Autopsy: A Matter of Life and Death
This week on the Naked Scientists, we observe a post-mortem. The patient was in his seventies but the coroner ordered an autopsy because the cause of death wasn't clear. Chris Smith observes pathologist Alison Cluroe conduct the procedure as she tries to find out why the patient died and sees how this once common practice is still saving lives...
In this episode
00:59 - How have post-mortems changed?
How have post-mortems changed?
with Dr Suzy Lishman, President of the Royal College of Pathologists
We've been conducting autopsies for hundreds of years but they weren't 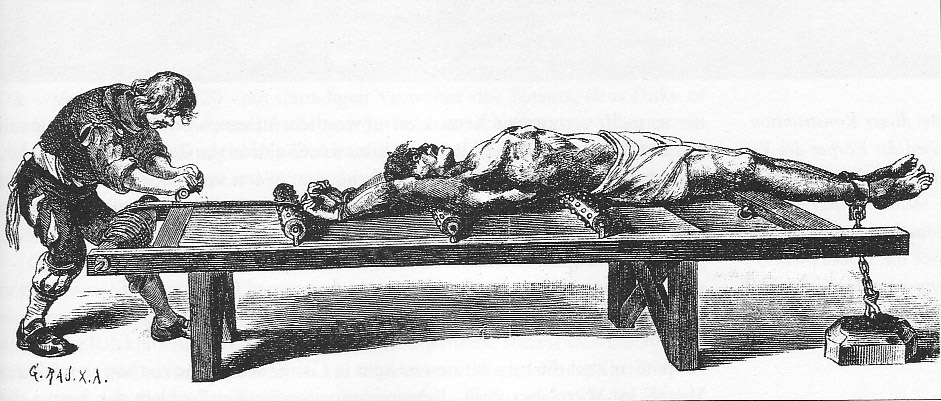 commonplace and often used as a criminal punishment, as Suzy Lishman explained to Chris Smith...
commonplace and often used as a criminal punishment, as Suzy Lishman explained to Chris Smith...
Suzy - Well for centuries it wasn't allowed at all. It was against people's religion, or against their cultural beliefs, certainly it wasn't seen as something that was desirable. Over the years, for example, post-mortems have been used as part of the punishment that criminals have. So if they were executed, for example, perhaps their body would then be donated for dissection and for teaching purposes. So, I think, although the value of the post-mortem was recognised, it wasn't something that anyone would volunteer to have done.
Chris - And when did the law change and people decide, well it's pretty important to know why someone's died and we're going to make this part of that process?
Suzy - In the last 100 years or so, it's become increasingly clear that post-mortem examinations reveal a huge amount of information and so they've become increasingly accepted. And at some point, in some places, it's become absolutely normal that if you die in a particular hospital or if you die following surgery, then it's standard practice that you have a post-mortem examination.
Chris - It's quite stigmatised though, isn't it? A lot of people are quite suspicious, or concerned, or worried by the prospect of a loved one having a post-mortem. Is that because of its historical underpinnings?
Suzy - I think the history of post mortems hasn't helped. So if post mortems were seen as a punishment or something that was only done to you when you had no say in it then, obviously, people are going to be suspicious and not want to have it done. But I think there were quite a few misconceptions about post-mortems. There actually just really like... I've often referred to it as like the final operation, so it's like having surgery in an operating theatre except you haven't got all those machines trying to keep you alive.
So it's completely respectful; the post-mortem is done in a standardised way and people are treated with the dignity and respect that they deserve. And pathologists never forget that the person they are examining is somebody's loved one, someone's son, someone's father, someone's mother, and I don't think the public always appreciate that. And I think some of the media and, perhaps, horror films don't help at all because people see post-mortems as something that are gory and bloody, but that's not reality at all.

03:22 - Looking for external clues
Looking for external clues
with Dr Hugo Ford, Dr James Rudd, Dr Helen Simpson, Dr Prina Ruparelia and Dr Alison Cluroe, Addenbrookes Hospital
The first step in a post-mortem is to examine the patient for clues as to the cause of  death. What did the pathologist, Dr Alison Clureo find with Chris Smith?
death. What did the pathologist, Dr Alison Clureo find with Chris Smith?
Alison - This is a gentleman in his eighth decade of life; he had a history of ischaemic heart disease. So this means had hardening of the coronary arteries that supply his heart so he was at risk of having a heart attack. He had a history of a condition called chronic obstructive pulmonary disease which is where the lungs may have either bronchitis, or a condition called emphysema, which can be related to smoking. And, on the background of that, a condition called pulmonary hypertension where, because of the lung disease, the heart begins to fail trying to pump blood through these diseased lungs. He also had a history of type 2 diabetes, which was treated with medication rather than insulin injections.
Chris - Is there anything else, in terms of information that you're given, that might inform something you go looking for? Do you learn about the occupation of a person, or where they lived, where they came from, that kind of thing that might bias your terms of thinking like well, I should look for x, y, or z.?
Alison - Well, we also know that there's a possibility that this man may have been exposed to asbestos in the past. So, given that history in combination with lung disease, we would want to make sure this wasn't an industrial acquired lung disease related to inhalation of asbestos fibres.
Chris - So, having acquainted yourself with this gentleman - what happened to him in the past, his past medical history and also his occupational history - what do you do next?
Alison - So, my next procedure is to examine him externally in the first instance to see if there are any clues, and to make sure that I am about to autopsy the correct person.
Chris - Shall we do that?
Alison - Yes. On examination, he has several significant findings, In particular, he has a condition called clubbing of the fingernails and of the toenails. This condition is commonly seen in people with chronic lung diseases.
Chris - They do indeed look almost like the end of a drum stick, when you get to the end where the drumstick hits the surface of the drum it's sort of rounded curve shape. It's not the normal shape of a fingernail and all of his fingers look like that.
Alison - Yes. The whole nail curve rounds and you see this in the toes, to a lesser extent, but it's much more obvious in the fingernails. The other significant finding on external examination is that he has swelling of his lower legs, a condition that we describe medically as pitting oedema. So the lower legs, right up to the knees are swollen and I can actually indent the tissues because he has fluid in those tissues.
