How to Keep your Heart Healthy
This programme comes to you from the British Cardiovascular Society Conference in Manchester, where leaders in the field have been presenting their latest research on preventing heart disease: one of the leading causes of death. We explore the radioactive toothpaste that can help you predict heart attacks, listen in to a genuine heart transplant and ask whether running really keeps your heart healthy.
In this episode

00:52 - Why fund heart research?
Why fund heart research?
with Professor Peter Weissberg, BHF
Cardiovascular disease (disease affecting the heart and blood vessels) is the  single biggest killer in the Western World. There is an annual British Cardiovascular society conference, where leading researchers from across the world meet to discuss how to predict and prevent heart disease. The conference is supported by the British Heart Foundation, which spends 100 million pounds on heart research every year. Professor Peter Weissberg is the charity's Medical director...
single biggest killer in the Western World. There is an annual British Cardiovascular society conference, where leading researchers from across the world meet to discuss how to predict and prevent heart disease. The conference is supported by the British Heart Foundation, which spends 100 million pounds on heart research every year. Professor Peter Weissberg is the charity's Medical director...
Peter - We've done extraordinary well as a community for heart disease over the last 50 years. The British Heart Foundation's been around for just over 50 years and in that time there's been a phenomenal drop in mortality from coronary disease in particular, so there's a huge success story there. But the problem is is that we're left with a community that's ageing, with a lot of chronic disability, a lot of heart failure, patients surviving heart attacks who would have died from them previously but now survive with damaged hearts, so we have a lot of problems that are accumulating in the elderly population that we've still got to deal with.
Chris - And what is B.H.F. doing about that?
Peter - So our priorities now are to try to improve prevention, diagnosis, and treatment of heart disease, particularly at a fundamental level. So most of our research money goes on basic scientific research to understand mechanisms, particularly at the moment, the mechanisms by which we might be able to regenerate the myocardium so that we can repair damaged hearts. If that were to occur then, of course, we could reverse the damage done by heart attacks and prevent the epidemic from heart failure which is accruing at the moment. If we can understand the fundamental biology of atherosclerosis properly then we can prevent and treat it better and, likewise, if we understand the molecular mechanisms of things like arrhythmia and congenital heart disease there's a chance of putting those right. So we're very much focussed on investment in the scientific basis of cardiovascular disease as a mechanisms for finding ways of treating it.
02:56 - Cardiology 101
Cardiology 101
with Dr Niall Campbell, Wythenshawe Hospital
Your heart pumps around 6,000 litres of blood around your body every day. But just how does it achieve this incredible feat? Cardiologist Dr Niall Campbell gave Chris Smith and introduction into the body's central organ...
how does it achieve this incredible feat? Cardiologist Dr Niall Campbell gave Chris Smith and introduction into the body's central organ...
Niall - My name is Dr Niall Campbell. I'm a consultant cardiologist, which is a heart specialist and I work at Wythenshawe Hospital, which is a large hospital in South Manchester.
The heart sits slightly to the left of the middle of our chest and it's a pump for moving blood around the body. The reason why we need to move blood around the body is to supply oxygen, sugars, and nutrients to the rest of the organs in the body.
Chris - How does this pump work - what's inside the heart that enables it to do that?
Niall - The pump has got four chambers and the heart is made up of a muscle. The two chambers at the top of the heart are called the atria, the two chambers at the bottom of the heart are called the ventricle. And there are four valves inside the heart which enable blood to flow into the heart and be pumped out of the heart in the correct direction so that blood can go from the left side of the heart to the rest of the body from the right side of the heart to the lungs where the blood can be oxygenated.
Chris - Why do you need to two halves to your heart, a right side and a left side like that?
Niall - So, blood flows to the right side of the heart from the rest of the body and that blood has low levels of oxygen. That is then pumped to the lungs where the lungs supply the blood with oxygen. Blood then flows to the left side of the heart and then that blood, which contains oxygen is then pumped back to the rest of the body, completing the circuit.
Chris - So when I put my fingers on my wrist and I feel my pulse, what does that correspond to and what is the heart doing to produce that pulse?
Niall - So, what you are feeling in your pulse is the blood flowing through your arteries and that is blood which is coming from your heart to your hand. That heart rate is controlled from the top right hand chamber of the heart from an area of the cells called the sinoatrial node, and that is almost like a beacon, or lighthouse which sends our repeated electrical signals. Those electrical signals are then transmitted from the top right chamber of the heart in a coordinated electrical system of motorways down to the bottom chambers of the heart to ensure that all the chambers of the heart pump in a coordinated fashion.
Chris - And when a cardiologist like you does an ECG you are recording that electrical activity and that tells you how the heart's performing?
Niall - That's correct. We are able to look at the ECG and we are able to work out exactly what is happening electrically in each chamber of the heart at any one time, and that enables us to make diagnoses about normal heart function but also enables us to give us an idea of what happens electrically when the heart starts to have problems.

05:51 - How does an ECG work?
How does an ECG work?
with Dr James Rudd, Addenbrooke's Hospital
ECG stands for "electrocardiogram" and this is the heart trace corresponding to the electrical signals produced by the heart as it beats. To find out what it's like to undergo the procedure, Chris Smith turned himself into a medical guinea pig and went along to Addenbrooke's Hospital in Cambridge...
the electrical signals produced by the heart as it beats. To find out what it's like to undergo the procedure, Chris Smith turned himself into a medical guinea pig and went along to Addenbrooke's Hospital in Cambridge...
James - I'm James Rudd. I'm a consultant cardiologist at Addenbrooke's Hospital in Cambridge, and we are in the ECG recording department and we are going to record your ECG today. So, if you'd like to follow me, we will head through into the examination room...
This is Laura. She is a cardiac physiologist and she's going to be recording the ECG today for you.
Chris - Hi Laura.
Laura - Hi Chris.
Chris - So what do you want me to do?
Laura - What I need you to do is remove the clothes from your top half so I can get to your bare chest...
Chris - Ok, I'm down to my bare chest...
Laura - Ok. So if could lie down so that your heads on the pillow and just make yourself nice and comfortable.
Chris - I don't normally get to lie down at work in the hospital.
Laura - Are you comfortable now?
Chris - I'm very comfortable.
Laura - So, I just need to shave your chest so that I can pop the stickers on.
Chris - When you say stickers?
Laura - The electrodes for the ECG.
Chris - Right, OK. I didn't realise that I was going to get a shave when I came to work.
Laura - Yep. That's a hairy chest there. So are you ready for this one?
Chris - I think so...
Laura - Just on the other side... There we go.
Chris - So you've just taken a little bit right in the middle, basically between the beast, isn't it?
Laura - Yes, just either side of your sternum there. Are you allergic to alcohol wipes or disinfectants?
Chris - I'm not allergic to alcohol - I know that for a fact. Alcohol wipes - no fine.
Laura - No bar here, unfortunately. I'm just going to wipe the areas where I'm going to put the electrodes, just to make sure there's a good contact with your skin, so it might feel a bit cold now. OK?
Chris - You're also cleaning up my ankles?
Laura - Yes, so stickers go on your arms and legs as well as on your chest. Right, so lot's of stickers now...
Chris - They look like they've got a sort of jelly on the back - the sticky with the jelly?
