Under the microscope this week, where new flu viruses including influenza H7N9 come from, the threat from extensively resistant tuberculosis and how doctors keep tabs on how bugs are spreading and who they are infecting...
In this episode

01:12 - Vaccine for dust mite allergies!
Vaccine for dust mite allergies!
It's the dream of many allergy sufferers to have some kind of jab that would vaccinate them against the misery of their reactions. Now new research from a research team in Thailand, working with a company in the US, have taken a step forward in developing a DNA-based vaccine that could be tested in clinical trials for people who are allergic to house dust mites - an allergy that affects up to one in five people in industrialised countries.
Over recent years, sc ientists have tried to cure allergies by exposing sufferers to tiny amounts of the proteins that trigger their reactions. The idea is that it stimulates helper immune cells, known as TH1 cell, that damp down the overactive, allergic immune response. But these treatments can take years, and there's a risk of triggering a massive reaction by accident.
ientists have tried to cure allergies by exposing sufferers to tiny amounts of the proteins that trigger their reactions. The idea is that it stimulates helper immune cells, known as TH1 cell, that damp down the overactive, allergic immune response. But these treatments can take years, and there's a risk of triggering a massive reaction by accident.
Writing in the journal Immunology Letters, the scientists have developed a vaccine based on a tiny fragment of DNA that encodes the instructions to make a protein, called Der p2, which is found in house dust mites. The idea is that when the DNA is injected into muscle, followed by a harmless little electrical pulse, cells take it up and start making a small amount of the mite protein. This helps to encourage the helper immune cells that damp the immune response, as well as helping to switch off the bad immune cells that are responsible for the allergic reaction.
In this paper, the researchers were working on tweaking the DNA in the vaccine to get the best response, as well as testing the best way to deliver it and the best dosing schedule to use. When they tested the vaccine in mice, they found that it could stop dust mite allergy from developing by triggering the good helper cells, suggesting that it's working as they'd hoped.
The scientists think their results could support moving their vaccine into clinical trials in humans in the near future. However, manipulating the immune system in this way is a tricky business and there are risks involved, so more work needs to be done to make sure any vaccine would be safe. So the dust mite allergy sufferers amongst us will just have to snuffle and wheeze a bit longer.
05:49 - Milk Monitor Collars Spoilt Dairy
Milk Monitor Collars Spoilt Dairy
If you've ever accidentally put spoilt milk in your tea or on your cereal you'll know it's an experience you don't want to repeat. One way to stop this culinary disaster is to have sophisticated electronic sensors that can pick up chemicals produced by milk when it spoils and then display this on the side of the package. Unfortunately, this is a rather expensive gizmo to add to every single carton of milk given the millions manufactured every day.
Chinese scientists think they have a cheaper solution to this problem. And they're relying on the same phenomenon that medieval stained glass window artisans have made use of for centuries - plasmonics. The new sensor doesn't pick up on noxious volatiles from food, but instead uses a simpler method that displays - with a simple colour change - how old the milk is, and to temperatures to which it has been exposed.
Gold nanorods suspended in a silver solution are the basis for the sensor. Thenanorods appear red rather than the gold we'd expect because, at the nanoscale, metals can interact with light in unusual ways, absorbing and scattering some wavelengths and reflecting others. Stained glass window makers were unwitting nanotechnologists and made use of this effect by putting metal salts into their glass: the vivid ruby reds in these windows are produced by gold nanoparticles, for example.
In the sensor, the silver ions slowly coat the nanorods, altering the way they interact with light and changing their colour from red to green. This change happens much faster when it's hotter, and so gives the consumer a brief history of the milk in a simple display. This display needn't just be used for milk, and would be especially useful for products like meat or seafood that can make you very ill if they warm up enough for bacteria that can cause food poisoning to multiply. The authors hope to roll out their sensor as soon as possible - you just need to remember that in this case red means go while green is the signal to stop eating!

09:57 - Quickfire Science: 3D Printing
Quickfire Science: 3D Printing
3D printing is a technique that's dramatically reduced the cost of building  complex plastic objects in recent years. But this week in the US, the first ever shot was fired from a gun that was built using 3D printing. Here's your quickfire science about the technology from Naked Scientists Elena Teh and Pete Skidmore...
complex plastic objects in recent years. But this week in the US, the first ever shot was fired from a gun that was built using 3D printing. Here's your quickfire science about the technology from Naked Scientists Elena Teh and Pete Skidmore...
Elena - 3D printing involves building up an object by stacking up many layers of material rather than carving bits away from a solid block.
Pete - It means that you can make one personalised objects quickly and simply.
