Zika immunity and falling body temperatures
Have these paralysed patients helped to reveal the brain basis of why we gesticulate when we talk? Also, new insights into how the body clock keeps track of the seasons, signs that immunity to Zika virus wanes with time, why human body temperature is lower than it was 150 years ago, and diversity in science: how can we better hold on to rare talent?
In this episode
00:30 - Reading the brain to decode speech
Reading the brain to decode speech
Sergey Stavisky, Stanford
We all do it. Whether it’s pumping the air as we yell “YEEESSS” when a favourite team scores a goal, or waving our hands expressively in front of us as we talk politics with a friend, gesticulating appears to be part and parcel of how humans talk. But what underlies this? Well perhaps a new discovery sheds some light on the question. As he explains to Chris Smith, working with patients paralysed by spinal injuries, Sergey Stavisky has been looking at recordings from the part of the brain’s motor cortex that normally moves the hand. When his subjects spoke, neurones in this area fired up too. But why?
Sergey - The opportunity that we had is we were recording in people with paralysis as part of a clinical trial and we're recording from an area where previously speech was not thought to be located, but no one had actually directly tested for this. And so this gave us this great chance to go and look. So we have electrodes that are placed in the so-called hand-knob area of motor cortex and specifically it's in an area that's well implicated in generating our movements. Traditionally, our group and many others have been decoding hand and arm movements, and because there's a need for people who can't move their arms and hands, to restore that ability. The clinical trial, which is called brain gate, was set up to put electrodes into this arm and hand area of the cortex, read out attempted arm and hand movements and do things like move a computer cursor so someone can use a computer or type or move a robotic arm. It turns out we found that there's also speech related activity there, but initially the arrays, these electrodes, were put in for the main goal of supporting the arm and hand activities of this trial.
Chris - What did you see then in that area when your subjects were speaking?
Sergey - We wanted to test for the speech activity and so we had them do a very simple task. They sat in a room, they were plugged in, we were recording from their brain and we just asked them to listen, hear a word or a syllable like ba, ga, da and just say that back. This, let us record both what they were saying and exactly when they were saying and what the brain cells around these electrodes were doing. What we found was that whenever they were talking, many neurons lit up and not only were they active during speaking, but they were differently active for speaking different words.
Chris - And to be clear the same cells, if you asked them to imagine moving the arm that that part of the brain would originally have controlled, those same cells would respond to that stimulus as well?
Sergey - Yes. So it's not that this area is no longer involved in our movement. So one might think that because these are people with paralysis, so they can't move their arm, but that wasn't the case: if we asked them to try to move their hands or try to move their arm, this part of the brain is very, these cells are much more active than during speaking. It just happens that also if we ask them to talk, the same cells are involved in that and it's not just speaking if we ask them to make the muscle movements that you would need to speak - so let's say open your mouth, move your lips, move your tongue - the same cells are also active. So it's, I want to be clear, we don't think that this is related to language in sort of a high level abstract sense. It's really the movements underlying speech. So in the similar way that we know these cells are responsible for generating the muscles to move the arm and the hand, we think they're also active during the production of speech. The other thing I want to clarify is, we don't think these are causally involved - so we don't think these cells are driving the speech. It's just that, during speaking, they're also active. So it could be that they're getting some sort of copy signal for coordinating arm and hand movements, or just generally keeping track of what's going on kind of in the rest of the movement system.
Chris - Now when I'm talking to you, I'm waving my hands around. Do you think then that actually what you've uncovered here is the connection across the motor cortex that underpins our tendency to just gesticulate.
Sergey - So you've hit upon a very relevant observation. Almost all people like to move their hands when we talk. And there's a rich literature of connections between the hand and the face; some evolutionary theories that speech sort of evolved on top of hand gestures for communication. It's certainly intriguing and quite possible that what we've uncovered is related to that. But I want to be careful because we don't have direct evidence for that.
Chris - If one looks at how the motor cortex is organised, it's almost like a map of the body there, with a person with their legs dangling down on the inside surface of the brain and then stretched out, head pointing downwards, down towards where their ear is. Now the hand area is actually quite close to the head area, isn't it? So do you think what you're picking up here is just spillover: when you activate this very big territory that corresponds to moving your mouth, do you think it could just be that the facilitation that's making that possible, is just spilling over a bit into the hand area and you're just eavesdropping on a bit of that?
