This week's Naked Scientists is not to be sneezed at - we're looking at the science of allergies! We explore what happens to cause your body to overreact to harmless things, and find out how potentially fatal peanut allergy can be cured. Plus, how a dose of parasites could keep allergies at bay, and how special filters can engineer a breath of extremely fresh air!
In this episode

01:40 - Amazing Amazonian geometry
Amazing Amazonian geometry
You may not be familiar with the name Euclid, but you're probably familiar with his ideas. More than two thousand years ago in Ancient Greece, Euclid laid down the foundations of basic geometry, such as the idea that two parallel  lines never cross, and that the angles inside a triangle always add up to a constant number.
lines never cross, and that the angles inside a triangle always add up to a constant number.
Many of us will have learned these basic principles of geometry at school, although some philosophers have suggested that we actually get most of our grasp of geometry from looking at the world around us and moving about in it. For example, figuring out that the shortest way home is in a straight line rather than a curved or wiggly one.
To find out whether this idea is correct, some French psychologists took a field trip to the Amazon, to find out how well the Mundurucu, a tribe of indigenous people who have no formal schooling in maths, grasp the principles of Euclidean geometry.
The researchers developed a series of tasks for adults and children from the tribe, asking them about lines drawn on a flat surface, or on a sphere. For example, they asked whether lines could be drawn between two points, or whether parallel or non-parallel lines would cross. To set the scene, they explained that the points were villages and the lines were paths between the two - a concept very familiar to the Mundurucu, who are experts at navigating around the landscape. They also asked them to estimate the third angle in an incomplete triangle, to see whether the Mundurucu understood that the angles inside a triangle always added up to a constant number.
When completing the tasks, the tribespeople did almost exactly as well as French or American adults and children given the same tasks, who would have had formal education in geometry. This suggests that just figuring out the environment, and learning to get from place to place gives you a pretty good grounding in Euclidean principles, without having to learn about it in the classroom.
But, intriguingly, when the researchers tested very young children - aged 5 or 6 - they found that their grasp of geometry was a bit shakier. They still had some of it right, but hadn't quite figured it out. So overall, it looks like we have an intuitive grasp of the principles of basic geometry, shaped by our learning and interactions with the world around us as we grow up.
This doesn't mean that we should stop learning geometry in the classroom as maths lessons teach you a lot more than the basics. But it does tell us that we develop a lot of our sense of geometry through our experience of the world around us, and that it fits in with Euclid's principles. But what's still not explained is the observation that the Mundurucu, as well as Western people with maths training, can understand concepts that are outside the sphere (pardon the pun) of what they can see or do. So that's something that still needs exploring.

06:59 - Gossip makes faces more memorable
Gossip makes faces more memorable
Gossip you hear about others affects whether you even see  them, a new study has shown.
them, a new study has shown.
According to evolutionary biologists, exchanging juicy tit-bits about others is the human relationship-building equivalent of plucking fleas off each other. It also allows a person to learn the "value" of an individual they have never even met without the potential costs of first hand experience.
But to what extent hearsay influences how the brain regards the subjects of casual water-cooler conversations wasn't known.
Now a US team lead by Northeastern University-based scientist Lisa Barrett and her colleagues has shown that hear bad things about someone you've not even met strongly affects they way your mind sees them.
The researchers asked volunteers to look at images of neutral faces that were paired four times with statements describing either positive - "he helped an old man across the road", neutral - "he closed the curtains" or negative - "he threw a chair across the room" social behaviours.
The participants were then shown the same photographs alongside images of unrelated stimuli, such as a house, in a binocular rivalry task. This is where two images are presented side-by-side, one image in front of one eye, the other image in front of the second eye. The two images then fight for recognition in the brain such that initially just one image is perceived and then, a few seconds later, the other image becomes visually dominant and the first image is suppressed.
When this was happening, the study participants were asked to indicate - by pressing a button, which image they were consciously seeing at any one time. By measuring the relative lengths of the dominance durations, the team were able to determine which visual input the brain was selecting for conscious attention.
The study clearly showed that neutral faces paired previously with negative gossip were consciously viewed for significantly longer than faces paired with either neutral or positive gossip. The researchers ruled out the possibility that their subjects were just learning the negative information better than the positive by also asking them to perform a memory test where they had to categorise the faces according to the statements they had read; this they did without evidence that negative information was being better assimilated.
In other words, say the scientists, hearing that a person lied, stole or cheated makes it significantly more likely that a perceiver will see that structurally neutral but purportedly villainous face because faces previously paired with negative social information are prioritised for consciousness. But why should this be?
"This preferential selection for seeing bad people might protect us from liars and cheats by allowing us to view them for longer and explicitly gather more information about their behaviour," the team point out.

09:38 - Regulatory T cells trigger immunity to transplant rejection
Regulatory T cells trigger immunity to transplant rejection
with Professor Robert Lechler, King's College London
Kat - Also this week, UK scientists have made big step forward in the field of organ transplantation. King's College researcher Robert Lechler and his colleagues have found a way to purify a rare population of immune cells called T-regs, short for regulatory T-cells, which help to switch off immune responses against donor organs that could help to reduce the risk of rejection.
[Robert explained the work to Chris Smith.]