Chris - You've pressed, just gently, over the skin of his shin and you've left a finger impression there, which sits there for a while, rather like a footprint in sand, and then it slowly comes back out again, and that's because of fluid?
Alison - That's fluid retention in the tissues.
Chris - Anything else?
Alison - He has some areas of hemorrhagic bruising and some areas of skin tearing on his upper arms. I'm just wondering, although I don't have this information quite to hand, whether he had had some steroid treatment for his chronic airways disease. Steroid treatment, long term, can cause thinning of the skin and, in this instance, it's quite possible that the injuries that we're seeing are related to him having very fragile skin, subsequent to him having been on long term steroid therapy for lung disease.
Chris - Now with me in the studio to unpick some of these external clues are:
Dr James Rudd, he's a cardiologist at Addenbrooke's hospital and a Senior Lecturer at Cambridge University. Also Dr Helen Simpson, she's an Endocrinologist - someone who understands how the body's endocrine glands work. And Also, Dr Prina Ruparelia who's a Respiratory Consultan, also from Addenbrooke's.
Now Prina - Alison mentioned steroid treatment there. What is chronic obstructive airways disease?
Prina - It's really an umbrella term. It's generally related to smoking; the smoking causes inflammation in the airways which damages the alveoli, which are the air sacks, and it causes bronchitis, which is production of excess mucus. So the people that have this condition will often have a cough and they will have symptoms of breathlessness.
Chris - What about the hands? Because on of the other things we spotted was that his fingers have this characteristic clubbing. How common is that and why does that happen, do we know?
Prina - The actual mechanism is not really clear but it's often a sign of another condition in the body. So, when we're looking a lung conditions, it can be a sign of what we call a suppurative lung condition, which means a pus forming lung condition such as a lung abscess or cystic fibrosis.
Chris - And how common is this sort of presentation with chronic obstructive pulmonary disease? Is this a common phenomenon?
Prina - You wouldn't see clubbing in chronic obstructive pulmonary disease, so there must be something else that is causing that.
Chris - So we've still got something to look for. We know that COPD isn't the only thing going on in this gentlemen then based on what you've told us.
Helen - We know that the gentleman had type 2 diabetes. What is type 2 diabetes?
Helen - Type 2 diabetes is the most common cause of diabetes with about 90% of the people in the UK who have diabetes, having type 2 diabetes. And it's where the body gets insulin resistant or can't react so well to the insulin that the body makes, and is what we think of as being related to obesity and a more sedentary lifestyle.
Chris - This gentleman wasn't particularly overweight. Is that a common way for diabetes to present then, or do some people start a bit overweight and then become thinner?
Helen - So, when you're diagnosed with diabetes, one of the symptoms can be weight loss, so becoming very thirsty, passing a lot of urine, and losing weight. We don't know how long he'd had diabetes. If it was a new diagnosis he may have been losing weight or could have lost weight from another underlying pathology or condition. The other thing is he'd been taking steroid tablets and this can actually cause type 2 diabetes. It could be a drug cause and that may have been accounting for some of the sugar problems.
Chris - Ah right. So he could have a diabetic problem because of the steroids he was taking for his chest problem?
Helen - He could have, yes.
Chris - Why should it be bad to have high blood sugar? Why is that a problem?
Helen - It can cause some symptoms in itself. So it can make you feel thirsty, pass too much urine, you can lose some weight, and cause some problems with vision, the lens in the eye can get a little bit cloudy. But also it leads to long term complications and we split these into medical word, macrovascular - so big blood vessel complications and small blood vessel complications. People with type 2 diabetes are five times more likely to die of heart problems or vascular problems than the general population without diabetes.
Chris - James - Helen has mentioned that diabetic patients are at greater risk of damage to their blood vessels. What's the relevance here? This gentleman has a history of heart failure. Why might this be relevant and, also, what's the basis for the pitting oedema, the skin changes that Alison remarked on?
James - So diabetes, as you've said Chris, is associated with high levels of glucose in the bloodstream, and this can damage the inside of the arteries causing a process we call atherosclerosis. If the arteries to the heart have been narrowed by atherosclerosis, the pumping power of the heat is reduced, and this can mean the blood can build up in tissues of the body where it normally wouldn't accumulate so, for example, patients can get swelling of the legs.
Chris - The high pressure what, pushes fluid out of the blood vessels and into the tissue and that's why you get swelling and that's why, when we put our fingers on the skin, we could make those little indentations because we were literally pushing fluid out of the way?
James - That's exactly right. The condition is called heart failure. If the patient's heart failure is treated, then we often use the amount of peripheral oedema, the amount of swelling of the legs, as a sign that treatment is working. This will tend to get better over a few days or weeks.

Opening up the abdomen
with Dr Hugo Ford, Dr James Rudd, Dr Helen Simpson, Dr Prina Ruparelia and Dr Alison Cluroe, Addenbrooke's Hospital
Dr Alison Cluroe begins the post-mortem by opening the abdomen to study the stomach, pancreas and kidneys with Chris Smith...
Chris - When one looks at a text book and you see a person drawing, you can see this very organised loops of bowel, but this does not look organised. Just before we've even moved anything around, there seems to be stuff everywhere.
Alison - Yes, I think it's probably a bit like a personal fingerprint - no-one's is probably quite the same. But you're right, it doesn't look anything like the text books.
Chris - Do you preserve the contents of what's in the intestine?
Alison - Yes. So what you're seeing here now is the technician is actually tying off the base of the stomach where it goes into the first part of the small intestine, and that's to preserve the stomach contents should we need to analyse it. Sometimes we do in a case where we're suspicious that the person might have taken an overdose, for example.
Chris - What you have in front of you, Alison, is a little table that you've put over the gentleman's legs and, on top of that table, you're putting each of the things that we have removed from inside his body. And so now, this is the process where you're beginning to look at each of the organs in turn to step through them and see if there's anything in there.
Alison - That's right. So, with my scissors I'm cutting down the gullet and into the stomach. There's quite a lot of brown liquid in the stomach and this is just likely to be fluid that the deceased gentleman has had prior to death. And the striking thing is that you can see those sort of little black spotty areas over the lining of the stomach here...