Laura - Yes. There is a gel and that makes a contact with your skin to pick up the electrical activity.
Chris - So, there's one gone on my left arm at the top on my shoulder, one gone on the right side of my chest. That's two on the chest. Is there a particular place you put them?
Laura - Yes. Each sticker has a specific position so that each ECG we do is exactly the same for every person. So I'm just going to get all the wires now and I'm going to place these on all of the stickers.
Chris - They've got almost like little crocodile clips like you'd connect up to battery or something on the end of the wires. They're going on these tabs?
Laura - They clip onto the stickers. They just stick onto the electrodes. OK?
Beep, Beep...
Chris - OK. So now I have wires everywhere?
Laura - Yes, ten wires. So now I need you to lie back into the bed and just relax as much as you can so that it makes a nice, clear recording...
Beep, Beep, Beep...
Laura - And that's your ECG done.
Chris - Right, now it comes to the verdict! I'm going to talk to the cardiologist and find out what is shows...
James - So we've got your ECG in front of us now Chris, and what we can see is a piece of graph paper with some black lines on. In essence, we've got a plot of voltage against time. So this is a snapshot of your heartbeat over about five seconds and, as you may be aware, the heart is a large muscle, it's about the size of your fist. And within the heart are specialist cells which are called pacemaker cells and these cells generate very small voltages which we can pick up on the surface of the skin using the ECG test.
Chris - OK. Can you then take me through James, how what we're seeing on this piece of paper relates to what my heart is doing.
James - So, the very first part of the trace here. I'm just pointing to what looks like a humpedback bridge. This is called a P wave and this actually happens when the atria at the top of the heart are full of blood and begin to pump the blood into the ventricles, and the atria are the holding chambers, if you like, at the top of the heart and they receive blood from the rest of the body and also from the lungs.
The next thing we see is a very sharp up and then down stroke and this is when the main pumping chambers of the heart, the ventricles, start to contract. They expel the blood around the body and they also push blood to the lungs as well.
Finally, we have another humpback bridge. This is called the T wave of the ECG and this is when the electrical activity of the heart is resetting itself back to normal, and the ventricles and atria are relaxed and getting themselves ready for the next heartbeat.
Chris - How could a cardiologist like you then take that trace and see when a person has a problem?
James - So there are several elements we can look at. We can look at the heart rate, we can look at whether the heartbeats are happening regularly or irregularly, and we can also actually look at the waves themselves. Sometimes they have unusual shapes, which we recognise as being a signal of an abnormality in the heart.
Chris - If I had heart disease. Say a third up coronary artery - not enough blood is getting to my heart. Would you be able to tell that from an ECG?
James - In most cases we can, yes, and it's always the first test that we do. As soon as you come into hospital, we would do an ECG, particularly if you had symptoms of a heart problems like chest pain or palpitations. An ECG is a really quick, inexpensive tool for giving us a clue as to exactly what's going on with the heart.

11:50 - The birth of a heart
The birth of a heart
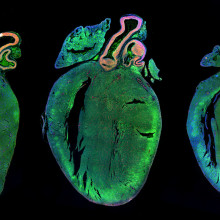
with Professor Alice Roberts, University of Birmingham & Emily Noel, University of Sheffield
One method being used by scientists to investigate the heart, and heart problems, is by looking at how they form in the first place. This is its embryological development.  Birmingham University's Alice Roberts is a clinical anatomist and she's just written a book on the subject...
Birmingham University's Alice Roberts is a clinical anatomist and she's just written a book on the subject...
Alice - Embryology is largely just how a single cell, a single fertilised egg develops into a baby. So you look at how cells proliferate. And there's this wonderful process of origami where new tissues form and they fold in on themselves and some of it's quite destructive as well, so you get cell death occurring to separate the fingers for example. Or particularly relevant to the cardiovascular system where you get rods of tissue forming and cell death in the middle producing little tubes which will later be blood vessel.
So when you look at the development of the heart embryologically, you see that it basically forms as a contractile vessel and then it loops around and it has to undergo this process of septation. So you get, essentially, little partitions appearing in the heart, which set it up so that at the moment of birth, it can suddenly go from supporting a single circulation to supporting a double circulation which you need if you're an air breathing animal, which you suddenly become when you're born. Up until that point you haven't been using your lungs to breathe air and instead you've been getting your oxygen from the placenta which enters the heart in a completely different way.
So embryology helps us understand the function of the heart during the antenatal period, so in that nine months when you're in your mother's womb. But also, actually, it has real relevance for understanding congenital heart defects as well. Because a lot of the problems that we see in babies hearts are because of something going slightly wrong with what is actually a very complex process in the embryo.
Chris - Alice Roberts. And also studying how the heart develops is Sheffield University's Emily Noel.
Emily - We're trying to understand how babies are born with certain heart defects. So, why they're born with holes in their heart, arteries that don't connect up properly, and we try and understand what genes make these process happen normally and why they go wrong.
Chris - How common are these abnormalities?
Emily - These abnormalities are the most common birth defect that there is, at least 1% of live births. Often these are sorts of defects that need to be corrected immediately postpartum and, quite often, even if you have surgical correction of these defects, individuals can end up with lifelong complications as well.
Chris - How are you trying to get to the bottom of why they happen?
Emily - We use embryological models - things like mouse or things like zebrafish to try and understand how your heart develops normally. Understanding how an organ develops normally is very important for being able to understand then what goes wrong. So we try and identify which genes are important for normal development and then we can systematically try to understand why these genes are important.
Chris - It is complicated but can you explain, for the likes of me, how does a heart develop and when?
Emily - The heart develops very early during embryonic development. So, in humans, your heart will have developed already by around four or five weeks after fertilisation, and the heart usually starts off as a very simple tube. This tube then undergoes quite a complex folding event, which is very important for making sure that your chambers line up properly, all your veins and arteries form properly, and it this sort of process of folding that we're very interested in and, if this process goes wrong, why you end up with defects.
Chris - So one tube bends itself into a series of wiggles, I suppose, and that gives you the sequence of chambers that the adult heart has?
Emily - Yes, that's correct. So one tube forms initially and this tube is already sort of roughly divided into what will become and atrium and what will become a ventricle.Those are the different chambers of the heart and then this tube will undergo two bending events which will mean that your atrium and your ventricle are going to be in the proper place in the adult heart, and that the sceptre between them can form properly.
Chris - Those are the walls?
Emily - Yes. Those are the walls of the heart which will separate your atrium and your ventricles.
Chris - And you're asking, well that must be obeying genetic instructions to form, so which genes are controlling it and, therefore, if it goes wrong, which genes must be going wrong?
Emily - Absolutely. So we look at all of these different aspects and say OK, what are the genes required for each of these processes and, if we don't have these genes, why doesn't the heart develop normally.
Chris - You make it sound very simple, but I'm sure it's not or you wouldn't be doing the research you're doing. How do you do that?
Emily - In my lab we use zebrafish embryos. We can either specifically knock down genes that we know are important in people and say OK, if we lose this gene in a zebrafish embryo, does it's heart not loop properly, and if it's heart doesn't loop properly, why doesn't it loop properly? And the other approach we can take is just to look in general at zebrafish that we know have heart defects and say OK, which genes have caused these defects?