Robert - Organ transplantation, I would say, was one of the major successes of the second half of the last century in the field of medicine because it is lifesaving very often and life transforming almost always. The success rates have improved steadily to the point that now, when you have a kidney or a heart, or a liver, these organs are successfully accepted in around 90% of cases and give a real lift of the quality of life of the patient. So, it's a terrific success story. However, there are three problems. The first is the side effects and complications of the drugs that we have to give to make it work and these are drugs called immunosuppressive drugs that cause blanket depression of the immune system so that the immune system doesn't attack the transplant. But it doesn't only depress the immune response to the transplant. It makes your immune system less competent at protecting you against infections and it increases your risk of cancer. So that's the first problem. The second problem is that transplants tend to fail over time. So the average kidney transplants from a dead donor would normally last around 10 or maybe 12 years and then gradually, they fail, and then the patient - if it's a kidney - goes back onto the kidney machine and waits for another transplant...
 Chris - And is the reason for that failure, Robert, that despite the immunosupression, a gradual and inexorable damage is being unleashed upon the donor tissue by the patient's immune system?
Chris - And is the reason for that failure, Robert, that despite the immunosupression, a gradual and inexorable damage is being unleashed upon the donor tissue by the patient's immune system?
Robert - It's a very good question and the answer is partly yes. Actually, the causes of late transplant failure are quite complicated and involve several different body systems but the immune system is definitely one of the drivers - you're right. Then third limitation is the supply and demand problem that the whole field of transplantation has been a victim of its own success and so we just can't keep up with the numbers of organs that are needed and this is made worse by the organ failure business because of course, kidney patients get back on dialysis and so dialysis programmes are filling up with patients who are waiting for their second or third transplant.
Chris - So what's your solution?
Robert - So we, and many others around the world, have been working on the possibility of making the patient's immune system "selectively blind" - that's one way to put it - to the transplant. The other language used is to make the patients "tolerant" - their immune system - tolerant to the transplant while leaving the immune system intact to protect the patient against infections and cancer. That would solve all three of the problems I described because you wouldn't need long term drugs, number one. Number two, this would probably limit the chronic transplant failure I mentioned, and thirdly, because transplants would last longer, then it would help to address the supply and demand issue.
Chris - And how can you do that?
Robert - There are several approaches that are being explored. The one that we have taken is to exploit a population of white blood cells that we all have in order to protect us from what are called autoimmune diseases when the immune system attacks "self". Many chronic diseases are caused by autoimmune reactions: diabetes, for example; multiple sclerosis; rheumatoid arthritis. These are autoimmune diseases. Most of us don't get those diseases and the reason is because we have this specialised population of white blood cells, they're called regulatory cells. They're rather like policemen that keep the immune system from attacking self. So, the question we posed is, could we take those cells and, if you like, divert their attention to regulate their response against the foreign bits of a transplanted organ.
Chris - These cells are present in the body at very low frequency, so how can you get enough of them and also get just the ones from a mixed population that you need just to protect the target organ and not bring down the immune system comprehensively?
Robert - It's a very good question. So the answer is that the approach we've taken is we've isolated this specialised population of white cells from normal individuals and expanded them in the test tube, and expanded them by stimulating them with foreign antigens - the foreign proteins of a transplanted organ. The ones that respond to the transplant's foreign proteins - those ones selectively grow and then you can make these cells expand to very large numbers in the test tube in order then to infuse them back in adequate numbers in vivo. And because you have only expanded the ones that react to the transplant foreign proteins then they're only going to depress the immune response to the transplant rather than to all the other environmental antigens.
Chris - And when you put them back into the patient, in your case you're using animals as a model obviously; what about the longevity of those cells? Do they last long enough to give us sustained immunosupression selectively against the target organ or are you going to have to keep repeating this process throughout the lifetime of that patient's graft in order to keep their immune system in check?
Robert - The experiments that we've just described were getting close to working in a patient because they were working with human cells and it was a model of human transplant rejection because these were little pieces of human skin that we were protecting with these human cells. So this was the human immune system working in an in vivo context, albeit it was in a mouse. Earlier experiments we've done with mouse cells in a mouse have examined the question that you've just asked and we've looked at that longevity and we can find these cells 80 days after we put them in. So you can find these cells for quite a long time. But, actually, what I would emphasise is that this kind of approach is really designed to tip the balance of the immune system towards tolerance, towards regulation, rather than rejection; and if you can tip that balance and reprogramme the immune system then, actually, it will tend to sustain that tolerant state itself, even if the cells that you initially put in subsequently die.
Kat - And as we'll be hearing later, regulatory T-cells may actually be a key to helping beat allergies too and could also work to help treat autoimmune diseases like rheumatoid arthritis. Let's hope so. That was Kings College London scientist Robert Lechler and he published that work this week in the journal Science Translational Medicine.

16:54 - Sweet solution to water purification
Sweet solution to water purification
Scientists have developed a sugar-fuelled chemical filter to clean up contaminated water.
Provision of clean water is viewed as the leading challenge in the  Twenty First Century, with still over half of the world's population living in unsanitary conditions. The problem is further intensified by the fact that, apart from just sewage which can be filtered out, water sources are also frequently contaminated by persistent organic pollutants such as trichloroethylene and trichlorophenol, which are known to be carcinogenic.
Twenty First Century, with still over half of the world's population living in unsanitary conditions. The problem is further intensified by the fact that, apart from just sewage which can be filtered out, water sources are also frequently contaminated by persistent organic pollutants such as trichloroethylene and trichlorophenol, which are known to be carcinogenic.
Now a team from the University of Kentucky in the US led by Dibakar Bhattacharyya, writing in PNAS, may have the answer in an ingeniuous, low-cost multi-membrane glucose-powered filter that can chemically degrade toxins.