Chris - Yes. The lining is sort of pale grey colour, and in some places it's not grey, it's like it'd got a rash - a very fine red rash. Why is that?
Alison - I think this gentleman has some gastric erosions. So these are very superficial damages to the lining of his stomach. That mucus there, when it breaks down, leads to stomach acids to be able to actually get to the lining of the stomach wall and cause ulceration and, hence, gastric ulcers. That's not uncommon in people who are very unwell.
We're going to move to some of the other abdominal organs now and the first one I've got here to look at is the pancreas. Now the pancreas lies just behind the stomach and it is an endocrine organ - that is an organ that produces hormones. It does two things actually, it produces insulin which, obviously, is useful in controlling our metabolism of sugars. And insulin is a substance that is in short supply in people with type 1 diabetes, where they're insulin dependent and need to have daily injections.
Chris - It's what - 15-20 cms long this one, isn't it? And it's got a sort of bulbous end, a fist sized end, and then a tail coming of that, that's a few cms across, and you've cut slices from one end to the other right across it. What are you looking for?
Alison - Pancreatitis. Inflammation of the pancreas can be seen in people with gallstones, people who are heavy drinkers but this pancreas looks quite normal.
Chris - Put that to one side...
Alison - We've got the two kidneys which are surrounded by a huge casing of fat. You can see, when I take this fat off you'll be surprised at how small the little kidneys are in size.
Chris - Is it normal for the kidneys to be encased in this much fat?
Alison - Yes. There always encased in fat and that's partly a protective process.
Chris - We can see going into the kidney is an artery - that's how the blood gets in off of the aorta. And the vein comes out and then anything that you don't want. You want to keep the blood obviously, the urine that goes down that eureta down towards the bladder. So you've got kidney out on one side, now you're doing the same thing on the other side...
Alison - They have an interesting external appearance. There is a small cyst; not uncommon to get small cysts in the kidney, they're quite harmless if there's just one or two. We have a mixture of surface appearances; we have a fine granularity to the surface. It should be very, very smooth but it isn't and then we have this much coarser indentations or scars on the surface, so we're seeing two slightly different things there.
The fine granularity is something you tend to see in people who have high blood pressure...
Chris - What about the scars that you mentioned? There's a very bit one - it looks like a crater on the moon actually. What's that?
Alison - So that is likely related to chronic infection and inflammation, and it's likely that this gentleman has had infection, probably arising from bladder infections.
Chris - It's left that legacy of the structural damage to the kidney but that's old, there's no evidence of that being an active infection?
Alison - No. The only thing we have is that we have some thinning cortex, that's the outer portion of the kidney tissue, and that thinning is a feature of the high blood pressure. The coarse scarring related to previous episodes of infection but we don't have anything else at the moment active that's going on in those kidneys.
Chris - So not a huge number of clues there, at least, not the acute cause of death yet. Now Alison did talk though, James, about high blood pressure. Why is that a problem?
James - So, in a similar way to diabetes, the presence of high pressure blood within the system can also damage the internal lining of the arteries. And, again, this can lead to hardening of the arteries of over many years, particularly if the high blood pressure is not treated.
Chris - Why does it cause that thinning of the outer surface of the kidney that Alison mentioned there, do we know?
James - It's due to, I think, to the same reason that we get with the heart, that the blood supply to the kidney itself is reduced chronically because the arteries supplying the kidney with blood are now down, and it's this long term reduction in adequate blood supply that leads to thinning of the cortex of the kidney.
Chris - If someone has high blood pressure, what symptoms would they have had?
James - This is one of the problems with having high blood pressure, very often it causes no symptoms at all and this the reason that GPs are very keen always to measure one's blood pressure when we go to the surgery. By the time it causes things like heart attacks and strokes and kidney problems, the high blood pressure may have been there for 20 or 30 years.
Chris - And what can someone do to control their blood pressure?
James - The best thing to do is to avoid things like smoking, to take regular exercise, try and eat a healthy diet. So, not so much red meat, plenty of fish, plenty of vegetables and fruit, and to get your blood pressure checked every year or so once you get to the age of 40. If lifestyle measures don't work, then the next step would be drug medications.
Chris - And Helen - we spotted that there was this damage to the surface of the kidney. Alison speculated that this could have been because, the gentleman being diabetic, was prone to infections and, possibly, kidney infections. Would you go along with that?
Helen - People with diabetes are prone to some types of infections and one particular site where people may get more infections in their feet, partly due to the damage to their nerves. People will injure their feet and not know, the blood supply can be reduced and so the cells that fight infection are slower to get there and also, if the sugar levels are high, it may be there's a better sort of culture medium for the bugs to grow in. So, certainly, we see increased levels of infections in feet and ulcers. As for the kidneys, I'm not sure we see a awful lot of extra kidney infections in people with diabetes but, I suppose you could speculate that, if the sugar levels were high and there was some injury there, there may be some focus for an infection to develop.
19:37 - Peering into the brain
Peering into the brain
with Dr Hugo Ford, Dr James Rudd, Dr Helen Simpson, Dr Prina Ruparelia and Dr Alison Cluroe, Addenbrookes Hospital
On the hunt to discover how the patient died, pathologist Alison Cluroe turns to  the brain, with Chris Smith...
the brain, with Chris Smith...
Alison - So I'm now going to look at the prostate gland, which is sort of the rubbery gland that sits just at the base of the bladder.
Chris - So the prostate, I can see that. That's about the size of a walnut and sitting around the tube, I presume that's the urethra? The tube comes out of the bladder so the urine can get out.
Alison - That's quite correct. The urethra tube passes straight through the middle of the prostate gland and that's where you have a problem if you've got an enlarged prostate and it gets swollen up, it actually nips off that urethra and so people have trouble passing urine.
Chris - We mentioned we'd seen evidence of past infection in the kidney. That would have come from the bladder so is the bladder normal to your eye though.
Alison - It is. I mean there's a tiny big of hemorrhage down here near the entrance to the prostate gland, but I actually think that's related to the fact that there was a catheter in place.
Now what I've done is I've separated off all the organ but I think, at this point, we might just let the technician take over for a moment and dissect back the scalp tissues so we can actually get the brain for a good examination as well...