Chris - You talk about fish though. How relevant is a fish to me as a human? I'm not a fish obviously.
Emily - No, of course.
Chris - Despite appearances may be deceptive.
Emily - Absolutely. Zebrafish hearts when it begins to form is very similar to the human heart. So it starts off as a tube and it undergoes looping events that are important for making sure that the chambers are lined properly. The zebrafish heart actually only has two chambers compared to the human heart, which obviously has four, but certainly these early processes of heart development are very similar. We know that a lot of the genes that govern this process are also very similar.
Chris - Once someone has been born with one of these problems, why is helpful you saying well we know which gene is was that caused that?
Emily - So there are a number of reasons why we try and understand genetically what causes congenital heart disease. One of those reasons is something as simple as genetic counselling. People who have these problems, they want to know why they they have congenital heart diseases. Information is very powerful and also it's very important that we can provide good advice to these people if they want to go on and have families of their own. So whether they're likely to pass these malformations onto their children too. The second thing is that if we know there's going to be a familial sort of genetic component to their heart disease that we can keep an eye on in pregnancies as they progress, and make sure that if there is going to be a need for surgical intervention, then that can happen as soon as it's pertinent to do so.
Chris - Some people also say, if we understand how the heart develops, we might be in a position to kickstart it into regrowing itself when it goes wrong and forming healthy tissue again in the context of disease.
Emily - Yep. And I think that's a particularly pertinent point when it comes to things like heart regeneration. So the zebrafish is capable of regenerating it's heart after it's had damage done to it and there is increasing evidence that, actually, embryonic genetic programmes are reinitiated in our hearts as it undergoes regeneration in the zebrafish. So being able to understand why these pathways are driving heart development may actually help us understand how we can activate regeneration in adults who have undergone things like a heart attack.

18:37 - Oh my cod! A treadmill for fish!
Oh my cod! A treadmill for fish!
with Professor Holly Shiels, Manchester University
Animals can form a key part of the work of investigating heart function. Holly  Shiels is based at Manchester University where she studies fish. Fish are useful to study because some species can survive in both hot and cold water, or even low oxygen levels, without their hearts giving out. If we can understand how, it will help doctors to develop better therapies for humans living with heart disease. Georgia Mills dropped by Holly's lab to find out how she studies them...
Shiels is based at Manchester University where she studies fish. Fish are useful to study because some species can survive in both hot and cold water, or even low oxygen levels, without their hearts giving out. If we can understand how, it will help doctors to develop better therapies for humans living with heart disease. Georgia Mills dropped by Holly's lab to find out how she studies them...
Holly - We work at a number of levels. We work with whole animals, we have a swim tunnel which is a treadmill for fish. We can put the fish in the tunnel and make them exercise by changing the flow of the water that these fish must swim against and changing the temperature and oxygen concentration to try and mimic the conditions in the environment and see how that affects the ability to swim.
Georgia - Is that here by the way - could we take a look at that?
Holly - Yes...
Georgia - It is like a bathtub with a sort of tunnel that, so I guess, you can look at the fish really easily when it's swimming along there. And it's not full of water at the moment but when it is you can just pump it through as fast as you want and, I guess, really put the fish through their paces.
Holly - But the funny thing is fish love to swim so you put them in a tunnel and they just swim. We don't make them go too fast and we don't make the conditions too difficult for them, just things would experience in the wild.
Georgia - And what can this tell you?
Holly - Well the first thing we can do is to look at how they swim. The link between that and the cardiovascular system is that the heart really underlies all performance aspects of the fish, and so we can ask it to swim under different conditions. We can also put probes on the fish to measure heart function while it's swimming. The simplest is measuring EGCs or electrocardiograms that are fairly noninvasive just from the centre of the surface of the fish and we can measure ECGs or heart rates during exercise. But we can also do more invasive things: putting flow probes on, measuring pressure, measuring blood flow...
Georgia - What are you hoping this will tell us when you get all these readings?
Holly - Well, it will help really tell us whether or not the cardiovascular system is responsible for it's ability to swim and what aspect is it. Is it the pumping ability, is it pressure development, is it the electrical ability? That kind of leads me onto some interesting work we were doing up in the Arctic last summer. We were looking at a fish called the Arctic Sculpin. We know that there's two populations of Arctic Sculpin. The one that was in this polar area seems to be progressively outcompeted by it's more temperate cousin, the Short Horn Sculpin. So we were looking at the sensitivity of both of their hearts to increases in temperature and we were using ECGs to look at the stability of the electrical activity of the heart as temperatures increase. So that can tell us if one species has a more electrically stable heart than the other species and, if it does, that might affect it's ability to migrate into different temperature zones.
Georgia - Before I ask you what you found out, I've just got to ask, applying an ECG onto a fish in the Arctic... this sounds like a story.
Holly - It was exceptionally interesting. We were working at a research station in the Arctic so we did have a lab and we did have the ability to try and do this. This wasn't out on a ship in the middle of the ocean. Our biggest problem was that our Sculpins started eating each other in the tank...
Georgia - Oh no!
Holly - So we ended up having less species by the time we got to finishing all the experiments. But it was certainly an adventure and I don't think we got the answer but, at this point, there are indications that the one with more thermal tolerance, it's heart was able to withstand higher temperatures better.
Georgia - Do we know why it's heart is better able to tolerate these changes in temperature?
Holly - Well it kind of comes to another way we do our work. So we can look at the whole heart function but we also work on the level of the single myocyte a lot of the time. Myocytes are the individual muscle cells that make up the working portion of the heart. So they're the parts that contract with each heartbeat and relax to allow the heart to fill. What we can do is take a heart and digest it using enzymes into these individual cells and then we can use a technique called voltage clamp or using iron imaging to look at iron flow across the cell membranes. That can tell us which of the different components that allow the heart to function are affected by the environment.
Georgia - What has this told you about what makes the heart adaptable and what doesn't?
Holly - Well I think that we've certainly... This isn't my work, this is the work of one of my colleagues in Finland, Maddy Van Eman. He's been able to show that the sodium channel is fairly temperature sensitive and might set the ability for the heart to work at high temperatures.
Georgia - And what are these sodium channels for?
Holly - The are the channels that open in the cell that initiates muscle contraction.
Georgia - I see. So the thing that helps the heart to bumbum, bumbum at the cell level might be what is key to different species being able to do well in certain conditions?
Holly - Yes, exactly. But what's also interesting is it's the same ion channels that control the bumbum, bumbum across all species. So whether or not we're looking at a fish, we're looking at a reptile, or we're looking at mammals and humans, we still have the similar components of ion channels, and so we can use fish or reptiles really to get deeper understanding about how the heart works as a whole and, hopefully, be able to use the information there to probe or to ask questions that are relevant at the level of humans as well.
Georgia - OK. So what kind of things that might be relevant to humans have you come across so far because I know I was wondering how similar to humans is a fish heart? So what kinds of things have your found?
Holly - Well, they're certainly different at the whole heart level, but at the ion channel level there's some similarities and, in a sense, that's been quite instructive for the some recent work that we've been doing looking at the effects of pollutants on the cardiovascular system. We came into this work a few years ago when we were asked to help understand the implications of the Gulf oil spill on the pelagic fish (the tuna, the mackerel), and we looked at the effects of different components of the oil.
