mutation within the small intestine. We have the same for the osteosarcomas or the bone cancer that the places where the tumours appear are the same as in humans and again, the mouse is different. So it looks like at least for the tumours, the pig is a good model.
Kat - And then presumably, when you're trying to develop new treatments, understand the disease, you've got these animals right there in front of you that you can properly investigate that you couldn't do in the same way with a human.
Angelika - That is absolutely right. So you can take samples from the tumour, you can take samples from the blood then you can also look for biomarkers to do early diagnosis. Can you see some differences in your blood samples which might indicate what is happening inside the animal in the tumours and you can do this all the way through the disease progression.
Kat - You also mentioned another application of these modified pigs is xenotransplantation which just sounds like something you find in a science fiction film. What is it and what's the role of pigs?
Angelika - So xenotransplantation means that you move organs from one species to another. In this case, it would be the porcine organs or the porcine tissues into humans. So, most people know that we have problems with diabetes. Diabetes also means that we have a lot of kidney failure. There's an absolute shortage of kidney transplantation or to cure diabetes in with islet transplantation. So if you could not take the kidneys or maybe the heart or the islets from the pig and transplant it in humans, you could cure probably the serious diseases.
Kat - But why can't we do that already if pigs are so similar to humans in so many respects? Why can't we do that just from a pig?
Angelika - Well, you know that even if you transplant from human to human, you have to make sure that it is a good match. And there are some genes in the pig which are not there in humans anymore. And so, there is a rejection of the organ which happens very quickly. Those genes which causes these very fast rejections, we have to remove from the pig. So the organ can survive, we also have to have some other pigs where there might be a small discrepancy between humans and the pig system - maybe the blood coagulation system.
Kat - So you're trying to make the pig organs look as closely like the human organs at least to the immune system.
Angelika - At least to the immune system. That's absolutely right.
Kat - How long is it going to be before we can actually have these kind of organs that you could transplant into humans? What's going to be the first step this way?
Angelika - Actually, it's already happening in some ways. You have decellularised heart valves which are either from pig or from cows and they implant it into humans. But there of course, you have destroyed most of the cells so they should not be rejected. The next will be small tissues. For example, the islet cells because you can also encapsulate them. You can place them and you could also take them out.
Kat - These are the cells from their pancreas that make insulin.
Angelika - Exactly. They are the pancreatic cells which makes insulin. So that would be already quite a step forward. You can also imagine like corneas you could use and then it will be going into whole vascularised organs. They are a bit more difficult but hearts can already survive in the baboon for almost two years.
Kat - Maybe one day soon you could be walking around with a pig liver instead of your liver.
Angelika - Well, yes. I mean, you also have to imagine that you might not need the organ for your whole life. But if you had for example, eaten some poisoned mushrooms your liver might degenerate very quickly. But it could also regenerate. But in between regeneration, you might be dead. It would not be a good outcome. So what you really want is maybe sort of an ersatz liver.
Kat - Temporary liver.
Angelika - A temporary liver for the short time that your liver has time to regenerate.
Kat - I'd like one for Friday night when I go out drinking. Borrow one! In the final application you talked about was, use in agriculture. So could we have GM pigs being used in agriculture? Is that a good idea? How does that work?
Angelika - In my opinion, it would be a good idea. But it depends of course, what is your target, what would you want to change. We talked a lot about human diseases and how you can help the humans. But of course, we also have a lot of diseases in the pigs, infectious diseases. And so, if you could find out what are the receptors for those infectious diseases, can you alter them so you don't get the infection but the pig is still healthy or is a sheep or cow, make them more resistant to diseases. So you have something which is good for the animal, something which also will have a better product because you know you can have your meat, your milk and so on from healthy animals. So yes, I would think it is a good idea.
Kat - Is that the same kind of techniques that we've seen so adding genes in to these animals or changing the genes to make them more healthy?
Angelika - The technologies would be the same. So in most cases, you would probably alter the genes which are already there. You would not necessarily have to add new genes and you have more and more new technologies coming up. Genome editing is one of them, where you can make really sort of very fine, precise alterations of the genome.
Kat - The world heard all about Dolly the sheep. She was a cloned animal cloned from an adult cell. Everyone got very excited. But then a year later, there were some other very unusual sheep born. Tell me about them.