Alison - So we've now taken the top of the skull bone off and you can see underneath the brain, which sort of looks like a bag of worms.
Chris - So the brain has come out in it's entirety in one go. You can see at the bottom where it would be connected down to the spinal cord and then up to the bit that would actually sit inside your head.
Alison - I am looking at the underside of the brain. We've got what we call the cerebellum, this is the little bit of the brain that deals with balance. You can see a cord of white tissue hanging over the top of that, that's the spinal cord and then the brain stem just above it.
Chris - The cerebellum's about the size of my fist, give or take, underneath the brain. Then the brainstem - that's what connects the spinal cord up into the main part of what I would like the call the brain proper.
Alison - Yes, that's right. And here you can see these two little structures here. These are the optic nerves. The...
Chris - There's a sort of poking out from the middle of the brain?
Alison - Yes. And we'll just separate those from where they run through the skull and into the backs of the eyes.
Chris - It's interesting because it's grey round the outside and white in the middle, so there is quite literally grey matter in your head?
Alison - Exactly. Grey matter is where the little grey cells and they are the neurons that fire off the impulses that allow us to do all the things we do, and the white matter sitting underneath that is the axon. And that axon, the reason it looks white is it's surrounded by a substance called myelin which protects it and allows the impulses to pass straight down the axon rather than them shooting off in different directions. So that's why you're seeing this two different contrasting areas of colour when we're slicing the brain here.
So, underneath the grey and the white matter, we have these spaces...
Chris - Right in the heart of the brain there are big holes, but they are quite normal?
Alison - Yes, absolutely. These are called ventricles and these contain cerebrospinal fluid, and cerebrospinal fluid it cushions the brain. It surrounds the brain and it's within the brain so the brain is sort of floating within a bath and that acts as a sort of a bit of protection for any sudden movements. It slows the movements down.
Chris - Like a shock absorber. Nothing abnormal coming up so far in here?
Alison - No. This brain actually looks very, very normal.
Chris - So we put the brain to one side.
Alison - The other organ that we haven't yet from the abdomen is the spleen. Now what I would say about the spleen is it's very soft and I think that the reason for that is that there is evidence of infection. Sometimes you can find at autopsy that there is a softening or a sort of liquefaction, a liquefying of the tissue of the spleen and I think that we have got a clue here to one of the reasons why this gentleman has died.
Chris - Which organ shall be look at next?
Alison - So I'm just going to open the gall bladder and drain away the bile...
Chris - The liver makes bile, doesn't it?
Alison - The liver makes bile. That's the bile, yes. Nothing to worry about in the gall bladder but something of considerable concern in this gentleman's liver. What we can see here are white bumps all over it (2-3 cms in areas), and these are tumour deposits that have extensively spread to involve the liver.
Chris - It's literally covered. If we look at how much of the liver is what should be normal healthy liver tissue and how much is the cancer, I'd say that maybe half of this person's liver is now taken up by these big blobs of tumour.
Alison - Yes, I would say you're right. About 50% has been replaced by tumour. We can see the background liver. This is the brown tissue between the white nodules, and the background liver is also abnormal, in fact. It's got a very congested pattern that we would call a nutmeg pattern, and nutmeg liver is seen when someone has a condition of congenital heart failure. Where the right side of the heart is failing, causes this back pressure on the veins, and that back pressure causes congestion within the organs that need to drain into the right side of the heart. So what you're seeing here when you see this nutmeg appearance is you're seeing normal bits of brown liver and then much darker areas of very congested liver and congested blood vessels.
Chris - These tumours then. The fact that the liver is full of them and they range in size, there are some small ones and some big ones. Does that they didn't come originally from the liver, they've probably come into the liver from somewhere else in the body?
Alison - I think it's more likely that these are what we'd call metastasis. That means they've spread from somewhere else. The liver is not the primary site of the tumour. I mean, obviously now, we've certainly got a malignant process in this gentleman which is likely to have contributed to his death.
Chris - Also with us is Dr Hugo Ford who's a consultant oncologist, or cancer specialist at Addenbrooke's Hospital. When someone actually get's a cancer, why have they got cancer? What has happened to their cells to make them behave in this abnormal way?
Hugo - Well, most commonly, there's some form of damage to the DNA in the cells. And this can come from an external source or it can come from the normal process of cell division and a mutation, which is an error in a replication when your cells are dividing.
Chris - Like a genetic spelling mistake?
Hugo - Like a genetic spelling mistake, and these tend to accumulate. And all of our cells DNA has, on the end of it, something called a telomere and every time you copy that DNA, a little bit of the telomere get's cut off. They only have a certain number of cell divisions before your reach the end of the telomere and that triggers the cell to die.
In cancer cells, they manage to immortalise themselves by lengthening those telomeres. So the telomere, effectively, doesn't shorten and, therefore, there is not trigger that tells your body that this is a cell that's reached the end of it's life and it needs to die.
Chris - So it carries on growing?
Hugo - So they are immortal and that is one of the key characteristics of many cancer cells.
Chris - Is the liver a common site for cancers to spread to?
Hugo - Yes, it's one of the most common sites for cancer to spread to, in fact.
Chris - Why?
Hugo - The general way by which cancer cells spread is through the bloodstream and that's certainly one of the most common ways, and they do tend to lodge in places where there are filters for the bloodstream. So we commonly see the liver, which is a major site of filtration for the blood. The lungs also, there's a high volume of blood flows through the lungs, and often the bones as well.
Chris - And is it just physically the spread to somewhere else in the body and the growth in another place in the body that makes cancer bad, or can it do other things to you biochemically, and so on?
Hugo - Cancers can cause problems by invading into various tissues that cause damage. But they can make hormones which can cause endocrine problems, for example, or they can produce antibodies which causes inflammation or damage to particular parts of the body. So there are a number of ways in which cancers can damage the body other than the direct invasion.
Chris - If you pick up a cancer that's already spread, what can one do then to work out what the prognosis is for that person?
Hugo - Well the important thing is to find out exactly what one's dealing with. So a biopsy is usually very helpful, and that's taking a sample of tissue from the cancer, looking at it under the microscope, and trying to identify what it's characteristics are. Now that may help you as to where it's come from, but it may also help guide you to the prognosis of the cancer, and the tumour, and how you might wish to treat it.