Sergey - I don't think it's spillover in the sense of uh, you know if you're having a loud conversation in the other room I can hear a bit of it cause it's just going through the wall. It's not that kind of signal spillover in a transmission sense. Now is it that a large area of the brain nearby is very active during speaking and it's sending some connections to this area and there's some back and forth. Spillover in that sense is very much how I am looking at this and that's what we think is going on. But these are neurons in this area that are actually firing and doing their neuron thing during speaking.
Chris - We do know of course that when people are subject to spinal injuries that there is a degree of cortical reorganisation. So to what extent do you think what you're seeing here is an artefact of the fact that the people you are studying are tetraplegic, and they've been tetraplegic for a while, and therefore they could have remapped how their cortex is wired up and were you to go and look in me, for example, you wouldn't see this relationship?
Sergey - That is a very nagging question that I wish I had the answer to. There are a couple of reasons we don't think it's remapping. If we ask the person to move their arm and hands, we see lots of activity and it looks very much like able-bodied arm and hand movement activity that we would observe in an animal model. So that's point one. Point two is if we asked the person to try to move their foot, we also see activity here and you might think, well they can't move their arm any more and they can talk. So maybe part of the brain devoted to speaking will have expanded to sort of make use of this idle brain area, but that wouldn't make sense for moving their foot because their foot is also paralysed. So, together, these things are more pointing to the hypothesis that really multiple body parts are represented across motor cortex. But you are right that we cannot rule out remapping. And because of the nature of these measurements that you have to undergo a brain surgery to have these electrodes put in, we're not going to be able to answer this in someone who is completely healthy anytime soon.
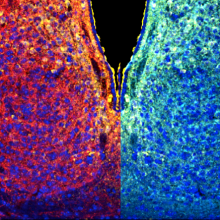
08:10 - How the brain keeps track of the seasons
How the brain keeps track of the seasons
Jennie Evans, Marquette University
Are you one of those people that dreads the onset of winter with it’s short, dreary, grey days that make you miserable and in the mood to hibernate? If so, you might have the appropriately-named SAD syndrome - seasonal affective disorder. Characteristically with SADS, symptoms of depression kick in as the days shorten, and relief only comes with the return of the sunshine in spring. But why does this happen, and what can we do about it? Speaking with Chris Smith, Jennie Evans, at Marquette University, has made the intriguing discovery that the nerve cells in the brain’s body clock - known as the suprachiasmatic nucleus - split into two separate timing devices in summer, producing much more prolonged timing signals. Locking them in this state might help to ward off SADS…
Jennie - The take home of our work is that if the brain becomes stuck in a summer mode, it may be a way to avoid catching the winter blues. There's a small part of the brain that basically acts as a calendar. It keeps time and orchestrates what our bodies do over the 24 hour day, making sure that we wake up at the right time and our hormones get turned on at the right time and we eat at the right time. And it receives light information from the environment like the sunrise, so that it's kind of set to local time and also the season.
Chris - How does it keep track of seasons? I can understand how it could track a day, because it's got the sun rising and the sun setting and that's a fairly potent regular stimulus, but how does it know when in the year we're at?
Jennie - It knows what time of day it is because the cells of this part of the brain make certain proteins and so the proteins get turned on and then they turn themselves off. So you can tell what time it is just by knowing how much of this protein is made at any given time. The way it tracks seasons is slightly different: it's the whole group of cells that act together and kind of coordinate with one another. So in the winter they're doing the same thing, at the same time. And so it's kind of the short brief signal to the rest of the body and that matches the, you know, short days of winter. But in the summer when the days get longer, these cells kind of "spread out" and they're doing things at slightly different times. So, as a group, their signals to the rest of the body, when the signal is short, it's winter. And when it's long and spread out in duration than it's summertime.
Chris - You don't mean the cells physically change position? You mean as in the stimulus, the signal that they are emitting to the rest of the brain and the rest of the body is, is spread out over a longer period of time in the summertime. But in the winter time it's a narrow focus signal on signal off.
Jennie - Yes, exactly. So it's the duration of this signal and winter it would be short and in summer it would be long.
Chris - Are all the cells in the body clock the same except they behave differently; or actually are there different populations of subtly different nerve cells in there? So it's natural for them to divide into subpopulations and have this more smeared-out function when the days get longer?
Jennie - No they're not all clones of one another. And we can recognise and kind of classify them into different groups based on the chemicals that they produce. So every single cell in the brain's clock can tell what time of day it is, but they express specialised chemicals and proteins that we use to kind of classify them into different groups. And they tend to form two main clusters that we can distinguish chemically.
Chris - And what are those clusters and how does that affect the behaviour of the whole population in summer compared with winter?