The filter consists of an upper membrane into which is impregnated an enzyme called glucose oxidase. This breaks up glucose molecules to yield hydrogen peroxide, oxygen and gluconic acid. The hydrogen peroxide then passes into a second, lower-layer membrane into which are embedded iron oxide nanoparticles.
These catalyse the decomposition of the peroxide to produce a highly reactive chemical called a hydroxyl radical, which can attack and neutralise toxins present in the water.
As a demonstration of the effectiveness of the technology, the team added a solution of glucose and TCP to the top layer of the membrane, successfully breaking down initially 100% and then about 70% of the TCP passing through.
In a further test on a genuine groundwater sample containing trichloroethylene, over 70% of the chemical pollutant was successfully degraded. With further optimisation, such a system could be used to cheaply detoxify drinking water for the half of the world who currently have no access to safe water supplies.

19:37 - Planet Earth Online - Ash Fall
Planet Earth Online - Ash Fall
with Professor David Pyle, Oxford University
Kat - In April 2010, a previously dormant volcano in Iceland, whose name I shall not try and pronounce, released a massive ash cloud that closed most Europe's air space and disrupted millions of people's travel plans. Planet Earth podcast presenter Sue Nelson was one of those people stranded abroad, so she welcomed the chance to meet Oxford University's Professor David Pyle for whom this cloud had an academic silver lining...
David - I haven't previously worked on Iceland but in this case it was the opportunity of having the ash cloud move from Iceland across the UK and then out across northern Europe, it gave us a once in a lifetime opportunity.
Sue - Let's hope it's once in a lifetime!
David - Once in 50 years maybe - an opportunity to collect fine particles of ash that have travelled between 1000 and 2000 km from the point of emission and before it actually reaches the ground. So we can use our observations to test our understanding of how we think these processes happen.
 Sue - How did you sample the ash then, did you simply come up to rooftops like where we are now and literally wet your finger and put your finger out? Because while I was stuck in Portugal, I was getting texts and emails from people saying 'my car's covered in ash'.
Sue - How did you sample the ash then, did you simply come up to rooftops like where we are now and literally wet your finger and put your finger out? Because while I was stuck in Portugal, I was getting texts and emails from people saying 'my car's covered in ash'.
David - We have a lab full of filters and pumps which we normally take into the field and in this case, the field area was Oxford and the best place to do it was the top of the department of Earth Sciences.
Sue - And you used a sort of larger version of the pump that you've brought up to the roof with us now, which I've got to say is spectacularly unimpressive in that - well, it's a large battery pack about half the size of a bag of sugar, with a couple of big crocodile clips. Otherwise it could be one of those paddles people use to give emergency cardiac arrest treatment. So how does it work?
David - This is an air-sampling pump - I'll just turn it off so you can hear. We use this air-sampling pump to suck air at about 20 litres a minute through a series of filters and it's a way of collecting direct samples from the atmosphere.
Sue - And do you have any of these particles still here in the laboratory?
David - Yes we do.
Sue - Well in that case I think we definitely ought to go and see them...
The lab contains filters, each with evenly spaced dots, showing a range of different size particles collected on the roof. These continue to be part of ongoing studies into the properties of ash particles. But David felt it was easier for me to observe the ash from a slightly more low-tech method of collection.
David - These are actually just two pieces of sellotape which a colleague used to collect the volcanic ash from their car windscreen.
Sue - Is that the large - well compared to what else is on that bit of sellotape - the large dark grain that almost looks like a black sugar or salt grain?
David - No. In fact those large grains will probably be bits of wood or something that's just carried around in the atmosphere and it's kind of the pale brown background material.
Sue - Oh wow! So the stuff that I just thought was general background fluff is actually all the ash.
David - That's right, yes. I don't think we've ever had an opportunity quite like this where we've had observations and samples collected from the volcano itself during the eruption, we've had satellite measurements of how the ash cloud then moves through the atmosphere from the volcano and then thousands of kilometres downwind.
Sue - It's sort of an evolving experiment, isn't it?
David - That's right, yes. So we have a great opportunity to use the measurements in the laboratory to work out whether the ash particles landed as single grains or as clots of grains all caught together.
Sue - Why do you need to know that?
David - It's actually very important both for understanding the hazard to aircraft and also for understanding whether there might be any tiny effect in terms of human health. Very fine particles, between 2.5 and 5 microns or so, are actually small enough to be inhaled into the lungs. If those very fine particles have actually clumped together in the ash cloud, that clump of particles will behave as if it were a larger particle and it will then land on the ground after 1000km rather than after 5000km. And once it's landed on the ground there's a chance that the fine particles will then separate and you'll have a higher than expected concentration of very fine particles at ground level. And this is one of the things we want to investigate.
Kat - That was Professor David Pyle from the University of Oxford talking to Sue Nelson about the ongoing investigation of ash particles collected from the troublesome Icelandic volcano eruption last year.

24:46 - Curing Peanut Allergies
Curing Peanut Allergies
with Dr Pamela Ewan, Addenbrookes Hospital
Chris - We're talking allergy this week and food allergies, it turns out, are relatively common. Figures we've seen from the US suggested up to 8% of young children and perhaps 3 1/2 % of adults are affected by them. In many cases, it's a bit more than a nuisance but that's about all, but for some people it can actually be a fatal problem. Pamela Ewan is with us from Addenbrookes Hospital where she's trying to develop a way to help people who have peanut allergies. Hello, Pam. Thanks for coming on the program.