Georgia - And what did you find?
Holly - We found that oil is not good for heart cells. It causes the cells to lose their electric ability.
Georgia - I imagine if the cells lose the ability to contract and relax at the regular intervals that they need to do that could lead to the heart not beating the way it's supposed to?
Holly - Exactly. And we also found that it also affected the calcium channels and these calciums, the ion that is actually responsible for heart contracting and for the heart relaxing, so it was affecting both the contractility and the electrical activity.

25:03 - Pollution leaves us heart-broken
Pollution leaves us heart-broken
with David Newby, University of Edinburgh
The WHO rate bad air quality as one of the leading causes of heart attacks and  strokes worldwide. It's also known that people who lay asphalt have a much higher rate of heart disease. David Newby, at the University of Edinburgh, explained to Chris Smith how he is investigating why this is.
strokes worldwide. It's also known that people who lay asphalt have a much higher rate of heart disease. David Newby, at the University of Edinburgh, explained to Chris Smith how he is investigating why this is.
Chris - But it's not just fish that are exposed to oil-based pollution: bad air quality is now considered to be one of the leading causes of heart attacks and strokes worldwide. Dave Newby, at the University of Edinburgh, has been investigating how...
Dave - My name's Dave Newby, I'm a British Heart Foundation John Wheatley Chair of Cardiology at the University of Edinburgh.
People have observed for quite a while that high air pollution has bad health effects and that's been known since the mid-1900s. What people have appreciated more recently is that beyond the obvious that air pollution can make your breathing bad, it actually increases the risk of heart attacks and strokes. So that's where I start to become interested because of this association of air pollution and you having heart attacks and heart disease. And not only getting it over time but also there's evidence that it actually triggers a heart attack.
Chris - This isn't just because people who are struggling to breathe that's just a stressful situation and that makes them have a heart attack - there's something more going on?
Dave - That's right, yes. It's more than that because the pollution that's in the air is actually sometimes imperceptible . The particles in the air are so small you can hardly see them, so it's not that. People keep asking well, what's the mechanism of that? OK, you see the association but it doesn't make sense to me. So what we did we set off on a programme of work to look at the mechanisms of how air pollution can do this and it was in many ways quite intriguing. So what we did was we worked with some investigators in Sweden. We went there because they have a unique exposure chamber and they have, of course, a Volvo engine. So what we did we had this diesel Volvo engine and we diluted down the exhaust and then fed it into this chamber which, of course, did raise some eyebrows I have to say.
Chris - Hang on a minute! You put people in a chamber and you blow in car exhaust for them to breathe?
Dave - Absolutely.
Chris - How did you get that through an ethics committee?
Dave - That's exactly what the British Heart Foundation said to me. And what was quite interesting was when I pointed out to them the levels inside this chamber were lower than the levels outside their front door because, at that time, they were in a very, very polluted area of London which was absolutely the highest levels in London recorded just round the corner. So I said to them if it's ethical for them to invite me down from Edinburgh to London to their polluted city and go on their committee, then it's ethical for me to do that. And it was diluted of course so the levels that we have are the levels you would expect at the roadside of a busy road and so this was relevant to what we see in the cities.
We got people to exercise gently in those chambers to breathe in this and then we looked at how their blood vessels responded. Now what we found was that the blood vessels were more tight and more constricted, they didn't relax as much, and the blood that flowed through it was much more sticky, and much more likely to cause blood clots. And those two things together, blood vessels that aren't relaxing, that are tight and have blood clots are just the recipe for heart attacks and strokes.
Chris - Do you know what component it was in the smoke that was doing that?
Dave - Yes. So in the exhaust, there are various different things. There are gases but there are also these particles. They are really tiny particles so they are so small you cannot see them by the naked eye. They are what we call nanoparticles - really tiny. It seemed to be those particles and they're covered in bits of metal, bits of unburned fuel, organic components, metals, and these things can react quite nastily to biological tissues, and what we were able to show was that it seems to be these tiny microscopic particles are what seemed to be causing the problem.
Chris - Just because you breathe them in or do they go further afield in you body once you breathe in?
Dave - Yes, that's a very important question and, actually, if I'm truly honest we don't really know for certain but there are three potential mechanisms. One - it goes into the lung, the lung doesn't like it and sends out messages to the rest of the body. Another mechanism is that they go deep into the lung, they get gobbled up by the cells of the body (the immune cells), and then they go into the bloodstream, and there they might harm the blood vessels, or they could even go straight into the bloodstream. We have some some preliminary data that these particles are so tiny, so small that they can cross cell membranes and get into the bloodstream. There they might actually cause the furring up of the blood vessels and cause heart attacks and strokes.
Chris - What about actually monitoring the real life experience of people in real life situation to see what their exposure is. Can we do that - do we have that sort of data?
Dave - We do. We can use personal monitoring so you wear this lovely backpack which monitors the quality of the air. It measures the particles, the mass, the number of particles, the gases in the air, and so you've got like a portable laboratory on your back. And we walked around Beijing just before the Olympic Games and we were able to see the quite dramatic levels of air pollution there.
We actually then went on to do a study where we got patients to wear a face mask. It's an industrial mask, this is not the simple cloths that you see people put in front of their faces. But this is a mask that's very efficient, takes out a lot of these particles and when we got people to walk round just for one day with these masks on, their blood pressure was lower, their breathing was easier, and some of the measures that we did of how much heart stress they were under were much lower. So actually stopping breathing in some of these particles in the air around you does seem to have benefits for the body.

30:19 - Can obesity harm your grandchildren?
Can obesity harm your grandchildren?
with Susan Ozanne, University of Cambridge & Lucilla Poston, King's College London
One factor which we know can harm your heart is being overweight - it makes you more likely to have high blood pressure and heart attacks, but - if you're pregnant, it can also increase the blood pressure of your child, or even your grandchildren. Chris Smith caught up with two researchers who are looking into why this is happening. Susan Ozanne is from the University of Cambridge, and she outlined the evidence that this is indeed happening....
you more likely to have high blood pressure and heart attacks, but - if you're pregnant, it can also increase the blood pressure of your child, or even your grandchildren. Chris Smith caught up with two researchers who are looking into why this is happening. Susan Ozanne is from the University of Cambridge, and she outlined the evidence that this is indeed happening....
Susan - From human studies actually, some of the strongest evidence is when we look at children, currently living in the same household, born to the same parents, but from pregnancies that occurred either before or after the mother had bariatric surgery, so therefore from pregnancies where she was either lean or obese.
Chris - So bariatric surgery are these sort of gastric banding surgeries that help people to shed weight?
Susan - Exactly.
Chris - And you're effectively saying look, we've got the same parents, the same environment. So the genes are pretty similar, the environment's the same but the only thing that's different is the weight, so you can compare the two?
Susan - So if you look at those children who were born from pregnancies after the mother had lost weight and she was lean. They are slimmer, they have lower blood pressure, and they're more insulin sensitive so they're less likely to get diabetes.
Chris - Insulin being this hormone that controls sugar?
Susan - Yes. So insulin is the major hormone in our blood which, when we eat a meal, makes sure the blood glucose levels don't stay high. It makes the blood glucose go into muscle where we store it and also into fat tissue.