Jennie - The two clusters, we tend to kind of distinguish them chemically and spatially. There's a core cluster that's kind of in the centre of this structure, and this is the part of the clock that actually receives the light input from the eye directly. But then it transmits and communicates this information to kind of the surrounding cells. And so it's these two main clusters, the light receiving group versus the downstream group that separate and reorganise their relationships in summertime.
Chris - How did you make this discovery then? How did you identify that you've got this going on?
Jennie - Well, we used a genetic trick that was developed by Joe Takahashi. They used a firefly enzyme and they attached it to a protein that's made every day. And so we can tell what time of day it is in a cell. All we have to do is take pictures of how much light it is producing. More importantly, we can take pictures in the hundreds of cells all at the same time. So we can see kind of how they're coordinated in space and time as a population. And so we expose this special transgenic mouse to either a standard laboratory condition, or these long summer days. And so under the standard condition, the cells were nicely coordinated and synchronised, basically doing the same thing at roughly the same time. But, in the summer, these two spatially-distinct clusters of cells do very different things. And so what happens is they're basically working opposite shifts. So one group will turn on, and they'll glow, and then they'll diminish; and then eight to 12 hours later the other group will turn on. And so it's kind of, they're normally unified, but in the summer they break into these two very different groups that are representing these specialised cells.
Chris - It's like having a watch on each arm, on the watch, on the right arm goes forwards, the watch on the left arm goes backwards there. There's sort of the mirror image of each other...
Jennie - That's a really nice analogy. So what I would say is it would be like, yes, having a watch on both arms and one might be set to Hong Kong time and the other would be set to 12 hours later.
Chris - But why would the brain want to do that? What's the benefit of that?
Jennie - We don't yet know enough about what these two groups are doing and how they're communicating. So it may be the case that one group of cells kind of starts - and so it's kind of like "turn on". So maybe it communicates with the structure downstream that controls your sleep and it says, "Hey, wake up!" And then the other group of cells, 12 hours later says, "Go to bed!" So they may be very distinct in terms of the types of signals that they're providing, and if they're spread out in time, then you would have sleep grow longer or shorter. Um, so that's, that's kind of speculation. We don't exactly know why it would adopt it this way. And I think really the heart of it is we need to know more about what these cells are doing and how they're communicating with the other parts of our brain and body.
Chris - Is it that when the days become very, very long, actually it's quite easy for the clock to get dysregulated because actually when you should be going to bed, you might not feel the urge to go to bed because it's still quite light. Whereas if you've got a double push, a clock to wake you up in the morning, but one to put you to bed at night, it can overcome some of the difficulty of having a very long bright day?
Jennie - That's a possibility.

16:02 - How long does Zika virus immunity last?
How long does Zika virus immunity last?
Alasdair Henderson, London School of Hygiene and Tropical Medicine
Zika virus, which is spread by mosquitoes and has been linked to birth defects including microcephaly, made headlines in 2015 when it began circulating in Brazil. Before that though, it had caused major outbreaks in Micronesia and Polynesia, the latter being the likely source of virus that spread to Brazil. Now, literally billions of people live within the “Zika belt”, the zone of the planet’s surface where people, the mosquitoes that spread it and the virus itself all co-exist. As such, disease monitoring, and development of effective vaccines are a priority. But working with blood samples collected over an extended period of time, as he explains to Chris Smith, Alasdair Henderson has found that something strange happens to a person’s immune response to Zika: it disappears...
Alasdair - So we looked at two countries that had Z outbreaks, and within approximately 18 months of those outbreaks ending, we found the number of people that still had antibodies against Zika much lower than we expected. It seems in both of these countries and both of these settings that adults in particular are losing their antibodies to Zika specifically.
Chris - And just to be clear, this is not normal for someone who's encountered a natural infection with a viral illness, is it? I mean, if we looked at measles, for example, we would find antibodies for life after that?
Alasdair - Yeah. Measles is a good example but also dengue, which is a closely related virus to Zika. We commonly assume that if you're infected with dengue, you are immune to that type of dengue for the rest of your life, which is what we expected to find with Zika. But our results didn't show that.
Chris - Interesting isn't it? Because Zika and dengue are actually quite close relatives aren't they? They're both flaviviruses, and they're not that different. So it's interesting that you've spotted this disparity?
Alasdair - Yeah, I think the fact that we worked quite well between some partners in Fiji and French Polynesia, and we found the same discovery in both locations, was really interesting.