Pam - Hello.
Chris - First of all, for people who just have an allergy, what actually is allergy? What's going on chemically in their bodies?
 Pam - Well in people with allergy, the problem is they've made an unwanted immune response so they make allergic antibody in which under normal circumstances, at least in our civilised environment, westernised environment, we don't need. So we first of all make this harmful antibody or unwanted antibody, and when you're then exposed to the protein to which this antibody is directed against, you get a reaction causing cells in the body to fire off, releasing a whole lot of chemicals which produce the symptoms.
Pam - Well in people with allergy, the problem is they've made an unwanted immune response so they make allergic antibody in which under normal circumstances, at least in our civilised environment, westernised environment, we don't need. So we first of all make this harmful antibody or unwanted antibody, and when you're then exposed to the protein to which this antibody is directed against, you get a reaction causing cells in the body to fire off, releasing a whole lot of chemicals which produce the symptoms.
Chris - What are the antibodies that do that and what are the chemicals that then unleash the unpleasant symptoms that we all associate with, having an allergic reaction?
Pam - Well, there's a whole range that can cause this. From things we breath in like pollens, or cat or dog allergens, dusts; to foods, to drugs, almost anything that is a protein can do this.
Chris - And what's it binding onto? You said antibodies. What sort of antibodies and where are they?
Pam - These antibodies, these allergic antibodies are called IgE and they're fixed onto cells in the body called mast cells which are really surrounding every place in the body where you meet the outside world. So it's the eye, the lining of the nose, the lining of the airways into the lung, the lining of the gut, and so on, but also in the skin. So, they're a sort of defence.
Chris - And when these IgE antibodies see the thing that they're reacting to, the thing you're allergic to, what do they then do?
Pam - They link up and cause activation pathways in the cells, allowing chemicals, particularly histamine, which are stored in these cells in little granules to be released and this whole thing can happen really quickly. So say, we were talking about cat allergy and you have cat IgE antibody within 30 seconds to a minute of inhaling the cat allergen, getting it up your nose, getting it in your eye. It binds with this antibody, fires off the cell and these mediators are released.
Chris - Now under normal circumstances they're there to protect us, presumably, these cells and they wouldn't normally react to the things that people are reacting to when they have an allergy. They would be reacting to bad things to warn the body there is a bad thing coming and so, those mechanisms will be good under certain circumstances but they just go into overdrive in people with allergy.
Pam - In allergy, these antibodies are directed against common environmental allergens which you should normally tolerate, so that's the primary problem.
Chris - So why do people make them?
Pam - Well, we think it's because the immune system becomes reprogrammed probably because you're not using this part of the immune system, because it's mainly important to parasitic infections. So preventing you getting infections with various parasites, worms, and so on. If you don't use it for that, it seems in allergy, you switch and use this pathway against allergens or proteins that should be normally tolerated.
Chris - So why is it then that -I have a little bit of hayfever, I will get itchy eyes and a runny nose, but I certainly wouldn't get anaphylaxis so I won't have to be resuscitated; but somebody who has, say a peanut allergy, I had somebody who lived in our house once and we had to be very careful with where she stored her food and where we kept our food because just a trace of peanut was enough to provoke this enormous and dramatic reaction in her that could be fatal.
Pam - Well it depends on where the allergen, the thing you're allergic to is getting to. So with pollen, with hayfever, you're breathing it in. It's in the air, so a little bit of it gets up your nose, gets in your eyes, and there, it meets the allergic antibody and fires off the reaction. Most of it is probably filtered out in your nose, so very little gets into your lung. Within a few people, it could cause asthma if it has got down there. Peanut or foods get absorbed into the circulation quite quickly. So although you eat them, they rapidly get absorbed from your mouth and so, quite quickly, they're all over the body and that's why you get these bad reactions.
Chris - Do we know whether they really are becoming more common? It seems that everyone you meet these days, either knows someone or themselves have some kind of dramatic allergy like this. Is it just that awareness has gone up or are they much more common?
Pam - No. There's a really well documented increase. There's a massive increase in the last 30 to 40 years and even bigger increases in certain allergies in the last 10 to 15, but there are quite good studies in similar populations comparing incidents of disease 30 or 40 years back and more recently, and there's a substantial rise. So most of it is real. There will be a bit of better recognition. There will be a bit of people thinking they're allergic when they're not, but there is a very big increase. So now, potentially about 1 in 3 of our population in the UK have an allergy.
Chris - Gosh! That's very high. Do you have any feeling for why that might be happening?
Pam - Well, this is complex but put simply, it's thought to be due to modern westernised lifestyle. So it's factors in our lifestyle, infection, or lack of infection may be an important component. There are probably lots of other things that we still haven't dissected out but it could be a whole variety of things. We have very different diet. We have different exposure to chemicals. There could be lots of reasons.
Chris - I did read there was an association between being exposed to big doses of antibiotics under a certain threshold age and this may have an impact on the kind of microorganisms that flourish in the gut, and they in turn educate the immune system and this may distort the ability of the immune system to tell friend from foe for a while, and therefore encourage allergies to establish.
Pam - It could be that. A lot of these theories focus on lack of infection or antibiotics or other things in early childhood. What is also interesting though is that we're seeing much older people who've been fine all their lives, at 16, 17-years-old becoming allergic. So you can't blame that on early programming.
Chris - And what are you doing to try and help the people who you've been dealing with, with these quite profound peanut allergies?
