This month we’re taking a look at the role that genes play in dementia, and finding out how researchers are using this knowledge to develop urgently-needed treatments. Plus, a big release of big data from the UK Biobank, and our gene of the month is an expert swordsman.
In this episode
Is dementia in your genes?
with Jose Bras and Rita Guerreiro, UCL
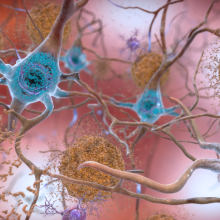
Dementia is an umbrella term that covers a range of neurodegenerative diseases, including Alzheimer’s (which is the most common form), fronto-temporal dementia, vascular dementia and more. Yet although these conditions all have different symptoms and affect different parts of the brain, they all boil down to the same biological principle: nerve cells dying. And while there are treatments that can help with the symptoms of some types of dementia, we still have no cures.
To find out how scientists are using genetics to understand dementia, Kat Arney went to the UCL Institute of Neurology to meet husband and wife team Rita Guerreiro and Jose Bras. She started by asking Jose to explain what we know so far about the role of genes in dementia. In particular, Kat wanted to know whether these conditions are caused by genetic changes that we pick up during a lifetime - as is the case with cancer - or whether they’re influenced by genetic variations that have always been there.
Jose - As far as we know, it’s more from birth. So in cancer, it’s slightly different because you can go into a tissue that has the disease, that has cancer, and you can see if there are changes.
In people with dementia, you can't go into the areas of the brain where the disease is occurring and look at the DNA of those cells only. You can't stick a needle into a brain of a living person and get some DNA out of it. So, as far as we know, it’s more changes that come with the person’s genetic makeup.
Kat - What sort of genetic variations and changes seem to be the chief suspects?
Jose - So for all of these diseases, for all of these dementias, we have a number of genes that we know are involved, and they're different for almost all of the diseases. There's a couple of ways in which we look at genetics involved in dementias. We look at genes that cause each of these diseases and these are genes where very rare mutations occur, and when they're there you get disease.
Kat - Would those be the kind of conditions that you can see going through families? You get some families with lots of the same type of dementia.
Jose - Exactly. These are exactly those types of mutations that lead to these diseases. They are very rare. It’s a small proportion of – for example, in Alzheimer's disease – small proportion of all Alzheimer's disease is familial, has these mutations in a small proportion. But on the other hand, even knowing that a gene that’s very rare is involved in a disease is incredibly informative for us because it enables us to identify biological pathways that are involved in these diseases. And so, it’s a very active area of research finding these genes.
Kat - So Rita, in terms of trying to understand how these genes, these faulty pathways might be involved, what sort of approaches are you taking in the lab, working together?
Rita - We use two main approaches in the lab. We look at genetic variability in families and we compare this genetic variability between individuals that, for example, are living with dementia and individuals in the family that are healthy. By comparing the genetic variants within the family, we are – in some cases – able to identify the mutations and the genes that cause the disease in that family. And so, this is used mainly to find causative mutations.
When a patient has that mutation, he or she will develop the disease within their lifetime. But we also use this genetic variability to compare between large groups of individuals living with dementia and large groups of healthy individuals. When we do this type of comparison, what we are trying to do is to identify risk factors. Variants in the genome of these individuals that will either be protective for dementia or that will increase the risk for the development of dementia in these individuals.
We have moved from being able to look at maybe a handful of variants in maybe a couple of hundred individuals at the same time. Now, we can look at the whole genome base pair by base pair, so a really incredible resolution when we do this. And we can do this in an enormous number of patients and of people, so this really was a very, very big advance in the past decade.
Kat - If there's one thing I know about genetics, it’s that there has been a huge explosion of data and techniques, but - oh my goodness! - it has made things very complicated. So how do you go from – as you described, you’ve got these very kind of strong affecting gene variations, mutations that track through families, you know they definitely evolve, they definitely make cells go wrong, cause the cells to die in certain types of dementia.
Then you’ve got all these genetic variations in thousands and thousands of people that kind of subtly raise or lower their risk of the condition. How then do you pin those genetic variations to actually doing something? How do you know what all these hundreds, thousands of genetic variations might actually be doing?