Chris - And when you say children, are we talking throughout childhood and into adulthood or are you saying just when their born? When does this effect manifest?
Susan - So you can see evidence for it very early on, but for the studies they've looked at people right up until their 20s and shown effects right from 2 years old right up until they're in their 20s
Chris - Striking that something that should be happening when that baby is just in-utero, just 20 weeks, should have 40 years of legacy or more.
Susan - Or more because, as I mentioned, it can also, potentially, impact on the next generation as well.
Chris - How?
Susan - So we think what obesity during pregnancy is doing is impacting on how our DNA is used. So it's not changing the DNA sequence but the genes that we're using within our genome, and how much we're using them differs, because of a response to the environment. It's almost like you're in a library and you've got a whole load of books but it doesn't mean to say you're going to read all those books, it's the ones you pick of the shelf that are going to determine which ones you read.
Chris - So we have a baby, it's growing in it's mother, the mother is determining the environment the baby grows up in. If the mother is obese, there will be some kind of change to the environment that the developing infant is experiencing, this has an effect of chemically changing the DNA and that effects what genes are turned on or off or how much...
Susan - Exactly.
Chris - So that affects the baby that is developing there and then, but how does that influence the next generation?
Susan - So that will determine how likely that baby is to develop diabetes, for example. How likely that baby is to have high blood pressure. How likely that baby is to have a heart attack. Now, obviously, that baby themselves when they become pregnant, if she's more likely to get diabetes, for example during pregnancy, then you will again have an impact on the next generation even if her diet has been totally normal.
Chris - I thought you might be going down the route of well, if you're having a daughter, when that baby is developing then inside her is her future ovary with all of her future eggs and, therefore, half of the genetic information of her children, your grandchildren in there.
Susan - Yes, and that will also contribute as well and, actually, the same thing is happening from sperm as well. So there's more and more evidence to show that dad's diet also impacts on the sperm and then how that will impact on the next generation.
Chris - As well as these so-called epigenetic changes, there are clues from animal studies that there may be changes going on in the developing brain. Lucilla Poston, from King's College London.
Lucilla - So what we've done is we've made mice and rats fat. We've given them delicious things to eat so they're very happy to do that, and they get fat when they're pregnant. We've looked at the offspring as they're growing up and we have found, just as has been suggested by the human studies, that the offspring do get fatter and they also have high blood pressure, and the focus in terms of mechanism is pointing towards an area of the brain which is called the hypothalamus and that area in terms of development is the womb is very susceptible to nutritional influence. So in the later stages of pregnancy when this area of the brain is developing, we know that nutrient hormones can actually change the way it develops. So you can imagine that if you hardwire the networks of the brain's neurons, you might actually change either the blood pressure or the fatness of the child because that area of the brain is very responsible for controlling both of those outcomes both in terms of the hunger, the satiety of the child, and the blood pressure of the child.
Chris - So there is a physical change in the connectivity of the bits of the brain that are determining blood pressure, how your heart works, and also your future appetite if you are exposed, during development, to a sort of obese environment?
Lucilla - You can change the development of the hypothalamus by the nutrient hormones which surround it during development. That's been shown experimentally, there seems to be no question about that. We can't look at that in people, so we can't categorically say this is happening in mums and their babies but the evidence from animal studies is certainly very positive that that could be one of the mechanistic pathways.

36:31 - Bleeding heart treatment
Bleeding heart treatment
with Professor Colin Berry, University of Glasgow
Heart attacks are very common, but thankfully many more people are surviving  them these days. The downside though is that victims often suffer health effects afterwards, like chronic heart failure, despite getting to hospital quickly and undergoing emergency treatment. It turns out that opening up blocked arteries that cause heart attacks tackles only half the problem. To explain why, and what happens when a person suffers a heart attack, Colin Berry, professor of cardiology at the University of Glasgow spoke to Chris Smith...
them these days. The downside though is that victims often suffer health effects afterwards, like chronic heart failure, despite getting to hospital quickly and undergoing emergency treatment. It turns out that opening up blocked arteries that cause heart attacks tackles only half the problem. To explain why, and what happens when a person suffers a heart attack, Colin Berry, professor of cardiology at the University of Glasgow spoke to Chris Smith...
Colin - Classically, it's the sudden blockage of one of the main arteries in the heart and that is typically caused by the breakdown of the wall of the heart artery because it's diseased. Fatty plaque has accumulated at one or more places, the plaque ruptures, that exposes the constituents of the wall of the artery to the blood and normally they don't meet, but when they do they're not a great mix and a blood clot forms and that blood clot leads to loss of flow in the heart artery that is experienced by the patient as chest pain.
Chris - Does that mean that the heart downstream of that blockage, that part of the heart is destined to die unless someone like you comes along?
Colin - Yes. Bluntly, that is the case and, within 60 minutes almost certainly, some of those heart muscle cells will have started to die off and within 2 hours it will be threatened and beginning to die off almost irrecoverably.
Chris - What's the current gold standard treatment? What's the best way do we think at the moment of managing a person in that situation?
Colin - The whole team is working in emergency care circumstance to achieve restored flow in the heart artery as quickly as possible. We put a plastic tube in the wrist, we put a long catheter to the heart arteries, we inject dye using camera imaging, and we identify the blocked artery and, as quickly as possible, we pass a wire through that blockage, open the blockage by placing either a balloon or, indeed, sucking out the clot. Whilst the situation looks so much better with flow restored in the heart artery, I know from my research that there is a different story that is operative at the level of the heart muscle.
Chris - Go on...
Colin - All the small vessels in up to half of patients are all blocked.
Chris - What do you mean?
Colin - So the treatment pathway focuses on the main artery, which is large, but that artery has myriads of small vessels. Imagine the arborisation from a tree; these small vessels and all the little leaves are all blocked with microclots.
Chris - Is that something that happened at the time that the patient had the initial event or are you saying that in going in and focusing on getting that clot out and opening up the artery, all we've done is export the problem downstream? We've broken bits of it up and they've floated off down the artery and lodged making more blockages downstream?
Colin - Yes, that is a very likely scenario.
Chris - So what you're saying is you have taken patients in in which this intervention has been carried out and you can see evidence that these vessels are blocked after what we currently regard as the gold standard treatment of unclogging arteries?
Colin - It represents a limitation of medical practice. We have focused on the main life-threatening problem and successfully treated the patient in that regard, but it has left a legacy of problems within the small vessels of the heart that can lead to heart failure in the longer term.
Chris - What are you proposing to try and do about this?
Colin - Historically heart attack was treated with a clot breaking drug. What we propose to do here is to give a small dose, a fraction of the dose, directly into the heart artery to break down all those microclots. That is the focus of this new trial called Ttime.
Chris - The idea being then that you go in, do what you've just described. You still open up the artery but anticipating that you will dislodge stuff that's going to go downstream and block those vessels. Anticipating that's going to happen, at the same time you're going to put in some clot busting chemicals which will hopefully prevent those other small blood vessels getting blocked or unblock them if they are blocked already, and that should reduce the risk of onward complications?
Colin - And we have to wait for a couple of years to know the answer to that question.