28:26 - The cutting edge: dissecting the heart
The cutting edge: dissecting the heart
with Dr Hugo Ford, Dr James Rudd, Dr Helen Simpson, Dr Prina Ruparelia and Dr Alison Cluroe, Addenbrookes Hospital
Surprising results ensure when dissecting the patient's heart as Chris Smith found 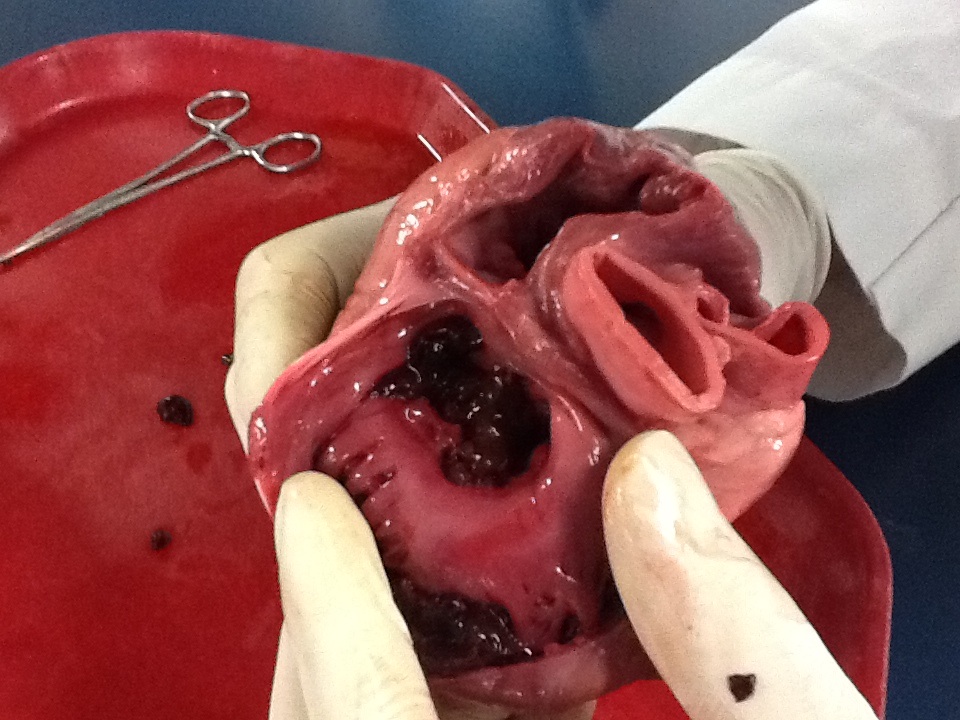 out with Dr Alison Cluroe...
out with Dr Alison Cluroe...
Alison - To take off the front of the ribcage and the breastbone we're going to need to use some shears... OK, so this is the inside aspect of this gentleman's breastbone, looking at it from behind as if we were standing inside his chest looking out, and what we can see here are these nodules on the surface.
Chris - So just to describe these a little bit. There are some little bumps; they're between a few millimetres and maybe up to a centimetre across; they're white and there are lots of them. It's almost like a rash, like a chickenpox rash but on the inside. What is that?
Alison - That's a tumour of some form. I'm not sure what tumour yet, I'd need to look at it down a microscope.
Chris - Do you think that the history of asbestos might be relevant?
Alison - It's possible, but this could also be a metastatic tumour from another malignant process. It doesn't have to be asbestos related.
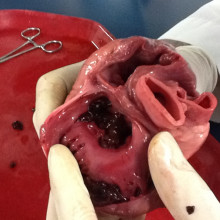
Chris - Right. So, this is the heart?
Alison - This is the heart...
Chris - And it's very big...
Alison - It's a huge heart. Much bigger then if you were to buy a heart from the butchers shop. You often buy a beef heart or an ox heart. The heart is made up of four chambers; two ventricles - the big pumps, and two atrias - the sort of smaller pumps really. Now all the chambers of this heart dilated so this is a very big heart. It actually weighs 610 grams...
Chris - A normal would be half that, wouldn't it?
Alison - 300-350 for this sort of sized person. So I'm going to open up the heart now and we're going to have a look into chambers, particularly looking at the valves that help with the blood flow through the heart...
I've taken these cross-sections through the heart, like slicing an orange and looking at the segments. The most striking thing is the actual chambers of the heart are very large.
Chris - Why does that happen?
Alison - Because the arteries that supply the muscle of his heart may be narrowed and those blood vessels are just not able to supply as much blood as we would like to see. The other striking thing, that perhaps I should mention, is that although the ventricular chambers and the atrial chambers are quite dilated. The heart muscle is quite thickened and it's very, very marked on the right side here. That is at least a centimetre in thickness that right side, and that's much too thick for the right side.
Chris - Two or three times bigger than it should be, isn't it?
Alison - Two or three times bigger than it should be and likewise on the left even here, we're almost up to 2 cm in places. Now this is a big meaty heart and it's failed so it's become baggy and you can imagine that's not going to work as an effective pump to force blood around the body.
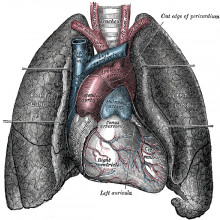
So what I've got left now having removed the heart are the neck structures and the arche of the aorta. Now the aorta, if you remember, is the great big artery that feeds blood around the body.
Chris - This is the big blood vessel, it comes off the top of the heart, it curves and does almost 180 degrees like a U turn, to then go down the body. That's what we've just opened up and the first bit of it looked OK, but this bit doesn't look so good.
Alison - And we've got these great big yellow hard plaques which have got calcium in them. So this confirms the fact that this gentleman does have quite significant atheroma (hardening of the arteries), and you can perhaps hear the calcium there...
Chris - There is, quite literally, a stone in the wall of the artery, and that's classic for someone having hardened arteries?
Alison - Exactly.
Chris - James - it really was striking how hard those arteries were. Why should arterial disease end up with calcium like that?
James - One of the ways that the body tries to heal this longstanding inflammation is by actually laying down calcium, exactly the same as would happen in a bone after a bone fracture.