Jose - That's a very good question and it’s a very difficult question to answer. So when we do these studies that Rita was mentioning – these association studies – we identify really regions of the genome that are involved in the disease. We don’t identify genes and we don’t necessarily identify variants that are themselves increasing or reducing risk for disease.
Again, from the region so the actual variants and their effect is incredibly difficult. And so, these are things we’re working on at the moment. It’s a very important question to answer, but for the vast majority of these regions, we haven't really been able to identify the driving mechanism of those associations.
Kat - Given that you are finding these variations, you're trying to study them, it sounds like a terrible question to ask but, what's the benefit? How can this actually improve the situation for people living with dementia, with their families? What do you do with this knowledge?
Rita - The first answer to that is directly to the patients. It’s very difficult to see what is coming out from here, but from a disease perspective, it gives us an enormous knowledge about the biology and the pathobiology of what we are seeing in the patients. Of course, the goal is to have this information and develop therapies, and develop new drugs that are targeted to these genes or to these proteins.
Now in terms of genetic variability and risk, what can be done and what is currently being worked on is to just model the risk of which per cent according to all the variants that they have and put this all into the same model and just get a score at the end that will tell us eventually if that person will have a much higher risk of developing disease or not.
Jose - One of the things for which these scores are important is for clinical trials. So we want to have the best cohorts in our clinical trials so that we get the most powerful answers from these trials. If we can identify the individuals that are more relevant to each study that we’re doing based on their genetic makeup, this is going to enable us to have much better clinical trials and what we’ve been able to do so far.
Kat - So there are direct to consumer tests – things like 23andMe and they look at – particularly, there's one variation that’s associated with the risk of Alzheimer's. I think it’s the APOE gene. What can people take away from this kind of test?
Rita - So, it is the strongest genetic risk factor for Alzheimer's disease. With this said, this means that if you do have the risk allele which we call the E4 allele, it doesn’t mean that that person is going to develop Alzheimer's disease. It just means that it’s at an increased risk for the development of the disease.
Jose - Personally, I am in favour of direct-to-consumer tests. I always think that having information is a good thing. Of course, you need to be able to deal with the information as what Rita was eluding to. But on the other hand, you want to know as much as you can about yourself. This is one very good way of knowing quite a few things about yourself.
Kat - If you did discover you carry this variation that increases your risk of Alzheimer's, is there anything that can actually be done? We hear about things like – to reduce your risk of heart disease, you should exercise, you should eat healthily. What could people do – if anything – to reduce their risk of dementia?
Jose - Well, you can exercise your mind. That’s one of the ways that we think helps. You can keep an active mind, keep an active body. We think all of these things are helpful, but of course, we don’t have therapies. So having a strong risk factor for Alzheimer's disease perhaps will enable you to start to do these things earlier.
Perhaps this will delay the onset of the disease if you ever get to develop the disease because as Rita said, having an E4 allele doesn’t mean you'll get the disease. So, having the information is perhaps in many instances is a very useful thing.
Kat - Jose Bras and Rita Guerreiro from UCL’s Institute of Neurology.
10:25 - Guilt by association
Guilt by association
with Raffaele Ferrari, UCL, and Claudia Manzoni, University of Reading
We’re starting to discover some of the genetic faults and variations that are associated with dementia, but we don’t know much about what they actually do. Two people who are trying to find out are Raffaele Ferrari, also at the UCL Institute of Neurology, and Claudia Manzoni from the University of Reading. Kat Arney spoke to them to find out more.
Raffaele - The one thing you really want to do is to identify genes as a first thing because there is a direct relation between genes and proteins which is important because we immediately know what the effect could be.
Kat - So this is finding out what genes makes stuff that’s in the nerve cells that could be going wrong.
Raffaele - Right. We would be able to name a protein which is affected by the genetic variability. There is a direct relationship between a gene and the protein. Normally, we know about the function of a protein so we may be able at first sight to understand a little bit more about what is molecularly happening within either brain cell.