41:17 - Radioactive toothpaste!
Radioactive toothpaste!
with Marc Dweck, University of Edinburgh
Better than trying to rescue a heart damaged by a heart attack is to try to prevent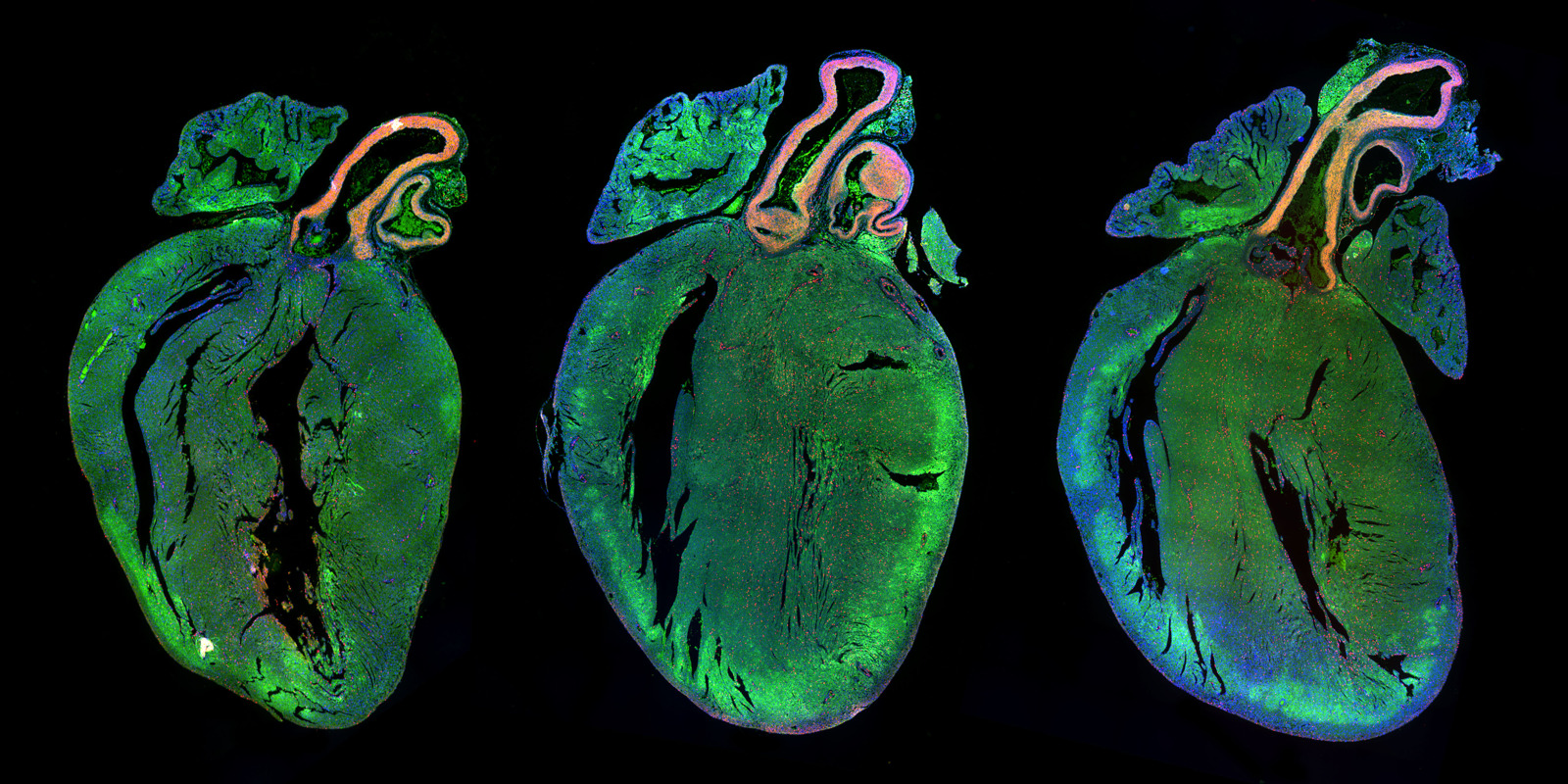 one happening in the first place. And Edinburgh cardiologist Marc Dweck, has a new method for spotting heart attacks waiting to happen, as he explained to Chris Smith.
one happening in the first place. And Edinburgh cardiologist Marc Dweck, has a new method for spotting heart attacks waiting to happen, as he explained to Chris Smith.
Marc - Yes, so at the moment when we assess these coronary arteries the easiest thing to look at are there any narrowings there. But what we've learnt is that actually the majority of heart attacks appear to have started where there isn't really a narrowing at all and so we need new techniques that go beyond just looking for narrowings. Looking at the components of that plaque, looking at the activity of those plaques to get a better sense of which of the plaques that are causing a problem and who are the patients who are more at risk of having heart attack.
Chris - What are you doing then to get a clearer picture of what's going on in the risky bits of the arteries? How are you trying to spot them?
Marc - So we have a new imaging technique called PET imaging. Essentially this is where we inject traces in the body that tell us the activity of diseases processes as it's occurring in the body. So we can start to look at the coronary arteries, to look at plaques and say right, this plaque is active, it is doing something at the moment. This is not a patient who has stable coronary artery disease, this is someone whose disease process is active. And our hypothesis is that if you identify the active people, you're going to identify people that are at higher risk.
Chris - What do you inject people with?
Marc - It's radioactive fluoride, I guess. Radioactive toothpaste effectively. This has actually been used for many years to look at bone. We're now using it to image calcification activity in the coronary arteries.
Chris - So does calcium go along with dodgy bits of artery that might have a heart attack risk then?
Marc - Actually, we think that the calcification process is a healing process. So you have lots of inflammation in the artery and then the body tries to heal it up by calcifying it. If we see the early stages of that calcium, then we know that there's a nasty plaque there that the body is trying to heal but it hasn't healed it up yet.
Chris - And this injection of radioactive toothpaste, the radioactive fluoride, that can highlight those early stage lesions can it?
Marc - Yes, we have looked at this in great detail over the last couple of years with Cambridge University, as well as Edinburgh, and it looks like this fluoride is binding to the very early stages of the calcium. So we are very excited about it.
Chris - So if you did this test on somebody and you saw a patch of artery that flashed up very hot on you PET scan with your radioactive fluoride marker suggesting to you this is a plaque which is very rapidly evolving, it might be a heart attack risk, what are you going to do for that patient then? How would you manage them?
Marc - Yes, that's an excellent question. I think there's two kind of schools of thought on this. One is that right, if you see an active plaque, a nasty plaque, then maybe you can try and stabalise that particular plaque.
Chris - How? What do you mean by stabalise?
Marc - So people have thought about maybe trying to put a stent into that plaque to stop it from rupturing. To strengthen the wall of it, I guess. Personally, I don't believe that's the right approach because what often happens is you see one active plaque at a moment in time but this is a dynamic process. That plaque might heal up OK, but another plaque may develop in another area and so, actually, I think the best chance of us preventing events is to use drugs. Things like statins, things like aspirin that kind of treat all the plaques at the same time and, in particular, we are developing very powerful drugs that really lower cholesterol levels a lot, but they're very expensive. And so we need to be able to target those drugs to the patients that are at the highest risk and so I think that's the space where this kind of imagining technique may have a role where you're really trying to identify those at the very highest risk that are going to benefit from the most aggressive expensive treatments.

