Keeping Organs Alive
Interview with
Helen - As
Megan Sykes was explaining, their system is currently only suitable for live transplant donors because patients have to be prepared for 5-6 days in advance before transplant for technique to work. So most donor organs wouldn't survive long enough.
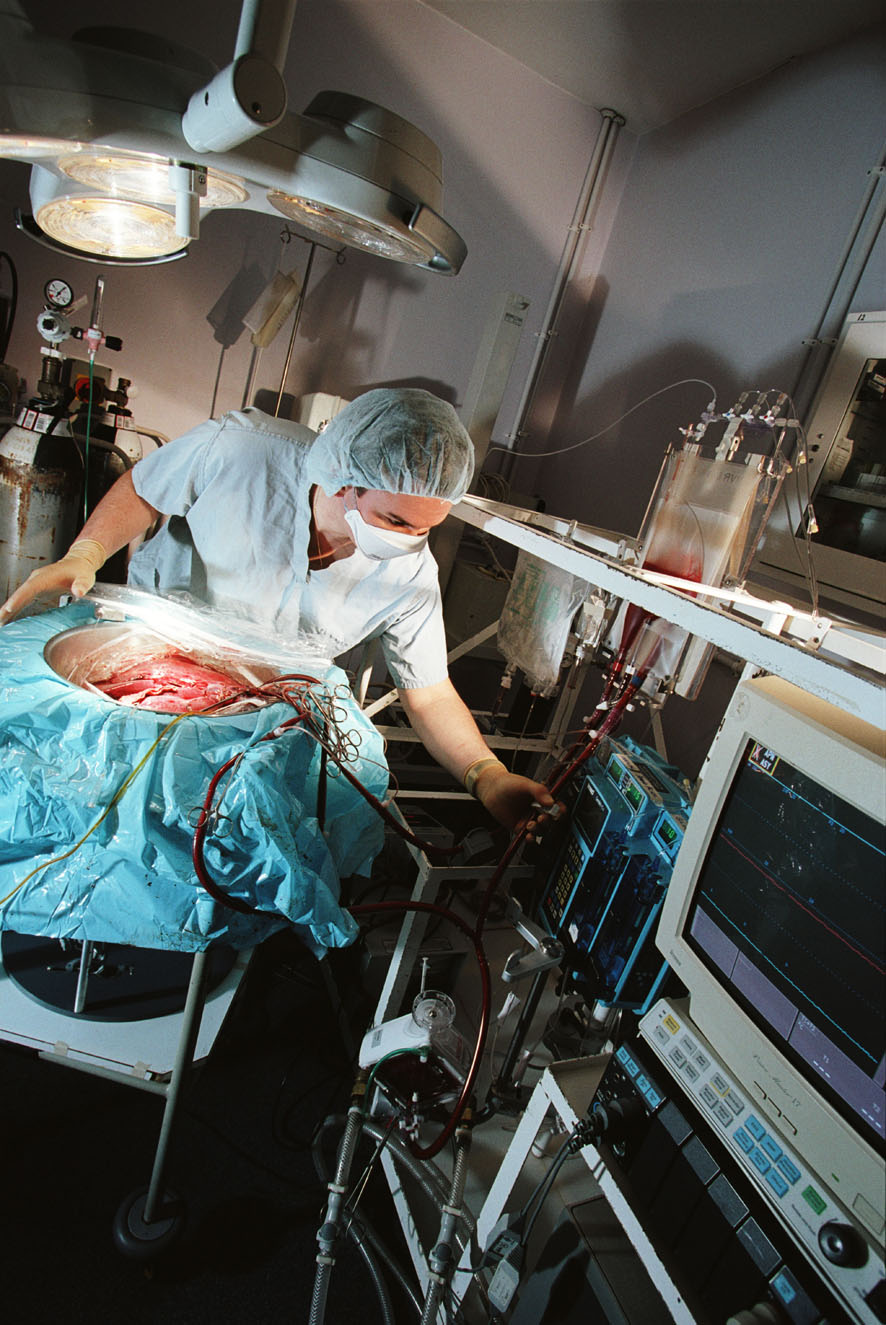
But that could be about to change because two Oxford Scientists, Dr Constantin Coussios and Professor Peter Friend, have developed a way to keep organs in pristine condition outside the body. I wonder if perhaps we could start by outlining what is it that goes wrong with organs in transit. How can they get damaged?
 Peter - The problem is that we remove organs, we deprive them of oxygen, blood supply and to restrict the amount of damage that occurs we cool them down. We all know that when we put biological tissue, meat, into a refrigerator it lasts longer but it doesn't last forever but the cells continue to metabolise. They continue to function but at a much, much lower rate: about 10 times slower. There is still a limit to how long you can maintain a cell alive under those circumstances. At the moment for transplants, for kidneys, you can store a kidney for up to 24 hours but we do know the longer you store it the more problems there are likely to be thereafter.
Peter - The problem is that we remove organs, we deprive them of oxygen, blood supply and to restrict the amount of damage that occurs we cool them down. We all know that when we put biological tissue, meat, into a refrigerator it lasts longer but it doesn't last forever but the cells continue to metabolise. They continue to function but at a much, much lower rate: about 10 times slower. There is still a limit to how long you can maintain a cell alive under those circumstances. At the moment for transplants, for kidneys, you can store a kidney for up to 24 hours but we do know the longer you store it the more problems there are likely to be thereafter.