Kat - So you can say, “Well, this gene looks like it’s quite badly broken. It’s probably going to make a badly broken protein, so it’s probably not going to work.”
Raffaele - That’s a great thing that we can do but this is literally just a tiny piece of information that is not still able to give us a broad view of what's going wrong in the brain cells.
Kat - So the basic problem is that sequencing studies, genome-wide association studies, that family studies have thrown up all these genes or these areas of DNA that you say, “Yeah, they're doing something in these kind of diseases.” But we still don’t know what – so I guess it’s like, if you look at an office, you can say, “Okay, this person works in an office, but we don’t know what their job is and what they're doing.”
So Claudia, how do we try and take these genes, what we know about the genes, and work out what the flip are these things actually doing because it’s alright to have a list I guess of the genes that you find. But it’s nothing if we don’t know what they do.
Claudia - This is exactly the problem that we are facing, that everyone is facing. Genetics from a certain point of view is simpler than functional biology because you identify genes in isolation. But then when you try to understand what that gene does, you need to go into the cell environment and the gene in the cell environment, works in cooperation with other genes and proteins. So you need really to look at something that is more complex.
Functional biology normally takes a lot more time than genetics to then analyse and identify the function associated with a certain gene. Even when we know the function that is associated with a certain gene, maybe we don’t know the function in disease because the function of a gene in the normal condition is one thing, but then we need to understand how the function changes when there is a mutation.
Kat - So normally, we do this with all those pesky experiments in the lab with cells or with animal models taking years and years, and years. I know people can spend an entire career just studying how one gene and the product of that gene goes wrong in a certain disease. We haven't really got that kind of time. What are you doing to speed that up?
Claudia - And also the money that you need for doing all those experiments. So, this is why Raf and I started talking a few years ago now about how can we think of doing something different and find a way to not solve the problem, but to find a way to ease the passage of information from genetics to the functional biology.
Kat - So to give you some kind of clues about where to start looking at the function.
Claudia - Yeah, exactly. So, we decided that the way to go was to stop looking at one gene at a time, but try to have a more broad look, a more general overview of what's going on, evaluating all the genes that we know are associated with a certain trait, and look at all the genes together to see whether they will point us in a certain direction. For doing that, we decided to start using databases that are already available, already generated, and are freely available in the public domain.
Kat - To go back to the office analogy, you're trying to use data that's already out there to work out – does this person work in the finance team or the human resources team? – what sort of data are you looking at?
Claudia - Yeah. We look at a protein-protein interaction type of data at the moment. We are planning to move to other data sets but at the moment, what we are really focusing on is protein-protein interactions. The idea is that proteins that work together, they interact. There is a principle which is called Guilt by Association principle.
If we know the function of protein A and we know that protein A interacts with protein B, but we don’t know the function of protein B, well, just by knowing that protein B is able to interact with protein A, we can infer the functional protein B. So we are using this principle to build networks of proteins, knowing that they interact together and to see for known proteins, to see in which pathways, in which functions they are associated based on the network of other proteins that they interact with.
Kat - To go back to our office analogy, if you know that two people are always going to meetings together, they're probably working together.
Claudia - Yeah, exactly. That is the perfect analogy, yeah, definitely.
Kat - So through this work – through understanding the genes, getting really good clues about what they do to direct the lab research at the right way, to find targets for drugs, what do you want to see as the key outputs for this? What do you see as coming out to benefit patients and how long, how far away is that going to be?
Raffaele - Ideally, I think we’re talking about two outcomes. One is that of understanding the molecular mechanism – what is impacted in the brain cells that leads to their death? This is critical because if we don’t know that, we don’t know how to handle it and how to fix it in a way, if it works out, it’s rewarding, just the beauty of understanding something. On the other hand, the understanding can lead to identifying either biomarkers in both preventive medicine or as a monitor of the disease progression, or as well as for developing therapeutic measures. We might be able to identify elements that fit all of these needs – so preventive measures, monitoring measures, or therapeutic measures.