45:30 - MAMILs: To run or not to run?
MAMILs: To run or not to run?
with Dr Sanjay Sharma, St George's University of London
One way to keep your heart pumping is to become a MAMIL: a Middle- aged-man-in-lycra! A phenomenon that has men in their 50s getting out and doing lots of running - but there's also a worry that over-exerting can actually be what causes some 'MAMILs' to have a heart attack. Georgia Mills caught up with Sanjay Sharma, from St George's University of London, to find out if running can ever be dangerous...
aged-man-in-lycra! A phenomenon that has men in their 50s getting out and doing lots of running - but there's also a worry that over-exerting can actually be what causes some 'MAMILs' to have a heart attack. Georgia Mills caught up with Sanjay Sharma, from St George's University of London, to find out if running can ever be dangerous...
Sanjay - We all know that exercise is good for you. People who exercise regularly have a favourable lipid and blood pressure profile, they are less likely to be overweight and diabetic. And by controlling all these risk factors for atherosclerosis, which is what causes heart attacks, they reduce their risk of dying from a heart attack by 50% when they reach their 50th or 60th birthday. So everybody knows that exercise is very good for you, and everybody should be doing it to gain an additional 3 to 7 years of life.
But what the MAMILs all about is a 40-60 year old man, gets to middle age and sees the middle age spread around the abdomen and decides I need to do something about this because I've heard that people who don't may die from a heart attack. They often join the gym or a running club and they soon realise they are as good as people who are younger than them. And the good news for everybody is that as one ages, of course the facial expression changes, the hair changes, but what doesn't change very much is your skeletal muscle and your ability to engage in endurance events. To give you some idea, if we look at the average times of marathon finishes between 20 and 49, there's not much difference.
Georgia - Wow! Is this true of men and women?
Sanjay - This is true of men and women. So, of course, men realise at the age of 40 or 50 that they can actually beat people who are younger than them and being ultra-competitive, this drives them on and that is usually what gives birth to the Middle Aged Man in Lycra who spends most weekends competing and exercising, and this is very, very, good for you. The one thing that everyone worries about a little bit, of course, is that is paradox that although exercise protects from heart diseases it can, in some people, precipitate or trigger a sudden death, usually in someone whose got a silent cardiovascular abnormality. We actually look at the demographics of people that die; they are usually middle aged (between 43 and 55), they're almost always men...
Georgia - So, as you say, there are clues then at who might be more at risk?
Sanjay - Around 55% of people who die have already got established risk factors for coronary heart disease so that's one thing to look for and try and rectify. One can rectify someone's cholesterol, or blood pressure, or even sugar control.
The second thing is that about 15% have a previous cardiac history and, what's worrying, is that about 30% of people have reported symptoms suggestive of cardiac disease such as chest tightness that's brought on by jogging, or breathlessness that disproportionate to the amount of exercise being performed, or palpitations or a feeling of dizziness during exercise. These are all ominous symptoms.
So the things to look for are: am I overweight, have I got a high cholesterol, have I got high blood pressure, am I diabetic, has someone in my family died below the age of 50. These are all warning symptoms and if you've got those, you do need to be assessed in a professional physician setting.
Georgia - Every now and then on the marathon you do see someone who's dies unexpectedly during it. And maybe it doesn't happen that much but does stick with you and I guess it's worrying. You think should I exercise, are the benefits worth it? What would you say to that?
Sanjay - I think everybody in this country, in fact, everyone in the universe must exercise. There is no medication invented yet that has the benefits of exercise i.e. anti-aging, preventing cardiac diseases, preventing depression, preventing dementia, preventing osteoporosis. If we packaged up exercise into a pill, it would be known as the miracle pill and, unlike medications, exercise is free, it can be performed at any time, and it's usually devoid of some of these side effects that you get with medication, so everyone should be exercising. The amount of exercise that you need to do is about 30 minutes of moderate exercise five times a week. By that, I mean a jog at a 15 minute mile pace, so four miles an hour. That's what you need to do to achieve these benefits. That's not to say that you have to do that, you can do less and still achieve benefits compared to people who don't do anything.
Now in terms of marathon running, I want to allay your anxieties. The death rate in marathons is about 1 in 50,000. The reason why it appears more is because many marathons, such as the London marathon, are under the radar of the media and are televised, so when something does happen to someone who's actually trying to raise money for charity by doing something that's good for them, it does to really, really captivate the audience, it captures the heart of the nations, but these deaths are rare. They're usually due to people who already have predisposing factors to cardiac disease. So I would say that if you've got any of the risk factors I've just talked about, then you should be tested out before you embark on something like marathon running.

50:45 - Heart transplants: the cutting edge
Heart transplants: the cutting edge
with Stephen Large, Papworth Hospital Cambridge
Heart failure is when the heart simply can't pump enough blood around the body, and it's so prevalent it costs 2 percent of our GDP! Transplants come from people who are brain dead, with permission of the families, and taken off life support. Stephen Large, a surgeon from the world-leading transplant centre, Papworth Hospital in Cambridgeshire, may have discovered something which might improve people's chance of getting thrown this lifeline in the first place.
and it's so prevalent it costs 2 percent of our GDP! Transplants come from people who are brain dead, with permission of the families, and taken off life support. Stephen Large, a surgeon from the world-leading transplant centre, Papworth Hospital in Cambridgeshire, may have discovered something which might improve people's chance of getting thrown this lifeline in the first place.
Stephen - We look at heart failure in sort of stages if you will, and we're looking at patients for heart transplantation who are stuck in the severe category of heart failure. So they're breathless at rest or they're persistently tired. Their exercise ability is very, very limited; their lives are so contained, dreadfully contained by the restrictions of their heart failure, they're pump failure, despite best medical therapy, and those are candidates for transplantation. And, of course, we find that the younger people tend to do better with transplantation than older folk, which is a little ironic because heart failure is an age-related issue. We heard today in this conference, 20% risk of heart failure developing in those over the age of 65, and that's a daunting prospect as you approach 65 - not great.
Georgia - In terms of actually taking the heart out of someone who no longer needs it, I suppose, and putting it into someone who does. This sound incredibly difficult. How long have we been able to do this and what are the success rates?
Stephen - Well, I was a secondary school student when this whole area exploded and, of course, Christian Barnard hit the press in '67 with his transplantation of Wychenzky. There was a big flurry of transplantation after that and folk didn't understand really the ups and downs of immune suppression because, of course, you have to damp down the recipient of the heart's immune system, otherwise they'll reject it, like any foreign protein. So we have to get the patients to have immune suppression so they tolerate the new heart and it keeps them going, and very effectively so too. As we saw again from statistics today, survival moving from a 50/50 chance of those with severe heart failure of 1 year to 50/50 survival after transplantation of 13 years, which is amazing, absolutely incredible therapy. And not just survival but, of course, a quality of life benefit hugely impressive.
Georgia - So how does one of these transplants work? Well, last year, BBC Radio 5 Live made history and did a live recording from one of these operations, and we've got a clip here that give you a small idea of just how incredible these procedures are...