Angelika - It was right from the beginning the reason why we were interested in the Dolly experiment is because we had cells in cell culture. And cell culture also alters the cells and cell culture was absolutely the next question necessary. And so the next experiment was to introduce transgenes, in this case it was factor 9 which is one of the factors which is important for blood coagulation and people who don't have factor 9 are haemophiliacs. And so, we wanted to make the product in the sheep, milk the sheep and then treat the humans with it. and this was in the next experiment, added the gene to the cells, use the cells to make the animals and that was then Olly, Polly, Holly, Molly.
Kat - So that carrying on with the Dolly type naming theme.
Angelika - It was. Actually, when the animals were born, they were all males. It's the time Germany won in football, but the Scottish team was not very excited to name the animals after the German football. So, they decided on Olly, Polly, Holly, Molly.
Kat - The last question really, you were one of the team that worked on Dolly the sheep 20 years ago. What in your opinion has been her impact and really, how have you seen this field develop over that time?
Angelika - If you just talk about genetic modification in livestock the way we're doing it right now, it would not have been possible without the experiment on Dolly. Without having cells in culture which we can change and then make a whole animal out of those cells which are cultured, without that, the whole field wouldn't have really developed. I think another very important point is really that it has inspired people to think differently. So, some things which looked impossible before, now they became reality. It also makes sort of, you're looking at something which can be very exciting. Science can be very frustrating but from time to time, you have these little highlights and they sort of spark an interest in science, in sort of your adventurous Geist.
Kat - Angelika Schnieke from the Technical University of Munich.

30:50 - Lissa Heron - Playing chicken
Lissa Heron - Playing chicken
with Lissa Heron, Roslin Institute
Kat - While there was much talk at the symposium of mammals, the Roslin Institute's Lissa Heron is working with a different type of agricultural animal - chickens. Although chickens can't be cloned in the same way that mammals can, they can be genetically modified, meaning that their eggs might provide us with a lot more than a tasty breakfast in the future.
Lissa - Well, chickens are a really useful system. They've been used historically for studying developmental biology, development of the embryo. But they're also compared to large animals like sheep or cows. They're much easier to keep and you can keep a lot more chickens in the same kind of space that you would keep sheep. They're a lot cheaper to feed as well. They have a shorter life cycle, faster breeding cycle, and they're really easy to scale up. In terms of pharmaceutical production, the egg is a really great system because it produces a lot of protein. You don't need to disturb the hen really because you just take the eggs and that's it. and there's an easy way of now making the genetically modified chicken so that you produce a lot of whatever protein you want in the eggs. The other benefits of chickens are that they can make proteins that behave more like human proteins compared to some cells and some other mammals. And so, when you give these proteins to humans as a therapeutic, they are less likely to cause an immune response - a negative immune response and they're also more likely to be active compared to proteins made in other systems.
Kat - So, what sort of drugs, what sort of molecules are we talking about here that you could make in chickens?
Lissa - So, a lot of the classic drugs that people are familiar with like aspirin or paracetamol, these are small molecules that can be synthesised in a chemistry lab. But a lot of the newer drugs that are having a lot more success in treating cancers and chronic illnesses are actually proteins. The very first drug that was actually made this way on the pharmaceutical market was insulin. So insulin is a protein made by cells in your body and people who were diabetic can't produce this. And so, they used to have to purify it from animals. Obviously, a lot of potential for infections and other problems and also it's cruelty, you have to kill the animals to get the insulin. So, they started looking to see whether we can make this in bacteria. and fortunately with insulin, you can. It's a relatively simply protein. So they started making it in a bacteria and that way, you can have much greater control over the cleanliness of the protein and how safe it is. You can make little tweaks, the sequence, to make it more active or last longer in the body, all these sorts of things. So, once you got insulin successfully used in human patients, we started thinking, "What else could we make for patients?" more and more of these sorts of things have been coming up. So you have what are called monoclonal antibodies that target cancer cells. An example of that is Herceptin, and then you also have things like interferon alpha which is used to treat hepatitis and also various cancers. So you have all these sorts of proteins but a protein can't be synthesised. It has to be made in a cell system because it's a very complex biological process and it's a very large molecule. So, it needs to be expressed and it needs to be folded properly and some of them have to have sugars added to them and various modifications like that. So you need a more complex biological system to make them.
Kat - So, if that complex biological system is the chicken's egg, how do you get the genes that make the proteins into the chickens?