Pam - Well perhaps first of all, to say peanut allergy is a very severe allergy or potentially very severe. So of the food allergies, it's the one that is most likely to cause either fatal or near fatal reaction, so it's a big problem. So it's a frightening diagnosis to have and it's also quite hard to avoid peanuts even if you're intending to. They're hidden in things and so, it's quite a difficult disease to manage. What we've done is we've tried to see if we could desensitise children with peanut allergy. In other words, switch off the allergy. Really, a cure we're aiming at.
What we've done is we've taken children with proven peanut allergy. We test them at the beginning to establish exactly how much of the peanut is needed before they kick in with an allergic reaction. We then give them peanut by mouth. We use peanut flour. So that's obtained by crushing and defatting peanuts. So we give them peanut flour hidden in some other food, starting with really tiny doses, something like a 300th of a peanut, so way below of what we know is their threshold for reaction. And then we very slowly step up, increasing the doses. The way we do this is we have them up to the hospital once a fortnight, we give them a dose, they go home and take the same dose every day for 4th night. They come back, we step up a bit, two more weeks on the same dose, and so it goes on until we get up to 800 milligrams which is equivalent to about 5 whole peanuts. So by the end of this updosing regime, they're eating and tolerating 5 peanuts. Then they go on having 5 peanuts a day for ages and then we do another challenge test where we give them 12 peanuts and we do that at about 6 weeks after they've been on the maintenance dose. And then 30 weeks out, we try a really huge challenge where we give them 32 peanuts.
Chris - And just very briefly to finish us off Pam, not literally obviously, can you tell us, why is it then that they can have a whiff of peanut and it can be fatal or near fatal for them, but after this kind of therapy that you give to them, they are able to tolerate it? What is changing?
Pam - Well we're looking at that as we go along and what we know so far is that their allergic antibody, this IgE to peanut has gone down. It hasn't gone away but it's gone down quite a bit and we know from other forms of desensitisation say, for pollen, the same thing happens and we're also looking at other immunological mechanisms including these T-regulatory cells you were hearing about earlier in the program to see if we can show that the immune system is being reprogrammed from an immune response which is pro-allergy into one that is anti-allergy.
Chris - Terrific! Well it's fantastic work. Thank you very much for coming in to the show. That's Pam Ewan. She is at Addenbrookes Hospital where she's doing that work.

34:35 - Parasites and Allergies
Parasites and Allergies
with Professor Rick Maizels, Edinburgh University
Rates of allergic conditions have gone up in recent years yet were virtually unheard of before the 19th century. This has led some people to suggest what's known as the "hygiene hypothesis" - that leading an overly hygienic life, as we do nowadays, may increase the tendency for the immune system to react to things that it would normally ignore. To tell us more about the hygiene hypothesis, from Edinburgh University Professor Rick Maizels...
Rick - Well it's essentially saying that the immune system that we have now evolved in the presence of many infectious organisms over eons of time and is best adapted to operate and protect us in the presence of various parasites and other infections. And as I may mention in a moment, some of these infectious organisms are a little bit immunosuppressive, dampen the immune system for their own protection. In the absence of those parasites and those microorganisms, the immune system now overshoots. So you have instances perhaps - and this is the hypothesis - we have instances where the immune system is overeactive and unnecessarily targets innocuous environmental antigens, otherwise known as allergens as we've just been hearing from Pam.
Kat - So basically, having worms meant that your immune system had something to do? It was focusing on the worms and not on having an allergy.
Rick - That's one interpretation, but the other interpretation is that the parasites are doing something actively to dampen an allergic reaction.
Kat - So what do you think they're doing?
Rick - What we wanted to do is to see whether there was a causal relationship. Was it the presence of the parasites that actually protected, actively protected, against allergy? We showed that in the laboratory in mice, and then going further, we are able to show that our new friends, these T-regs, these regulatory T-cells, which Robert Lechler called the policeman of the immune system, they were preventing allergy in mice so that parasites were able to expand the body's own mechanism that protects us from allergy.
Kat - So the immune system is using these cells to let the parasites get away with it and it's occupying them enough so that they're not amounting allergic reactions to things.
Rick - It's a question of half full or half empty. It's either the immune system is choosing to do this because it protects the body from allergy or it's the parasite manipulating this human immune system in its own interest, but at the same time, actually having a beneficial effect.
Kat - But is it the case that it's just parasites that do this or other dirty things in our dirty world that might be doing this to us?
Rick - I think it's much broader and I think what we've found is a point of principle and as Pam was saying how the rapid rise in allergies really in the last few decades, and of course, western populations reduced parasite loads many years before that. So, I think what we'll find is that in the environment and in the sort of global spectrum of different infectious organisms, there are some particular species which actually have a beneficial effect, and are not necessarily dirty. I mean, some of them may well be natural commensal microorganisms which expanded or decreased because of our diet and that's also been mentioned. I think we have to take a global view of all these different influences.
Kat - Because obviously, you don't want to infect someone with worms, just to make they're hayfever better. How do you think you can take some of the discoveries you've made forward to make maybe viable preventatives or treatments for people with allergies?
Rick - Well what we're aiming to do is to reproduce the effect of a parasite infection without having to have a live parasite within you. And we've been able to do this firstly by collecting these regulatory T-cells and show that these will protect mice from allergy. Now, we are isolating active substances from the parasite that themselves expand these regulatory T-cells in the lab, with the objective then of being able to replace live infection with an active principle from the parasite itself...