Chris - So why should this healing process actually be bad news.
James - Most of the time the calcification of the arteries is a good thing. The body does succeed in stopping the inflammation happening within the arteries. Sometimes, unfortunately, it doesn't and the calcification itself can lead to problems such as heart attack and stroke. So the plaque within the artery ruptures, and that fatty gruel that's built up within the artery wall over many years is suddenly exposed to the blood flowing right past it and this can trigger immediate formation of a blood clot within the artery. And if this happens in an important artery like an artery supplying the brain with blood or the heart muscle with blood, then you get downstream reduction of blood flow to that organ and you get a heart attack or a stroke as a result.
Chris - James - the other thing we found was what Alison described as "a very baggy heart." It was extremely large. Why does it look like that and how does this relate to that diagnosis of heart failure?
James - This is because there's long term high blood pressure which has caused thickening of the heart muscle, as you would if you worked in the gym on your biceps. The muscle mass of the biceps would tend to increase and this has happened in this patient. But the other thing in this gentleman is that, as I said, the arteries are hardened so the blood supply to the heart muscle is reduced, and has probably been reduced over many years. And this causes the heart to experience what we call heart failure whereby the chambers of the heart actually get larger and, unfortunately, the pumping power of the heart, even though it's more musclebound, actually get lower, and lower, and lower as time goes by.
Chris - So despite being a bigger heart, initially that would have probably helped to overcome the fact that this guy had high blood pressure. Eventually, the chronic deprivation of oxygen and blood flow to the heart, and ongoing problems like hard arteries, means the heart just can't cope and it begins to become bigger.
James - Exactly. So initially the compensation that you've described, the heart becoming more musclebound, would certainly have worked for this gentleman but, unfortunately, the heart can start to fail and this is where we see the heart becoming extremely large.
Chris - And Prina - when we looked at the breastbone, there were lots of little tumours that we highlighted. We said possibly related to asbestos. Before we speculate what the lumps are, how does asbestos cause lung disease?
Prina - Asbestos was commonly used in building about 40 years ago. We don't use it so much now, it's banned...
Chris - It's a mineral, isn't it?
Prina - Yes.
Chris - You dig it up out of the ground.
Prina - Exactly. So it's a mineral with silica. It's just a very heat resistant, durable, and quite useful material because you can mix it with other things.
Chris - So does concrete and that doesn't give us cancer, so what's the difference the distinction?
Prina - It can become a dust which, once its inhaled, can migrate into the lungs and you can't break it down. So it just sits there and it can participate inflammation in the lungs.
Chris - So it's the fact that it's very small, gets very far into the lung that then doesn't get out again, that you get cycles of inflammatory damage?
Prina - Exactly. The body recognises it as a foreign body but can't break it down and so then that can drive mutations and form tumours.
Chris - And someone who has had a lifetime exposure of asbestos and might be developing one of these asbestos-linked diseases, what short of symptoms would they have?
Prina - There's a long lag time from asbestos exposure to developing an asbestos related condition.
Chris - How long?
Prina - For the cancers it's in the range of 20 years. For the fibrotic conditions it may longer, 40 years after the exposure. But symptoms may include breathlessness, chest pain, a cough. It can be quite vague symptoms and people may not realise for quite a long time before they present for medical attention.
37:14 - The lungs go under the knife
The lungs go under the knife
with Dr Hugo Ford, Dr James Rudd, Dr Helen Simpson, Dr Prina Ruparelia and Dr Alison Cluroe, Addenbrookes Hospital
Next, pathologist Dr Alison Cluroe dissected the lungs to see whether this might  hold the key to the cause of death with Chris Smith...
hold the key to the cause of death with Chris Smith...
Alison - So what I have here is the thoracic organs and what you're seeing me do at the moment is I'm just opening up his gullet to make sure there is no food in there. And then I'm just opening up his voice box, the larynx, and then beyond the voice box we're going into the windpipe or trachea, and then it splits, it divides into two. One going to one lung and one going to the other - these are the bronchi and, in fact, in this gentleman's right main bronchus we have pus.
Chris - The fact that you can see pus there, that's immediately telling us that there's something wrong with this person's lungs?
Alison - Absolutely. The other thing I can see are more of these white nodules that we discussed on the lining of the ribcage, and you can see more of them on the surface of the lung here.
Chris - This persons lungs are about football sized, aren't they? If you were to put the whole block of tissue together, it's about the size of a football. Are they very heavy?
Alison - They are unnaturally heavy. Sometimes lungs fill up with fluid because the heart isn't working to pump fluid away from the lungs and it's like a very wet sponge, soaked up with water and, if you look now as I just press the lung tissue, there's lots, and lots, and lots of fluid.
Chris - It's frothy.
Alison - It's frothy, it's pouring out of the lung tissue.
Chris - And if that lung was full of fluid instead of being full of air, it would have meant the lung didn't work as well as it should do. He would have been short of breath.
Alison - Absolutely. So he's going to be having trouble breathing and that's all a consequence of his heart failure.
Chris - Anything jumping out at you at this stage that you can see?
Alison - Not a great deal at the moment. There does appear to be a suggestion of some infection which, actually, looking at it now closely, having touched it, I wondered if it was infection, but now I can see that it's a plaque. It's a white plaque of tissue. That is very typical of the sort of plaque one might see in asbestos exposure.
So I'm just going to move on to the vessels of the lungs and cut down there...
Chris - These are the arteries and the veins that bring blood to and from the lungs. Why are you interested in the vessels?
Alison - Well, I'm particularly looking for evidence of pulmonary embolism, that is blood clots to the lungs, particularly because of two reasons. This gentleman has evidence of swelling of his lower legs and that increases the predisposition to blood clots developing in the veins inside the calf muscles of the legs. But also he has a disseminated malignant process which also makes the blood more sticky and, therefore, increases the risk of you developing blood clots, and I can't see any evidence of that.
Now I'm going to slice these lungs because I can feel some large lumps inside the lung tissue...
Chris - In both of them?
Alison - In both of them... As I open it up, you can see at the very top part of the left lung,there's this great big cream and pink mass - it's about the size of an apple, and this is a tumour.