Elena - To print an object, a 3D image is first created using computer aided design programmes.
Pete - The programme then creates digital slices of this 3D design with each slice around 0.1 mm thick.
Elena - The printer then converts these digital slices into layers of a printed material usually plastic and builds successive layers on top of each other.
Pete - When plastic is used, it is fed into the printer as long thin strings then heated until it melts then can be printed as a liquid, much like using a hot glue gun to make patterns on a surface.
Elena - The making of the gun printed each plastic component individually and then connected them together. The only metal component was a nail used for firing pin.
Pete - Critics are concern about the production of the gun as the digital design will be made freely available online.
Elena - Some British companies have also warned that the material has not been fully stress tested and could disintegrate from firing.
Peter - Other methods of 3D printing involve using a fine plastic powder which is held together using an ink jet printed glue or using a laser to melt metal powders together to build metallic objects.
Elena - It's not just small objects with 3D printing is becoming useful. It's a low waste method of building structures and some people are even starting to think about printing houses.

11:54 - 3D-Print Your Way to Invisibility
3D-Print Your Way to Invisibility
A "cloaking device", capable of rendering objects invisible to microwave light, has been produced using a standard 3D printer by scientists in America.
3D printing - or Stereolithographic polymer-based fabrication to give it its proper name - 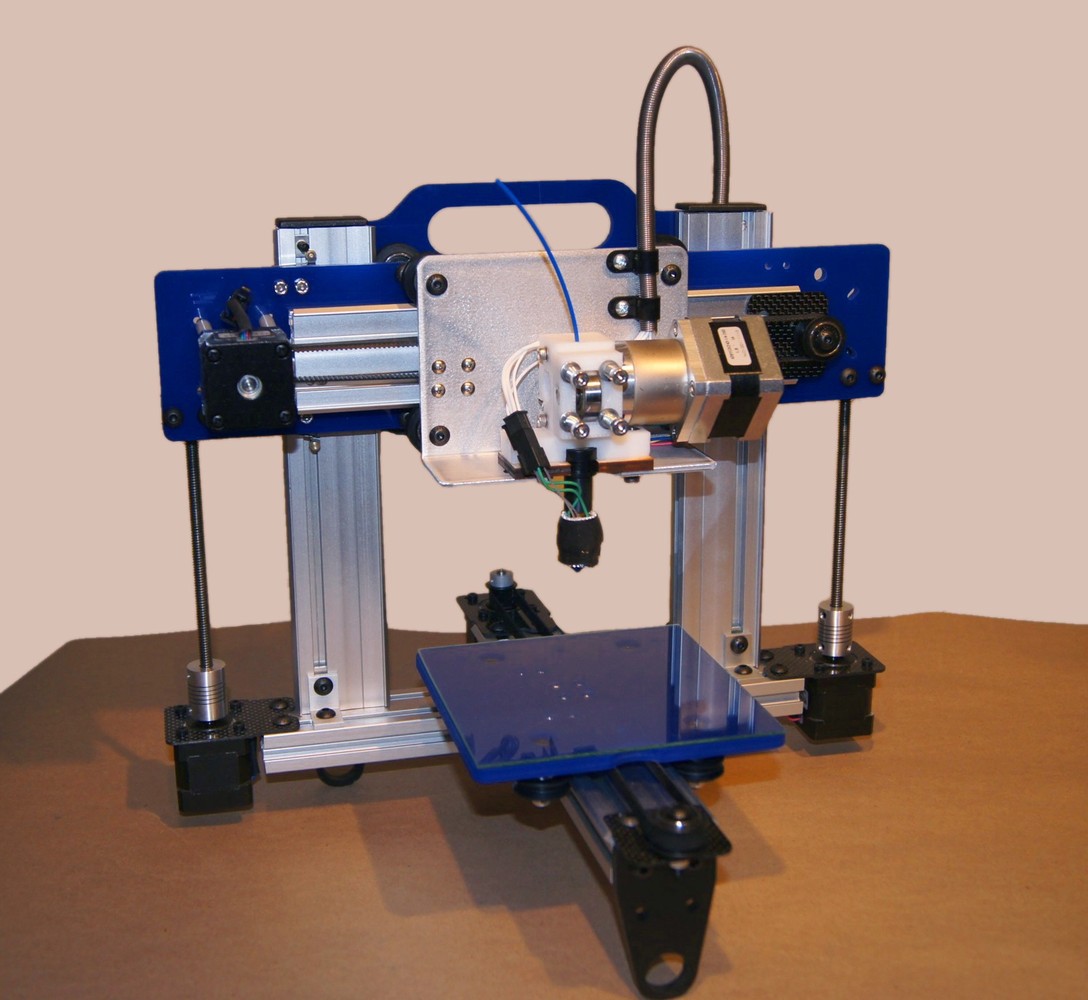 has made headlines numerous times in recent years, from making replacement door handles to providing the template for face transplants. And with companies such as Makerbot already producing high-quality 3D printers for less than £1500, it's easy to think of 3D printing as just a tool for the masses. But a paper in this month's Optics Letters shows that this technology can also have implications for high-end scientific research.