40:37 - Naked Engineering - Filtering our Air Supply
Naked Engineering - Filtering our Air Supply
with Chloe Agg, WPS-CEL
Meera - This week, Dave and I are exploring the process of air filtration. Dave, what in the air would we want to filter out?
Dave - Well it depends what you want to do with the air. If you want to just make it more breathable, you might want to filter out the big particles, which will go into your lungs, or possibly get some of the pollen out there which you might be allergic to. But if you want to make a computer chip, you're going to want to get virtually everything out down to the tiny, tiny particles, micron size sort of things you get made in a diesel engine.
Meera - Another industry where this is important is the pharmaceutical industry. To find out more about air filtration here, we've come along to the process engineering company, WSP CEL in Coventry to meet Chloe Agg, the Building Services Engineer here. Now Chloe, how is a system set up in a pharmaceutical factory? What does an air handling unit look like?
Chloe - An air handling unit is a big gray box. Usually, they're about the same size as a static caravan. The purpose of this is to pull the air in from the outside, clean it up, make sure it's the right temperature, the right humidity and pump it all in to the pharmaceutical factory.
Meera - And as this air is getting drawn in, what kind of particles are you wanting to remove?
Chloe - First of all, we need to make sure that no birds can get inside the air handling unit, so we have a bird mesh for that. Then slightly smaller objects, we need to make sure that there are no flies or other insects that can get in, so we have an insect mesh. And then the next stage is a panel filter. We have one right here. It's made of cotton fibres and wire mesh and it prevents any large particles from getting into the AHU - the air handling unit.
Meera - So it's a square-shaped panel with cotton fibre material going through, but it's pleated in a vertical way, so it's pleated going all the way up through the filter.
Chloe - That's right. The filter is zigzagged along to make sure there's extra 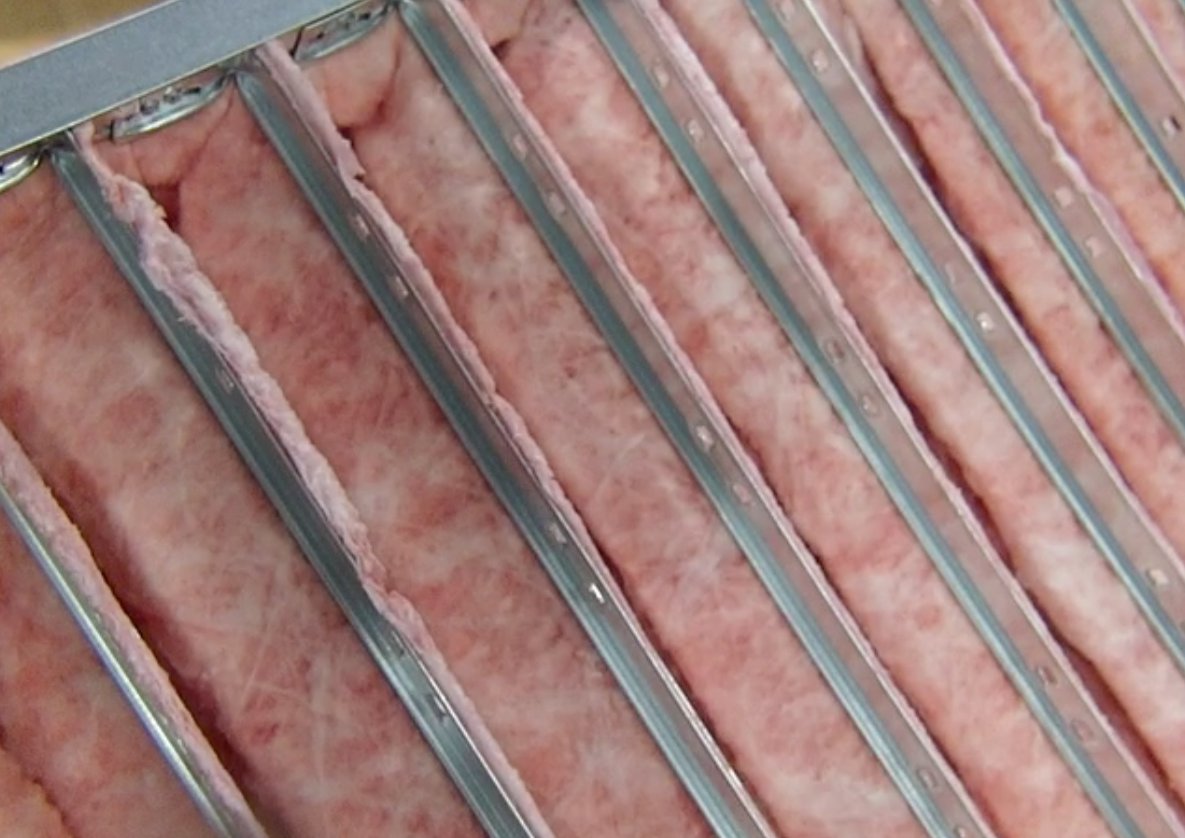 surface area for all the air to pass through nice and slowly.
surface area for all the air to pass through nice and slowly.
Dave - Because if the air is rushing through, you're likely to force more larger particles through than if it's just moving gently, when it's likely to get jammed in the filter.
Chloe - If the air is moving more slowly through it, there's more opportunity for the particles to get trapped, and it also means that it takes less energy to pull the air through.