Chris - I'm glad you brought up the location cause I was going to say where did you do the study and how did you do it?
Alasdair - I am doing a PhD, which is kind of based in the Pacific, but specifically in Fiji. And there'd been two studies previously looking at different diseases in the past. So, in 2013, some researchers from the London school went and were studying typhoid and leptospirosis. There was then a big dengue outbreak. And in 2015 more researchers went out and sampled the same individuals to collect their blood and test for antibodies after the dengue outbreak. There was then some confirmed Zika cases, so I went out in 2017 and tried to find as many of the same people again. So we had serial blood samples from the same people.
Chris - So although blood had previously been collected for other purposes, you were able to go back and then look retrospectively for Zika antibodies in there and compare those historical samples with the ones that you got more recently?
Alasdair - Yeah. While it wasn't the focus of those original studies, they tested against a whole variety of viruses, um, at the same time and over time we found these interesting dynamics, particularly with Zika.
Chris - And how dramatic were the differences. If you look at the numbers of people who tested positive originally and then seemed to lose their antibodies, how many people was that happening to?
Alasdair - So if we look in Fiji specifically that 2013 study we found about approximately 6% positive for Zika. Two years later that number had gone up to 24%, and then two years after that we are expecting it to be at least 24 possibly higher. But we actually found that it had dropped to 12%.
Chris - And if you arranged people by age, was there any difference? Because we do know that people respond differently to infectious challenge at different ages. So can any of this be explained on the basis of the age of the individuals?
Alasdair - Yeah, it seems that way. We've shown here in adults that drop in antibodies seems to be where it's concentrated. But actually if you look at school children or children below 16, they keep their antibodies.
Chris - What do you think the mechanism of this is?
Alasdair - It's hard to say at this stage, but one of the possible mechanisms is, because people who are older are more likely to have had more infections over their whole life, including dengue, potentially, if you've had a lot of dengue in the past, you might not keep your Zika-specific antibodies as well as a child who might not have experienced as much dengue.
Chris - Does it also mean just because someone does record a low level of antibody, we know for example with other infections, chicken pox is quite a good example of this. There are some people in the population when we test them, they relentlessly test negative for chickenpox antibodies, but they don't catch it and it looks like they have, they have indeed had it in the past - they are immune, but they just don't come up on our tests. So are we seeing a sort of similar phenomenon here where we might have people that are actually immune to Zika, but they're not recording any demonstrable antibody levels?
Alasdair - Yeah, and I think that touches on this potential idea of cross protection. So, with Dengue there are essentially four types of dengue, and infection with one can lead to a period of cross-protection where you can't get infected with other types. We might be seeing a similar thing with Zika here, because we looked at two different tests. So one of them looked for a specific response to Zika that's called the MIA. And the other one looked at how well people's blood could neutralise each virus. And actually we found that people who were negative on the MIA - so didn't have specific Zika antibodies - still had quite high neutralizing antibodies. So whether that means that people are still able to fight off Zikar infection, we don't know, but it's indicative of that.

22:14 - Human body temperatures are falling
Human body temperatures are falling
Julie Parsonnet, Stanford
What’s a “normal” human body temperature? Probably not what you’ll likely see documented in the text books, as - speaking from Antarctica to Chris Smith - Stanford’s Julie Parsonnet explains…
Julie - The number that most people use nowadays was established in the 19th Century by a German doctor named Carl Wunderlich, who took about a million temperatures on 25,000 people. And on little pieces of paper, wrote them down and did all these calculations, figuring out what is the right temperature for the time of day and for women and for men. And really, he did it absolutely stellar job. Just fantastic. Um, but things have changed since the middle of the 19th Century.
Chris - In what way?
Julie - We're a lot healthier now than we were then. We have a lot fewer infections. We live in much more comfortable circumstances. We do a lot less physical labour. We have much better homes and much better hygiene and we've gotten taller and we've gotten fatter and we've gotten colder. We took temperatures from civil war soldiers in the, from the 19th Century - so people who are born as early as 1800 actually - and then we compared them to temperatures from two other groups: one that was in the 1970s, and then our clinical data that we have from Stanford University with a lot of temperatures, and we found that the temperatures are declining over time and we couldn't explain it by just the thermometers that were used or the way they took their temperatures. We did a lot to try to piece through that. It really appears that people who live in the 19th Century just had a really harder life. They had a lot more infections, things like tuberculosis and syphilis and rheumatic heart disease, and they lived under harsher conditions. They had no air conditioning and heating and their lives were just harsh enough that they just had to rev up their bodies all the time to keep themselves safe, to keep themselves healthy. They had to fight all those infections that were taking a lot out of them by increasing the metabolism.