has made headlines numerous times in recent years, from making replacement door handles to providing the template for face transplants. And with companies such as Makerbot already producing high-quality 3D printers for less than £1500, it's easy to think of 3D printing as just a tool for the masses. But a paper in this month's Optics Letters shows that this technology can also have implications for high-end scientific research.
In 2006, a group at Duke University in the US successfully cloaked a non-transparent object - making it electromagnetically undetectable to particular particular wavelengths of light. Within three years, they had produced a working cloak capable of rendering objects surrounded by it invisible to microwaves. Now, a team from the same university have gone one step further.
Led by Yaroslav Urzhumov, the Duke researchers have produced a microwave X-band cloaking device, entirely fabricated using 3D printing. The technique involves laying down thin layers of a material - usually a polymer - by guiding a nozzle in a pre-programmed path, gradually building up a three-dimensional object. Urzhumov's cloaking device resembles a Frisbee with lots of holes, with the object to be cloaked placed inside the large hole at the centre of the disk.
The 3D printed cloak is a transformational optics (TO) material; TOs are carefully structured, with specific holes and grooves that guide and deflect light around the object. An illuminated object can generally be identified in two ways - by the presence of a shadow, or the detection of light scattered from its surface. But, when TO objects, like this 3D cloak, are illuminated by light of a particular wavelength (~3 cm), they don't show either of these properties - TOs can entirely eliminate both reflection (scattering) and shadow, so that the cloak and object combined resemble just empty space.
Previous cloaking devices have used expensive and exotic materials, involved metallic components or have needed to be immersed in liquid to cloak objects from light at particular wavelengths. And in the microwave regime, due to the strict geometry needed to produce TO materials, researchers have been limited to cloaking only small objects.
But using advanced mathematical models, Urzhumov and his team determined the locations, sizes and shapes of the holes needed to deflect microwaves to cloak larger objects. The team then used this data to design and produce a complete shield at a low cost, using standard materials and a 3D printer. The device took seven hours to "print", and because of its novel design could cloak the presence of a metallic cylinder six times wider than the thickness of the cloaking device itself.
In the not-so-distant future, the team say, they will be able to enhance the design of their cloaking devices so that it could work at a wider range of wavelengths - even down to the short wavelengths of visible light. But making objects invisible to the naked eye is no mean feat. The first step is to identify a material that is already transparent to visible light, and use that to build a cloak to conceal things. The second step will be to find a printing technique sufficiently precise to produce the much smaller holes needed to deflect visible light. Urzhumov believes that the answer may lie in nanotechnology, whereby materials can be precisely structured on a small scale. So it may one day be possible to make your own invisibility cloak from the comfort of your Makerspace (or shed).

14:55 - Balloon goes up on Helium prices...
Balloon goes up on Helium prices...
The fate of one of the world's main sources of helium is about to be decided - and prices are set to soar sky high. That could hit universities and hospitals where liquid helium is used to cool superconducting magnets in high-tech equipment such as MRI scanners. Helium is a trace component in natural gas, and extraction at more than a dozen sites around the world feeds a global demand of 170 million m3 each year. But roughly one-third of that comes from a geological stockpile in Amarillo, Texas - the US Federal Helium Reserve - which is slated to close later this year. Without enough production capacity elsewhere in the world to meet current needs, the US Congress is now considering legislation that would keep federal helium flowing for another few years. But even if the reserve does get a new lease of life, its helium would be sold at much higher prices than before. That could hike the average cost of helium by 30% next year, experts say.

18:14 - Environmentally Friendly Steel
Environmentally Friendly Steel
with Prof Derek Fray, Department of Meterials Science and Metallurgy, University of Cambridge
Steel is the most widely used metal in the world. In 2011 alone, around a billion tons of it were produced worldwide. But the steel industry accounts for 5% of the world's carbon dioxide emissions. This week, a team based at the Massachusetts Institute of Technology revealed a more environmentally friendly way of producing it using electricity. To comment on the work, we were joined by Derek Fray who's a metallurgist from Cambridge University.