Meera - So at this stage, you really removed birds, insects, and large particles of things like dust as well, but you still have very small unwanted particles that you want to remove. What kind of smaller particles do you want to remove and just how small are these?
Chloe - The particles could be anything down to the size of about 0.1 micron, they can be microbes and bacteria, and all sorts of harmful things you wouldn't want in a pharmaceutical environment.
Dave - So that's a particle which is about a 500th of a human hair across. Can you still filter them by essentially a sieve process like the other filters?
Chloe - If we try to filter out those particles using the sieve process, we'd have to have such a densely matted filter that it would block almost instantly and will take loads of energy to pass the air through.
Meera - So how are these particles stopped and what kind of filter is used?
Chloe - We use a High Efficiency Particulate Air filter or a HEPA filter. Those filters are quite different to the panel filters and are usually made from glass fibre. We use glass fibres rather than cotton fibres because they're smaller and you can get a higher density of them so that the small holes between them are smaller than they are on the cotton filter. The filters are made so they've got lots and lots of surface area. They might be a bag or they might be, again, zigzags like the panel filter.
Meera - But if you're not then just sieving out these particles, how are you getting rid of things like microbes and bacteria?
Chloe - The particles are captured in one of three different ways. It might be through impaction, interception or diffusion. The larger particles tend to be captured by impaction. That means that they collide with a fibre, even though a hole next to the fibre might have been larger than the particle itself. Interception means that their particle passes near to a fibre and is attracted to it, and gets stuck. And diffusion happens only with the very, very small particles, and it works kind of like brownian motion. The small particles don't move in a straight line through the filter. They move around in a random motion and because this means they take longer to pass through the filter, it gives them more opportunities to get stuck to the fibres in other ways.
Dave - So all three of these processes are basically based on a particle moving through the filter and being attracted to a fibre, and actually just sticking to it.
Meera - What about the structure of these HEPA filters? So we've established that they can be made of glass fibres in order to capture particles, but there are also different types. So we've got two filters here in front of us and one is very - it's got these pleats going backwards, kind of away from us, but putting my hand just inside, the material is extremely soft. It feels just a bit like the lining is just cotton wool or something. That's the kind of texture it has.
Chloe - That filter is a fabric filter. So it's still made of glass fibres, but it's like the loft insulation that you get at home, nice and soft, and it gives lots of different places for their particles to get stuck to.
 Meera - Next to it, is a very rigid structure. The first filter had over 10 pleats. This one's got about 4 or 5 now and it's a lot more rigid. What's the material here?
Meera - Next to it, is a very rigid structure. The first filter had over 10 pleats. This one's got about 4 or 5 now and it's a lot more rigid. What's the material here?
Chloe - This is a paper version of the glass fibre and although it looks like there are only four pleats, actually, each of those pleats has got several hundred pleats within it.
Dave - So you get a larger surface area into the same space which means you can push the air through more slowly, thus saving energy.
Chloe - That's right and also with the rigid filter because it doesn't move in the air, it doesn't take any energy out of the air.
Meera - How long do these filters really last? They must get blocked up at some point. What happens when they do get blocked up and how do you know when they are?
Chloe - We make sure we monitor the pressure at either side of the filter and that tells us as the filters are slowly getting blocked up because the pressure drop across it will be larger. Depending on what air you're filtering, that could be anything from 3 months to a year. When you do need to change it though, it might be full of quite dangerous pharmaceutical ingredients, so you usually have to incinerate them.
Meera - How efficient are they at removing the unwanted particles?
Chloe - The filters we've got in front of us would remove 99.995% of all small particles.
Meera - That is a very high degree of accuracy, so what would the future challenges or aims even be to make this even better as filters?
Chloe - To reduce the amount of energy that they use. At the moment, the air handling units that these filters are in use about 15 kilowatts for the fan. That's just to pull the air through the air handling unit and into the pharmaceutical factory. But they could also be potentially using around 200 kilowatts of cooling to make the air cold enough to pull the moisture out to do de-humidification. And after that, you need to heat the air up to make sure that all the occupants of the rooms are nice and warm and comfortable. So you could be using another 80 or 90 kilowatts just for that. So in total, you're looking at around 300 kilowatts for one air handling unit.
Dave - So that's several family cars running flat out continuously 365 days a year.
Chloe - We take into account energy efficiency a lot in our designs now. The real challenge is to be able to design a pharmaceutical factory where there's a nice, safe, clean environment for manufacturing, but one that isn't using the same energy as several family cars continuously.
Chris - Chloe Agg who is the Process Engineer at WPS CEL showing Meera and Dave How to remove even the smallest contaminants from our air supply.
Why isn't there a vaccine for hayfever?
Rick - Vaccines boost and stimulate the immune system and the problem with hayfever is an over reactive, unnecessarily reactive immune system. So really, we need an anti-vaccine. I guess because it's easier to start an immune response than stop one, we're likely able to have a single shot, but that's as Pam was telling you, maybe a more softly-softly approach could work.
Chris - Pam, anything to add to that?
Pam - Well, there is a special desensitising vaccine that you can use for pollen allergy which works quite well, so that's not a normal sort of vaccine as Rick was saying which would stimulate the immune system, but there is an allergy vaccine which can work.
Chris - Is that sort of using the same principle as your gently-gently, softly-softly approach to peanut stimulation?
Pam - It's different. No, it's doing it by injection, so it's giving an injection into the skin. So, that systemic sort of stimulation to the body, but otherwise, similar principle, yes.
Will my cat allergy get worse with time?