Lissa - We use a system called a lentivirus. This is a type of virus that is actually related to the HIV virus. These viruses are really useful because they're able to integrate into the genome of your target animal. They are not silenced like a lot of other genetic modifications that are made because the lentivirus needs it to replicate eventually. But we remove the ability of the virus to replicate. So, we're only using the bit of the virus that inserts into the genome and expresses and that's it. So, once you put the virus into the chicken, there's no more virus made. There's not any infectious agents or anything. But that puts the gene into the chicken and that gene is also attached to a promoter which is a bit of DNA that tells the cells to make a protein in a particular place. In this case, it's the promoter that is used for ovalbumin which is the protein that is most abundant in eggs, in egg white. And that then drives the expression of whatever gene that we've put in for expressing another protein.
Kat - And then presumably, when the eggs are laid, you just get the egg white and get the protein out the other end of it.
Lissa - Yes, that's exactly it. we just dilute the egg white down and remove one of the proteins from it which is called ovamucin and that's the protein that creates the kind of jelly-like structure of egg white. So we have to get rid of that so that we can access the rest of it and then we can run it down a standard chromatography column. So this is how all proteins are separated whether for research or for pharmaceuticals. Because the egg only has about 12 proteins in it, it's actually really easy to separate out compared to maybe trying to purify something out of a cell that has hundreds and thousands of proteins.
Kat - How do you know that this works? Are there any drugs that are already made in chicken's eggs and what are the kind of drugs are you working on?
Lissa - So there are actually three drugs on the market that are made from transgenic animals. The very first one was approved in 2009 and that's from the milk of a transgenic goat. There's another a couple of years later which was from the milk of rabbits. I don't know how they milk rabbits so don't ask.
Kat - Carefully. With very small hands!
Lissa - Yes. I just picture there are some very tiny little milkers. And then just in the last year and a half or so, there was another drug that was approved and that is made in transgenic chickens which use pretty much the same methods that we do.
Kat - Given that this seems like an incredible system for making drugs, molecules, that are really active in humans and could be really useful in medicine, is it then feasible? I mean, near where my mom lives, there's a nice free range chicken farm. There are some chickens running around. Presumably, you're going to need more chickens than that.
Lissa - It depends entirely on the drugs you're looking at. So some drugs actually only require a very small dose. And so, you would only maybe need a few hundred chickens and that would do you for your market. There are others where you would probably need farms of hundreds of thousands of chickens. In terms of the feasibility of that and obviously, you have environmental regulations and about having livestock animals, the chickens would have to be indoors. You can't have free range chickens because they might be exposed to outside infections and things eaten by foxes and that sort of thing. You don't want that. But the likelihood of using chickens to replace every single pharmaceutical protein production is very unlikely. It wouldn't be suitable for every single kind. So I think that the thing where you're really going to be targeting these is where you need to make a biologic in very large quantities for a low amount of money but where the dose doesn't need to be that big. So one of the things that we're targeting is actually the animal health market because at the moment, animals are priced out of the biologic's market because it's too expensive to make and people can't afford to pay lots and lots of money for an antibiotic for their dog or treatment for livestock animals. So, these sorts of things where you can't afford to pay a hundred pounds for a dose for each pig you have or each cow you have. But if you can bring that price down by producing it in chickens, then you've suddenly got a big market open to you where you can treat a lot of animals, you can treat companion animals, you can treat livestock without having to overuse antibiotics or without having to just let these animals die because there was no treatment available before.
Kat - The Roslin Institute's Lissa Heron. And if you want to find out more about the legacy of Dolly, take a look at the Roslin Institute's special website - that's
dolly.roslin.ac.uk or you can follow
@Dollyat20 on Twitter.
39:21 - Gene of the Month - Deadpan
Gene of the Month - Deadpan
with Kat Arney
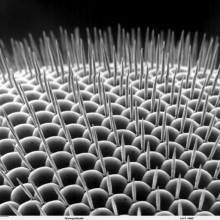
And finally it's time for our Gene of the Month, and this time it's Deadpan. Another of those fruit fly genes, Deadpan was first discovered in 1992 for playing a key role in determining whether a fly will be male or female. The gene encodes a type of molecule known as a transcription factor, which switches genes on, and it's involved in many other roles in the development of an embryonic fly, as well as just its sex. For example, along with other genes called Tramtrack, Phyllopod and Sevenless, Deadpan is involved in building the clusters of light-sensitive cells known as photoreceptors, which make up the repeating units of a fly's compound eye. Although our eyes look very different from a fruit fly's, similar genes are involved in setting up repeating patterns in a human baby's body as it develops in the womb.
- Previous Older drivers drive safely
- Next Moulding the Minds of Tomorrow









Comments
Add a comment