Chris - The rest of the lung tissue is pinky brown. There's some blackness which I presume is carbon, which is in there from when perhaps this person's been a smoker, but there is this very well defined, big, round, apple sized blob.
Alison - Now what I'm most interested in is this... now cutting the other side.. Is another lump of tumour, which I had actually thought was within the lung, I'm now thinking it might be a lymph node that's got tumour in it.
Chris - Lymph node being - these are our glands. They drain fluid away from different tissues. So if cancer breaks away from one place in the body, one of the places it can go is into these glands.
Alison - That's right. Now we also have a bit of pus, so we have got a little bit of what I think would be bronchial pneumonia developing here. Not surprisingly, because we've got this great big tumour and I think, given that location, it's likely to be a lung adenocarcinoma and I think, although they can sometimes they can be associated with exposure to asbestos, there also not uncommon in people who have a history of smoking.
Chris - Dr Alison Cluroe. So a number of pathologies there. We've got these frothy lungs, we have an apple sized cancerous tumour, and also a lot of black carbon was visible in the lungs. So let's start there...
Prina - how do you end up with black lungs if you smoke?
Prina - Cigarette smoke has lots of different chemicals in it. There's over 700 different chemicals in cigarette smoking including tar so, if you chronically smoke, you will deposition of those chemicals.
Chris - Don't the lungs clean themselves out?
Prina - They do, but smoking in itself can damage the cilia, which are these little hair-like structures in the airways which gives a mechanisms to clear things from your lungs. If you smoke it damages those cilia and so you can't clear it.
Chris - So it's a bit like the cleaners all going on strike and no-one to empty the rubbish bins so stuff just accumulates, and the accumulation of the stuff then accelerates other sorts diseases and disease risk, I suppose, things like cancers?
Prina - Yes, exactly, cancers. And equally this gentleman has COPD, and that has also been shown to cause damage to the cilia and inflammation within the lungs which may also have predisposed him to tumour development.
Chris - And Hugo - the spread from this, what we presume to be the primary cancer in the lung around the body, both to the glands tissue and to the liver, does that fit?
Hugo - That would be an absolute classic characteristic of the way that lung cancer would affect the body, spreading through the lymphatic system (the lymph glands) and through the bloodstream to those other areas.
Chris - And he didn't have a known history of lung cancer when we reviewed his notes. Is this a pretty common thing to just discover like this?
Hugo - Well it is certainly common that lung cancer is advanced at the time that it's diagnosed.
Chris - Why?
Hugo - Well there's a combination of features. The first thing is, of course, that the symptoms can be quite non-specific, so most of us would get a cough and wouldn't think too much of it. Often the tumour has to be quite large before it would give you the more serious symptoms that one would get. For example pain, coughing up blood which is a very important symptom. For a tumour to actually cause you to cough up blood, often they're quite large cancers and, by that time, it's much more difficult to treat them.
On the other hand, for the amount of disease that this man has, I would be surprised if he wasn't having some symptoms from it, and I think it would be interesting to know whether for the few months before his death he actually did have symptoms which, in retrospect, would have been attributable to his lung cancer.
Prina - Alison - used the word bronchopneumonia. She said there was some pus coming out of the airways and this gentleman had clearly had some signs of infection, what is bronchopneumonia?
Prina - So, pneumonia is an infection within the lungs. It is usually due to either a bacteria or a virus on occasion. We breathe these things in all the time, the lungs can usually clear them but, in some cases, that can cause an overwhelming infection and then, in a bid to try and fight that infection, there'll be a lot of inflammatory cells coming into the lungs and so that causes a buildup of pus. And bronchopneumonia is an infection within the main airways.
Chris - Would the cancer this gentleman had have made it more likely for him to develop that condition?
Prina - Yes, for a number of reasons. As he's got cancer his immune system may have been suppressed. Equally it's possible that there may have been a tumour deposit that was affecting the clearance mechanism of the lung. And equally we already heard that he'd probably had steroid treatment as well. So all these three factors could have contributed.
Chris - Because steroids reduce your immune response, don't they, so that would increase his risk of succumbing to an infection?
Prina - Yes, exactly.
Chris - What about the fluid? These lung, I picked them up and they're very, very heavy. Twice, three times the weight they should have been. Where was all that fluid coming from?
Prina - Because of his heart failure you will get a back pressure in the blood vessels in the lungs and they will become leaky. Just as his legs were swollen you would get fluid leaking into the lungs for that same reason. Equally because he's got infection, that may have made his blood vessels a bit more leaky as well.
Chris - And Hugo - one of the things we didn't find here, but Alison specifically went looking for, was a pulmonary embolus, a blood clot that lodges in one of the main blood vessels supplying the lung. And she made the point that people with cancer are more likely to suffer from what she dubbed sticky blood. What's the background and basis of that?
Hugo - So there are a number of reasons why people with cancer are more likely to have blood clots. And those range from a local effect from actually a cancer in the pelvis which is pressing on a blood vessel reducing the flow, and that means when the flow in the blood vessel is less, and slower, it's more likely to sludge up and clot. To the fact that people with cancer often don't eat and drink very well and can get very dehydrated and that's another thing, which again, makes their blood more likely to sludge up. And finally, actually some of the treatments that we use for the cancer themselves can make the blood more sticky, more likely to clot.
So there are a number of reasons we do see, not infrequently in people with cancer, blood clots either in the veins lower down in the body or in the lungs.

47:06 - What was the cause of death?
What was the cause of death?
with Dr Hugo Ford, Dr James Rudd, Dr Helen Simpson, Dr Prina Ruparelia and Dr Alison Cluroe, Addenbrookes Hospital
The patient had a whole host of pathologies but what was the cause of death? Dr Alison Cluroe explained her decision to Chris Smith...
Alison Cluroe explained her decision to Chris Smith...
Alison - I think at the end of the day the cause of this man's death is a combination of different pathologies, and then teasing out how we prioritise those to get a proper and accurate cause of death on the death certificate is the issue that we're now faced with. And in my view, looking a the degree of fluid in this gentleman's lungs and the presence of the superimposed infection in his lungs, those are going to be his primary cause of death. I think, in fact, he has died as a consequence of bronchopneumonia secondary to heart failure as a consequence of ischaemic and hypertensive heart disease. However, he is also a very unwell gentleman because we know in the background of all of that he's got lung cancer which appears to have spread to his liver.