Pam - No, I don't think that would make it worse. So it would be fine to carry on with antihistamines, but cat allergy can get worse if you constantly expose yourself to cat, providing your allergy is on the severe side. So, it can get worse and worse, so it's best to minimise exposure. But the opposite of that is that people with very mild cat allergy can actually be okay, providing they have constant but low exposure to their own cat.
How do we treat cat allergies?
Pam - Well, you can be de-sensitised to cats, but it doesn't work very well. We do sometimes see this for vets or people where it's very important to absolutely get it under control, but the standard treatment which is the first line and usually works very well is a nasal spray, eye drops, and non-sedative antihistamine. So there's a very good treatment that will work.
Why didn't humans evolve through allergies?
Rick - Well, we evolved to tune our immune system in the presence of different infectious organisms and in a way, allergies have resulted because we're no longer in the environment in which we evolved. So I suppose, because allergies are so recent and human population is no longer being selected by natural selection, I don't think we are going to evolve through allergies.
Do children typically grow out of food allergies?
Pam - Well that depends on the food allergy. So if you had egg or milk allergy as a young child, there's a very good chance of growing out, but if you had a peanut allergy, only a tiny minority of the very mild ones might grow out. So it's very dependent on which food we're talking about.
Chris - Do you know why?
Pam - We don't know for sure why this is, but we've done some research on egg allergy, looking at those who resolve and those who persist, and we can see changes in the immune system. The development of these T regulatory cells and various chemicals they produce occurs in the children who grow out of egg allergy. So it may be that it's somehow easier with certain foods, like egg and milk, to develop the right sort of immunity to grow out. And perhaps that's due to small amounts of these things being in foods.
How do you know if you have an allergy?
Pam - You should go and see a doctor first, but you would go by the symptoms. The symptoms would tell you what disease, and then that disease may or may not be allergic. In order to work out that you've got to look at circumstances of exposure, when the allergy comes on. It's obviously easy if it's something like a cat, you go near it and you get symptoms. It's not so easy if it's something like house dust mite, which you're exposed to most of the time. But by teasing out the circumstances, you can have a good idea, and then that can be backed up by allergy tests, which can show you've got this allergic antibody to whichever substance you're looking at.
Kat - And what would be the typical symptoms of allergies? Presumably it's different for a food allergy compared to a cat allergy?
Pam - Exactly. Allergy in the nose, eyes or lungs, so rhinitis and asthma, you would get sneezing, itchy eyes, blocked nose, runny nose and asthma. With a food allergy, you might get an acute reaction with rash and swelling, through to something much more severe. Or, chronically, you could get eczema due to food.
What can mums do to reduce the chances of their children having allergies?
Pam - That's difficult to answer. I don't know if he's asking about breast feeding, but breast feeding is thought to protect against allergy. We don't know when the right time to wean is, and there's a lot of research going on at the moment to look and see whether early introduction of food might actually be better, and reduce the incidence of food allergy rather than late weaning.
Does local honey alleviate hayfever?
Pam - I don't think so. Quite a lot of people say this, but there's no scientific evidence, as far as I know, showing why. People think they're eating pollen, and that might help, but the amounts of pollen will be pretty low.

Does being allergy-prone have a genetic factor?
Pamela Ewan, from Addenbrooke's Hospital Cambridge, and Rick Maizels from the University of Glasgow, answered this question...
Rick - Some of those genes were probably preserved in the human population because they protected people from infections such as these helminth parasites. So the other side of the coin is that the same reactions that now give us allergies are protective against some parasites.
Chris - Pam, anything to add to that?
Pam - That's a good answer. There does seem to be some genetic basis, but it's quite loose. We know if one parent has allergy, the child is more likely to, and if both parents have allergy, the child is even more likely to. But it's quite hard to pin it down to a specific gene. There are certain genetic associations, but it's quite loose.
Should peanut allergy sufferers avoid all nuts?
Pam - The answer to that is a bit complex, but peanut allergy and tree nut allergy, in other words the non-legume nuts, occur commonly in the same people, but you can have them separately. If we get a child with one nut allergy, we will say "avoid all nuts" because we know they're likely to go on to develop other nut allergies.
55:58 - How much petrol should I put in my car?
How much petrol should I put in my car?
We put this to James Painter, from Bloodhound SSC... James - Hello, I'm James Painter. I'm one of the engineering leads on the Bloodhound land speed record project. We're at the moment designing and developing a vehicle to set a new land speed record and we're targeting 1,000 miles an hour.
Well that's an interesting question. I mean really, once you're carrying around more fuel than you actually need to get from A to B or to your next petrol station, you're carrying around more fuel, essentially, than you need. So, I suppose essentially non optimum, but certainly, it does depend on how far you want to go, how quickly you want to get there and how much you enjoy sweating when the low fuel light comes on.
Certainly in terms of vehicles and automotive manufacturers are a lot of family size fuel tanks tend to 40 to 60 litres and really, that's driven by giving vehicles a reasonable range. And also, in terms of the packaging space that the manufacturer has got to play with in terms of getting the fuel tank located. So when you are carrying around this additional fuel, certainly starting and stopping, accelerating and breaking that fuel is a bit more of a penalty within town driving, rather than when you're on the way to way and you're actually doing at a constant speed on the motor way.
Diana - So it's best to only fill up what you need but this could lead to hundreds of visits to the petrol station which might be out of the way and therefore add extra mileage.










Comments
Add a comment