Chris - How much of a difference is there comparing people? When Wunderlich did his research in Germany in the 1850s and today
Julie - It's about 1.1 degrees Fahrenheit is about the difference that we see between then and now. But I do want to make the point, 1 degree Fahrenheit is a lot, but we could see a fairly big difference within a person almost that high even today. So if you take a temperature, compare the temperature of a young adult late in the day with an elderly person early in the morning, their temperature might be more than one degree Fahrenheit different. So that although 1.1 on average seems like a big difference, temperature does fluctuate from person to person and from time of day especially, and by age. And so, again, I do think that that we shouldn't all expect our temperature to be exactly 37.5. We're all going to vary and we need to start thinking about that a little bit.
Chris - It's an interesting hypothesis and it's biologically plausible that the lower burden of disease in the population is translating into a lower average body temperature. But are there any actually studies that would support that hypothesis?
Julie - There are not a lot of studies that look at why this would happen that would show the reasons that it might've occurred. There is one study that was done a few years ago that looked at the level of inflammation in people since even 20 years ago and they shown that our inflammatory levels - the rates of proteins that indicates inflammation - have dropped even over the last 20 years. So that supports our underlying hypothesis that this is, that we're becoming less inflammatory, that we are just having less things that are revving up our immune systems. And there are also some data that suggests that at least one other country that has a lot more infectious disease burden, Pakistan, their temperature is still high. It's still 98 six so again, it supports that there are things that correlate with inflammation that are also correlating with temperature.
Chris - If one looks back in history, you can see that in fact disease was concentrated at the bottom end of the social spectrum and there were different diseases, perhaps diseases of affluence at the top end of the social divide. If you stratify your data by social class, can you see a temperature effect in there from the early days because obviously people with a lower burden of disease would have had less inflammatory stimulus and therefore their body temperature, if you're correct, would have been a bit lower.
Julie - We haven't really looked at it. The people that we're looking at are all veterans of the civil war, which makes them a rather unique group and people who required getting their pension to move forward in life. So they're not people who are at the upper end of the spectrum who could get by without their small military pension. So we didn't really have a great diversity of population and wealth. But I, you know, it's an interesting question. I think it's worth going back and trying to see if there's a better way that we can piece through that information and, and look into that hypothesis. We did look parenthetically at individual infections and say, did these raise temperatures? And if we exclude people with these diseases, does it matter? And we did find that people who said they had tuberculosis, which is a very small number, and people who said they had bladder infections did have higher temperatures overall. So we could find signs that the temperatures we were reading were accurate and that these infections do affect things.

27:40 - Investigating the leaky pipeline
Investigating the leaky pipeline
Marcus Lambert & Linnie Golightly, Stanford
Frequently here on the eLife Podcast we touch on topics that concern scientific careers, or what life is like for the present generation of researchers. Last month we looked at how well supported early career scientists are in terms of their mental health. This time we’re considering why, despite the fact that we’re actually pretty good at recruiting into science individuals from backgrounds regarded presently as “underrepresented”, but we don’t seem to be very good at hanging on to them once we’ve got them, as Chris Smith hears from Marcus Lambert and Linnie Golightly…
Marcus - My name is Marcus Lambert. I'm an assistant Dean for diversity and student life at Weill Cornell medicine and an assistant professor in our department of medicine.
Linnie - I'm Lynnie Golightly. I'm an associate Dean of diversity and inclusion at Weill medical college and associate professor of medicine. We really are interested in diversity because that means excellence. And we were trying to understand why after people having invested in our society, having invested in people going through undergraduate, graduate school and then entering a postdoctoral fellowship, we then choose to go into an alternate caree,r because they're very valuable and we want them to be part of our research community.
Chris - But implicit, Linnie, to the point you just made is that that is a fact - that people are not doing that. So what's the evidence that that's true?
Linnie - Well, we have very low numbers historically in the Academy of people of colour, and women, for a number of reasons. Actually anyone who we lose is important because our numbers are very low. So it's trying to understand what factors might cause anyone not to continue.
Chris - And, Marcus, how did you approach this?
Marcus - Our approach here to really develop our own unique survey to really understand the factors that contribute to people's career choice. Specifically scientists in their postdoctoral research phase. We also looked at things like self efficacy and outcome expectations; things that might not be so evident, but could be playing a big role in how people make their career choices.