So, I will give the cause of death as bronchopneumonia, arising on a background of ischemic and hypertensive heart disease. And under number 2 on the death certificate, we will put down disseminated lung cancer and also diabetes.
Chris - So James - now you know the verdict, what do you think.
James - Well, I think I'm not surprised by the verdict. We've been building up, I think, to this sequence of events, the diagnosis, for some time. So this would explain the patient's dying had a number of serious illnesses, some of which had relatively recent onset like pneumonia, but some of which, I think, have been present form a long time such as the heart disease.
Chris - Hugo.
Hugo - Well, I would agree with that. What I think is interesting about this gentleman is actually how many different things he had wrong with him which, apparently, nobody knew about. And I think that does ask the question about how often we actually do ask our doctors about the symptoms that we have.
Chris - When I was at medical school, on the front of one of the handouts, very memorably it said "a healthy patient is one who has been inadequately screened." It's absolutely true here I think, isn't it James?
James - No it is, you're right. I don't know if this patient lived alone. That might have been an important factor whether he had nobody to complain of any symptoms to. But yes, he seemed to have multiple things wrong with him which, unfortunately, culminated in his dying.
Chris - Now everyone sitting here has the benefit of all of the technologies that hospitals can bring to bear to solve a problem - blood tests, scans - we've talked about many of them. If you're a general practitioner though, which is the individual to whom most cases will present in the first instance because that's who they have a relationship with. They can't get to see one of you guys until they've actually been to see a GP. They don't have access to these sorts of things Helen.
Helen - No, I think it must be incredibly difficult. GPs are great, they have to deal with everybody who walks in through the door and some of these symptoms, as Prina said, can be non-specific. If someone's breathlessness with known lung disease, you may not think it can be anything else if that's the only symptom, so I think they have a very difficult job unpicking everything. We can call a colleague up very easily on the telephone within the hospital and, as you say, we have access to blood tests and scans. GPs have to refer, there may be delays, so I think primary care has a very difficult job in teasing out all the different things that patients can present with.
Chris - Prina - you're the respiratory person and it did turn out to have a very important bearing on what happened here because, ultimately, we think that's why this person died, but there was a lot more to it than just having a chest infection in this instance.
Prina - I think he clearly had many different medical problems and going through the post-mortem, much of what we saw in the first external examination is explained. The clubbing is certainly explained by his lung cancer.
Chris - Well it was you at the beginning who said "well I think something else is going on because we can explain, on the basis of the history, why he got that."
Prina - Yes, so that certainly had a bearing but I think also you could see from his heart failure and his COPD that he had many reasons to be breathless. So that might explain why he didn't perhaps present with his lung cancer as well because many of the symptoms he had may have overlapped with his other conditions.

51:28 - How post-mortems save lives
How post-mortems save lives
with Dr Suzy Lishman, President of the UK’s Royal College of Pathologists
It sounds counter-intuitive but conducting post-mortems can help save the lives of the living as Suzy Lishman explained to Chris Smith...
the living as Suzy Lishman explained to Chris Smith...
Suzy - I don't think we can underestimate just how valuable post-mortems are. And I think people often believe because we now have very sophisticated scanning equipment and we can do lots of tests before people die, that we can't find anything about them or about their disease after death, and repeated research has shown that that's just not true. We know that around a quarter of post-mortems find really significant findings that may have made a difference to the way in which that person would have been treated had they been known about before their death.
Chris - How many people are having post-mortems now?
Suzy - Around 200,000 people a year have a post-mortem at the request of the coroner, and we know that the vast majority of post mortems done in this country are coroners post-mortems. Only a very small number are done at the request of the doctors or the family. So the numbers have been falling, particularly these consented post-mortems have been falling for some time. And there's a real problem with that because the coroner's job is just to find out why somebody died as well as who they were, where they died, and just some basic facts like that. Whereas, a consented hospital post-mortem can really do into much more detail and give the family much more information about what happened to their loved one, and the effects of any treatments they might have had, and whether there are any implications for the surviving family.
Chris - And why have numbers fallen?
Suzy - I think it's a combination of things. I think partly people don't think it's necessary any more because people have had scans and they think they've got a definite diagnosis before death. So they don't think there's any point, and nothing else will be gained, and I don't think that's true. I do think there's an aversion to having post-mortems because of misconceptions that they're not respectful and dignified procedures, and that people feel, when somebody's died, that they don't want to put them through anything else. And also, I think, hospitals are coming under increasing pressure to do more and more work with fewer and fewer people and so there are not enough pathologists, with enough time to dedicate to doing more and more of these post-mortems. So they're one of the first things to go when the pressure goes up.
Chris - When you say there are not enough people doing this, what's the evidence of that? Have we actually got a drop in the number of trainees going into pathology as a specialism?
Suzy - The numbers of people training in pathology have stayed relatively constant, although we believe that we need more people than we currently have allocation for. Pathologists now now longer have to do post-mortems as part of their qualifying final exam and that was introduced because we knew that, in a lot of departments, pathologists never did a post mortem again after they became consultants and after they qualified, and so there was no real need for them to learn those techniques if they weren't going to use them again. So we know that a percentage of trainees are no longer training to do those post-mortems but, actually, that's not really why the number of people available to do them is falling. It's really because of other pressures on people who are perfectly capable and trained to do post-mortems, who just don't have time to do it. Perhaps their hospitals have said that it's not a priority for them and they're so busy making diagnoses for the living, and there are so many targets, for example, to diagnose cancers quickly, that post mortems have really lost out and aren't being valued for the benefits that they can provide.
Chris - And what's going to be the impact of that downstream?
Suzy - I think there's a real worry that the post mortem service, and by that I include the coronial service because it's the same doctors providing both types of post-mortem, that it will collapse in some areas. That if you haven't got enough people that are able or willing to do post-mortems, then the service can't be provided and, of course, that's bad news for relatives because they're not getting the answers they need, and they're not perhaps getting them as quickly as they ought to.










Comments
Add a comment