Chris - So this is my first look proper into the operating theatre and you can see Steve's head right in front of me just coming out of the top of the bed. Various tubes connected to the top of his head and coming out of his mouth as well. And if I just come over to my right as well, pretty much the most important machine in here which is effectively doing the job of Steve's heart, working out the circulation of Steve's blood around his body whilst his heart can no longer do so. One, two, three surgeons right next to Steve and doing all of the main work, and then we have a perfusionist here who's operating that machine I was talking about that's doing the work of Steve's heart, and then the anaesthetist just to the left as well. And they know that they've got a long road ahead.
Let's have a quick word with Laura who is the transplant coordinator. So just tell us where we are at the moment because they've been working for some time already? What stage are we at here?
Laura - We're at the stage where we're preparing to explant the heart here from Steve, so he's on the bypass machine now. So Mr Howell is just loosening the heart and preparing to take it out properly and in the background we are waiting for his new heart to be delivered to us. So we've got the timings quite strict and we're hoping that will happen within the next half an hour.
Chris - And when you say the timing's quite strict. I mean it's actually incredibly tight isn't it? It's effectively a race against time?
Laura - Yeah. It's a four hour window that we have when we stop the circulation and the blood supply of the old heart and transport it on ice and need to be reperfused in Steven's body. So it's crucial and, obviously, you've got transportation time to factor into that as well.
Chris - Just as a reminder, at this moment in time, we're heading to a critical stage here, aren't we now?
Laura - Yes, it's crucial now because we're getting anxious that the heart will be on it's way to us and we need to make sure that we're ready because we just want to cut down the amount of time that the heart is on ice as much as possible.
Chris - Well the heart has just been taken out. I'm going to come round this way because the heart has just literally been taken out. You might have heard the surgeon, Neil Howell, just say the heart is out so that everybody in the room knows. And here it is on a table in a plastic bowl. It's quite a sight, it's quite a size, it's bigger than I would have thought, and it's just made a movement there completely independently from Steve's body as well. Now what they will be doing at the moment is preparing Steve's body for when the new heart arrives and in front of me, effectively, is a man who, at this moment in time, does not have a heart in him, which is quite a thing to consider. And also to look at what is now going to be his old heart in front of me and, again, as I look, it's still moving even though it's no longer in Steve's body, which is quite a thing to see and I've seen that happen about 6 or 7 times now. That will now go for various tests and now we await the arrival of the new healthy heart....
Neil Howell - how are things going here?
Neil - Well they're going pretty straightforward really. So you can just see in here at the moment when we look in, this is the cavity that's left by the heart being removed and you can see what a huge space there is there. And you can see down here we've got what we call the cuff, so this is the residual heart tissue, the residual blood vessels that we're going to sew the new heart into. We've got absolutely everything prepared, we're all ready. I've got my first suture already placed at the top of the left atrium so, the second the heart comes in, I can take it out, inspect it and start implanting it...
Chris - So the box has been opened. There's some paperwork and such like in the top and then it's full of ice. The ice being scraped back . Ice as you would picture it a cool box...
And one of the team here rooting through that ice. What's happening - what's it protected by?
Neil - Okay. So this is the standard way of protecting the heart when it's getting transplanted so it's triple bagged and literally just packed in ice. So this is when the coordinators get a little bit stressed and they don't like it. What they're doing is cutting through the first bag without trying to cut through the second or the third bag. And what they're going to do is they're going to open this up and then I'm going to reach my hands in into the sterile interior of this and I'm just going to lift the heart out. Then we'll move it to this bowl over here. So as soon as I see what I want to see which is that bit there and this goes into an empty bowl at this stage just because there's a lot of water.
Chris - What's the heart floating in there?
Neil - It's just some saline, so salt water
Chris - Picking the heart out there, orientating it around.
Neil - That's where it's going to sit so..
Chris - I mean this is absolutely amazing stuff to see. The work they're doing here where they're just treating this heart with great care but, at the same time, preparing it in order to put it in. So here we go then...
Neil - Okay, so first stitch goes in...
Chris - Just to tell our listeners now. Neil Howell has got his instruments deep into Steve's chest bringing the heart into that cavity that we talked about and now the heart's sitting inside there. As I said, that area about the size of a small football. Quite whitish walls around his chest and some more ice thrown into the area as well just to keep that heart as cold as possible even though it's now sitting loosely in Steve's body. And Mr Howell just trying to manipulate the heart to try and move it into the correct position. He's got both of his hands in Steve's chest now which he was talking about earlier...
Neil - What I'm trying to now is just open up because I'm doing a sort of upside down anastomosis right at the back of this guys chest . So what I need to be able to do is just to.. Thank you, trying to drop the instruments.. Is to try and now see what I'm doing because as I do this anastomosis I gradually see less and less of what I'm doing. I'm just trying to keep in the same position really. I'm just opening up the donor left atrial cavity so I can see where I am stitching. You know there's lots of old phrases in surgery and one of them is "if you can see what you're doing it's generally an easy thing to do." And half the problem, I think with surgery, is just not being able to see what you're doing half the time.
So the heart is no completely finished. You can see the heart's just starting to beat so we've connected half the joints and the heart's just starting to beat
Chris - Mmm. And that's quite a sight isn't it? From the heart being brought in completely still in ice and now we see the new heart inside Steve pumping. Pumping away.
Neil - It's not pumping. So it's not doing any work - it's beating.
Chris - It's beating. Yes, okay, I see the distinction.
Neil - At the moment there's not a lot of blood going to this heart because it's all going round Ruthy's machine. But it's starting to beat and that is a good sign.
Georgia - That was Chris Warburton following Steve's transplant. But people like Steve are often sat on the waiting list for donations for months, even years. Back to Stephen Large...
Stephen - The central issue here is really the huge imbalance between the supply of hearts for transplantation and the need for it. We're an ageing population, the need is going up, and the number of organs available is actually going down. Why? Because public health is so good. People are wearing crash helmets, they're driving at sensible speeds. It's a demonstration of fantastic outcomes from public health.
So we've been looking at alternatives. And so what we've been doing in Papworth is to ask the question, what about those poor folk who have no therapeutic outcome for their devastating brain problem and treatment is withdrawn at the relative's request and the intensive cares request. And for a number of years now those folk who have treatment withdrawn, their hearts stop and they have gone forward for organ donation.
And up until recently the question of using the heart from such donors hasn't been an issue but we've pushed and said these are appropriate hearts, and we've shown that in modeling in rat and a pig model, they're going to be very appropriate hearts. Perhaps even better than the current ones we use. And so we started a program after ten years of justification on the 28th February 2015. Hugely exciting and to date the country has transplanted 23 hearts. The majority at Papworth and 4 from our sister hospital in Harefield, and this is a hugely exciting development. We think that at least 50 further heart transplants will be offered to program through this development, so it's pretty exciting stuff. But the frustrating thing is the demand is still so much greater and I think, sadly, that demand will always be greater than supply whatever fabulous innovations we come up with
But, in the meantime, let's encourage everybody, everybody to get onto the organ donations register. Opt in and help somebody.
- Previous Genes for all
- Next Turning Carbon Dioxide Into Stone










Comments
Add a comment