Helen - So, the longer you store it is it just more likely that it won't take when you transplant it?
Peter - Well it's got an increased risk of not working at all but if it does work it's likely to work less well and for a shorter time.
Helen - So at the moment the technology is just 'put the organs on ice.' Is that as simple as it is, really?
Peter - Well, the technology's essentially profusing the organ with a specialised solution which is designed to protect the cells from swelling and putting on ice to reduce the metabolic rate. That's, as you say is rather a simple concept and one that has worked quite well for a number of decades but it has severe limitations.
Helen - So, Constantin, perhaps I'll bring in you here as well. How are you addressing this problem, what are the technological changes that you've come up with to address this issue of organs surviving alive, if you like, outside the human body?
Constantin - We've long held this belief that cold is good but warm is better. In fact, organs are designed to be stored and operate at normal body temperature. We wanted to come up with a way to store an organ in such a way that it would never know it had left the human body. What we started working on was developing the technology that would allow us to maintain an organ at body temperature whilst profusing it with cold blood: feeding it such that it was undergoing the same function as it would be within the body.
Helen - So you've almost tried to trick it into thinking it hasn't left the body at all.
Constantin - Precisely. The major assumption in cold preservation as Peter just mentioned a moment ago you have damage in proportion to storage time whilst if you're able to maintain an organ in normal, active synthetic state what will happen is there'll be no such damage in proportion to storage time.
Helen - Ok so keeping the organs in a system that's tricking it into thinking it's still in a body. That's all sounds quite straight-forward. It isn't, is it?
Constantin - People have been trying to do it for over a hundred years and one of the major challenges which is particularly true for the liver, which is the main organ that we've been focussing on so far, is that it dramatically changes its vascular resistance to flow. Depending on how much we're eating or sleeping or drinking the amount of flow through the liver will allow through itself will change dramatically. The major innovation and the reason we believe what we're doing works much better than previous attempts is that it allows the organ to auto-regulate its blood supply. It's effectively a system designed around the organ which under no circumstances forces blood through the organ. What we end up with is very exciting. It is in fact a liver which manufactures bile outside the human body, just the way it would inside the human body itself.
Dave - So are you basically just pumping a constant pressure rather than just pushing a certain amount of blood through every second?
Peter - The object is to maintain completely normal physical parameters in terms of both flows and pressures. The liver, in particular is complex. It has a dual blood supply: one vein a high flow, low pressure and one artery with high pressure and lower flow - very complex. What actually happens inside the liver is relatively poorly understood in those terms. What we've done is to generate a system which places the liver in a completely physiological environment.
Dave - What is it which is limiting the life of the livers which you're using at the moment?
Peter - We haven't tested the hypothesis, as it were, to destruction so we don't know. We know that livers will survive and function apparently normal for periods of up to three days. We haven't done the ultimate experiment we'd like to see how long they will go but there are some complex biomedical engineering challenges in terms of, for example, damage to red cells in an artificial circuit which will become limiting at some point.
Constantin - The major limiting factor, if I may add, is the lack of sleep for the investigators concerned because at seventy-two hours the given team of a given size, eventually someone has to go to bed. We very much hope that with the advances of automation and integration that we're getting into we'll be able to test it to destruction.
Dave - If you can keep the liver for long periods of time does this mean you can match donor livers to recipients much better because you don't have to have them both ready at the same time?
Peter - Well, there are two huge potential advantages. One of which is that we can start to take organs that were previously discarded, organs that were damaged or organs that are causing concern as to whether they're going to work and we have good evidence now that we can actually resuscitate and improve the performance of an organ before it's transplanted. We can also measure how well it works before it's transplanted so there's no risk, as it were, to the patient receiving the organ. It's already been tested so that's a very large advantage. The other advantage which you were alluding to was if you could keep the organ for long enough you could start to do some very complex interventions into the matching between the donor and the recipient. You were hearing from professor Sykes a few moments ago about one very interesting intervention which is a bone marrow transplant. But, that requires time before the transplant takes place. This sort of technology starts to open up strategies of this sort, not just the one we've heard about but others which would improve the immunological outcome following transplant.
Helen - You're focussing at the moment on the liver and presumably would this kind of technology be applicable to other organs? Are there other organs that are even more of a challenge to keep alive outside the human body?
Constantin - Indeed. The principle as I said, the governing principle which has made this invention work is blood regulation. The principles behind it are certainly applicable to all organs that do not act as their own pump so all organs excluding the heart. In particular, the liver, the kidney, the pancreas, the small bowel and potentially the lungs in isolation are all potential candidates for use with this technology. The fundamental difference and the thing that makes this exciting is that in a cold preservation context you do not have a functioning organ during the period of preservation. In this paradigm you've actually got a fully functioning organ that can be quantitatively assessed prior to transplantation. That's really quite exciting.
Helen - So Peter, how close are we to seeing this actually happening in a hospital in emergency rooms: this technology might be applied?
Peter - There's been a lot of work on this working on an animal model. We're confident that the system works. We've gone all the way through with transplants. It's clearly an advance. We're currently in the process of developing prototypes which can be used in patients and clearly that's something which has to be developed but we are looking to carrying out limited clinical trials within the next year or two. It's not very far away.
- Previous Avoiding Organ Rejection
- Next Building a New Heart










Comments
Add a comment