Claudia - And the other point is that if we know the mechanism, we can actually think of a drug that is able to impact the mechanism because at the moment, we don’t have drugs. We don’t have therapies for all these disorders unfortunately. But we have some drugs, that we can prescribe to patients but these are symptomatic drugs. So they don’t cure the neurodegeneration. They just work on the symptoms.
For example in Parkinson’s, we can reduce the tremors, but we don’t stop the progression of the disorder. But if we really know the molecular reason why the cells in the brain are dying, we can think of an intervention that is actually directed to the problem and then we can prevent or stop the neurodegeneration. So, this is why it’s very, very important to understand the molecular mechanism at the base of the degeneration.
Kat - Raffaele Ferrari from UCL and Claudia Manzoni from the University of Reading.
18:60 - UKBiobank: Big data, big release
UKBiobank: Big data, big release
with Peter Donnelly, Wellcome Trust Centre for Human Genetics, University of Oxford
This month saw the release of the biggest ever dataset from the UK Biobank - a huge long-term study of human genetics and health. Researchers all around the world are able to apply to download the data and trawl through it to answer vital questions about health and disease. Kat Arney spoke to Professor Peter Donnelly, the principal investigator of UK Biobank, based at the Wellcome Trust Centre for Human Genetics in Oxford, to discover what the fuss is all about.
Peter - The idea behind UK Biobank was to collect a very large cohort of individuals in what's called a prospective study. So those individuals are recruited, they give consent for a range of studies to happen at the time they're initially studied, and then over time, there’s further information collected either directly from individuals or with their agreement to link with medical records. So it gives you a resource which is valuable and interesting from day one, but which in some sense matures. As time passes, some of those individuals go on to develop some diseases and others would develop other diseases. The very important thing about the prospective study is you measure lots about the individuals before any of that happens. So you can look back and see if individuals with these properties are likely to happen, and so on. And the fact that it’s as large as it is 500,000 individuals, it is a real key to its value and its added success.
Kat - In terms of looking at this kind of genetic level, what have you done?
Peter - A few years ago, UK Biobank convened a group of many of the experts in human genetics in the UK to think about how to get best value out of the UK Biobank results in terms of genetics. The very strong view of that group at the time was that the right way to do it then was to measure genetic information in all of the participants of the UK Biobank. If you are able to decide in advance a set of positions in our genome in our DNA to measure then that can be done these days reasonably economically. And so, there was an expert group convened to design the chip, the array that does the measuring for each individual, and for each person, that allows measurement of about 800,000 positions in their DNA, in their genome. And we’re able to choose them so that we’d include lots of things we thought might be interesting for diseases, other things we thought might be interesting for other reasons, and then many, many other markers or genetic variants or snips – as we call them – across the genome which allow us to interrogate the whole genome recently effectively.
Kat - So we’ve got this 500,000 people, we’ve got all these genetic information – you’ve genotyped them – what other information have you got about them?
Peter - One of the enormous strengths of UK Biobank as a resource is the depth and the breadth of information that’s measured on the 500,000 participants. So, when each of those individuals was initially recruited to the study, they spent half a day or so at what's called an assessment centre where a lot of information was collected about them. They were asked questions about themselves, questions about their medical history. Many things were measured about them – height and weight, things about their vision and their lung capacity. So, there's a lot of measurements about them as individuals. They get blood samples. So some of that had been used for the DNA analysis to have a genotyping, but other aspects of those, blood samples are used to measure – what we call biomarkers, so things like cholesterol levels, other things that are informative about the health circulating in our blood. Since the initial assessment, there had been follow up studies on collections of subsets of the cohort to get more detailed information from them. A subset of people give information about their diet over a period of time which is available on those individuals. There's been some re-assessment of individuals. In a really exciting development recently, there's imaging, so different sorts of medical imaging done on people’s brains and their abdomen, and their arteries, and so forth which again, is a rich source of information. Recently, UK Biobank has succeeded in linking some of the health information kept in our NHS records with the individuals. So there's an enormously rich collection of information of many things like height and weight, and then various medical things, and really detailed things like images, measurements and biomarkers on all these individuals.
Kat - This is something that you are putting out into the world and you want people to use. What sort of things could researchers look for in there? How do you see people using this data? What sort of questions could people ask with it?