Chris - And who answered the survey?
Marcus - We distributed this to postdoctoral listservs across the United States. So it was mostly post docs.
Chris - And what sort of reply rate did you get though Marcus? Because obviously one always worries, when you send out a survey, that only people with a particular axe to grind or people who are particularly successful bother to fill it in?
Marcus - We didn't exactly measure our response rate. We got about 1,284 responses, which we felt was pretty representative of the pool. Uh, and with good geographical diversity as well.
Chris - And Linny what were the questions that were on that survey and what results did they elicit?
Linnie - Well, we had a number of questions trying to understand better how they felt about themselves, how they felt about the likelihood that they would succeed. We looked at the number of papers they had, what kind of impact the papers were, the types of institutions that they were at; their mentorship; their lifestyles; financial security; those sorts of questions to try to get a full picture of their ideas towards themselves, towards the places that they were working and the impact it might have on their family and their, uh, futures.
Marcus - And Chris, we also ask questions related to things like, can I publish in top scientific journals? I am confident that a, I can secure grants in my field. And this led us to some clue about their level of self efficacy compared to other postdoc respondents.
Chris - And broadly, Linnie, what trends emerged? What did you find?
Linnie - Well, we found that the first two years of the postdoctoral training was really critical. That was a period of time during which people might change their minds, both women and underrepresented minorities in terms of leaving the academic research pipeline. We also found that financial security was very important; that mentorship from their PI was very important; and that their sense of self worth was very important.
Chris - So at the end of that two years, is that a make your mind up point then if people have made it past two years, they tend to then go the course?
Linnie - After those two years, people really have made a decision to go one way or the other. So I think that what we would think and what we would say would be when someone first enters their postdoc, you really need to address the things that we've found would emerge later in order to try to encourage them and have them stay the course. So for example, one of the main things that we found was that underrepresented minority post docs unlike their peers felt that they were not meeting people within the Academy who they really wanted to be associated with. And so that's sort of an understanding that, if you continue on this career, you'll have people that have different values than you is really something that should be addressed early on so that people don't leave.
Chris - Indeed so, Marcus, that must be your target point: you've got to focus your attention on those first two years in order to make sure that people make their mind up to stay?
Marcus - Yes, I would agree. You know, one of the two biggest points where we see the largest drop-off for postdoctoral fellows are really at the end of year two and at the end of year five. And it was particularly at the end of year two that we noticed that there was this difference between women and underrepresented postdocs and their well-represented counterparts for well-represented males specifically. You don't see that drop off at year two. You really start to see the dropoff after year five.
Linnie - One of the other things to raise is that female postdocs were a little bit different than their male counterparts in that there's this issue of self efficacy: that is, a belief in one's own research abilities was lower and that they had lower outcome expectations that the belief in the outcome of their research efforts than men. And so this is also something that we need to address in terms of empowering women to understand that they are just as capable and to believe in themselves as much. And so one of the questions is what happens, and again, these are historical reasons, but for someone to come all this way and get all these degrees and be in their postdoc and yet not feel that sense of yes, they can do it, it means that we're not really doing our full jobs in the Academy.
Chris - When you look at what you have found here, does it give us almost a wishlist of things that we could do - we could implement - in order to address the problems that have been highlighted? Or are we just left with a bunch of questions?
Marcus - I would really argue that institutions hold a lot of power and being able to change the sort of dynamic here, and making sure that people feel empowered to choose the sort of career paths that they want to choose. And I would argue that we have a lot of ability to provide the level of support to postdoctoral fellows that we do to undergraduates that we do to graduate students. And I think postdocs are often sometimes overlooked in this path.
Linnie - Yeah. And I think that we definitely have, not a wishlist and not just a bunch of different things that we might do, but we really have a clear path. I think that support systems need to be multifactorial and look at the many different dimensions of the person you're talking about. It's not just the number of papers, it's not just that you're at a wonderful institution, it's who are your peers. It's what are your supports. It's is somebody talking to you about financial security? Is someone talking to you about how do you balance your research and your teaching about, yes, you can reach out to your community yet still do suburb research. If you look at the person as a total, I think we can do a lot better. And we'll where we forward these people staying in the Academy.










Comments
These are hardly full
These are hardly full transcripts! And no references. Is something wrong here?
Maybe you missed them? You
Maybe you missed them? You have to click on the titles of the interviews, or "full transcript" to drop down the content. The references are below each of the interview transcripts. They are visible on the interview pages accessed by clicking the title of each interview.
Add a comment