Peter - I think there are a number of very natural things that people want to study but one of the really exciting scientific opportunities is the resource is so vast in terms of their genetic data, and all the other things that are measured on people that I'm sure there’ll be really clever scientists who think why it’s worth exploring that data to tell us things about human biology and human disease that we wouldn’t guess now. So that’s really exciting. The obvious things people can do, they can look at the relationship between genetic information. We have various outcomes that people have – now those outcomes might be in terms of whether they get diseases or not, arthritis or heart disease. That could be really helpful in understanding more about the disease and in time developing new treatments for the disease. Another really important thing which UK Biobank will enable researchers to do is to understand the way risk factors we have from genetics interact with other things around us like our diet, our lifestyle, other aspects of our health. In fact, it’s one of the key drivers in setting up the UK Biobank resource was to have a study which was firstly, large enough and secondly, collected the right kind of information to allow researchers to do exactly that. So up until now, largely, we’ve been able to look at how whether you have this genetic variant or this one affects how likely you are to develop the disease. But what UK Biobank allows is to ask questions like, if you have this variant rather than that variant and this diet rather than that diet, does it matter? So, helping us to learn about the ways in which the stuff we inherit – our DNA – interacts with things around our day to day life, both the choices we make and the things that we interact with in the environment. The ability to study what’s called gene environment interactions will be a really powerful use for UK Biobank.
Kat - So sort of opening up the black box between our DNA and the way we come out?
Peter - Absolutely, yes.
Kat - In terms of this as a scientific achievement, what does this represent?
Peter - I think there's no doubt that as a scientific research resource, UK Biobank as it stands now is an extraordinary collection of information for researchers. It’s by a long way – I think – the most valuable resource of its kind available anywhere in the world. One of its strengths is that it is available to researchers around the world, researchers who are working to answer questions that are consistent with the mission and the framework of UK Biobank and it will only improve. It will improve in two ways. There will be more information collected about the individuals in the study and as time passes, there’ll be more outcomes in terms of the diseases individuals suffer from or other things that happen to them which will be helpful for researchers to study.
Kat - How would you summarise your hopes for this dataset and maybe for UK Biobank more broadly, say, over the next 5 years? Where would you really hope that this will go?
Peter - I think scientists studying the Biobank resource over the next 5 years will uncover a whole lot of novel really key insights about human biology and human disease, and some of those will have immediate impact in terms of the way we treat patients. Others of them will lead to new ways of developing drugs, new ways of choosing treatments in particular situations. Its impact on human health and healthcare will be enormous I think.
Kat - Peter Donnelly from UK Biobank. And if you’re a scientific researcher and you’d like to get your hands on the Biobank data, you can apply through the website - that’s ukbiobank.ac.uk

Gene of the month - Musashi
First discovered in fruit flies in 1994 by a Japanese researcher, Makoto Nakamura, while working in Baltimore in the US, Musashi is named after the 17th century samurai warrior Musashi Miyamoto, who devised a fighting style of wielding two swords at the same time rather than just one. Rather than waving swords around, fruit flies with a faulty version of the Musashi gene have double rather than single bristles popping out over their bodies.
It’s now known that Musashi binds to certain RNAs - the molecular messages produced from active genes - and affects how they are processed and read by cells to make proteins. It seems to have a particular role in ensuring that stem cells in the nervous system maintain their stem-cell abilities. This explains the double bristle effect: fly bristles are made up from four cells - two are nerve cells, while the socket and bristle shaft are not. Without Musashi, there’s nothing to stop one of the nerve cells becoming a bristle shaft too.
There are a few mammalian versions of Musashi, which also seem to be involved in maintaining nerve stem cells and other stem cells around the body. Intriguingly, they get reactivated in some brain tumours and other cancer types, suggesting they might be causing cells to forget what they’re meant to be doing and revert back to more stem-like behaviours.
Check out this news story to find out how the Musashi gene might hold the key to better Zika virus vaccines and even a treatment for brain tumours.










Comments
Add a comment