Chris - First of all, what's the process by which we actually make iron that leads to it producing so much CO2 every year?
Derek - Well, it's reduced by carbon. Carbon is an excellent reductant and it's very, very plentiful. As you know, we're used to burning in our homes to keep the homes warm.
Chris - And we're doing that by chucking carbon into a furnace and the carbon stealing the oxide off of the iron to leave molten iron.
Derek - That's correct. It ends up as CO2 eventually.
Chris - What's the aspiration then to try and get that CO2 down? How could we do it better?
Derek - Well, this team at MIT has discovered a means of electrically reducing iron oxide at very high temperatures, about 1600 centigrade which is more than white heat. So, they simply dissolve it in a liquid solution and electrolyse it.
Chris - Now, what is electrolysis?
Derek - The iron, when it dissolves in the electrolyte as it's called, is known as iron ions and oxygen ions. And when you pass an electric current through the solution, the iron ions will go to the cathode, discharge and form iron and the oxygen ions will go to the anode and form oxygen gas.
Chris - But we do that with aluminium oxide. We make aluminium metal by electrolysing bauxite which is aluminium oxide. So, why can't we just do that for iron?
Derek - Well, the problem is that well, in the aluminium case, you also produce a lot of carbon dioxide because they use a carbon anode. So, the team in MIT, their goal has been to produce an anode which can evolve oxygen on and you get pure oxygen generated. So, there's no CO2 from actual decomposition of the iron oxide.
Chris - So, the problem that they had to grapple with was, what sort of material to use to do that electrolysis, what to use as the electrodes? So, how did they approach that then?
Derek - The approach they adopted was essentially, use stainless steel. Stainless steel is usually iron, chromium and nickel and what they did, they used an alloy which is iron and chromium, plus a few other minor elements.
Chris - So, you mix those two things together. Why don't they just melt when you dunk those materials into molten iron oxide? Why don't they turn into just liquid iron?
Derek - The melting point is higher than the temperature of the electrolyte.
Chris - So, what happens to these electrodes? Why does this work where others have failed then?
Derek - Well, it forms a very tenacious oxide film which doesn't dissolve in electrolytes and it's conducting, so it can pass the electrons to and fro through it.
Chris - What forms an oxide layer? Just talk me through what's going on in this electrolysis then?
Derek - When you put the iron chromium alloy into the electrolytes, it oxidises a little bit, you get a very, very thin layer which is very stable. So, it doesn't dissolve.
Chris - So, that forms on the surface of the electrodes and this protects the electrodes from the environment they're in. So, what does this mean in terms of how we would actually deploy this?
Derek - It would be very similar to the whole Heroult cell for the reduction of aluminium. We would have a liquid metal pool, you'd have the electrolyte floating on the top, and then your anode would be above that. So, when the oxygen forms on the anode, it just escapes.
Chris - Could you do this in a batch process or would you have to chuck a whole out of the oxide in and then run the electricity through it, and reduce it to metallic iron then pour that off and start again or could you continuously add little bits of iron oxide and keep the process going all the time?
Derek - Well, if you go back to the whole Heroult cell, essentially, that's a batch process. The aluminium is taken out about every 8 hours and you feed the alumina in about every 8 hours as well.
Chris - If we actually do this, why is this better than doing it the traditional way with carbon because the electricity is presumably going to have a carbon cost attached to it?
Derek - I think the assumption would be, the electricity would come from photovoltaics or wind power or sea power, or tidal power. Obviously, if you're having to use electricity from a coal fired power station, you're no better off.
Chris - Does the discovery of this new material actually mean something in terms of how we could use it in other areas though? It's not just for iron. Could it be used elsewhere?
Derek - You could use it for other metals.
Chris - What about the fact that it also makes this oxygen? Is that useful?
Derek - Probably not on the earth, but it would be in the Solar System or on the moon, the rockets that took the astronauts to the moon 20 or 30 years ago. They were mainly oxygen. You need about 80 tons of oxygen, about 10 tons of hydrogen for the power. So, if you obviously hope to bring the astronauts back, you have to take enough oxygen up there. And if you could generate the oxygen on the moon, it would be very much easier.
Chris - So, in other words, if we could take moon rock and use this sort of technology, these sorts of electrodes and electrolyse moon rock, it would be very nice because we could get all the metals out as well which could be good for construction.
Derek - Could be used for structural things, yes.
Chris - Plus, we would then get a supply of oxygen to send people off another journeys or even bring them home which is surely nice.
Derek - The advantage of the moon is that gravitational field is 1/6 of that on the Earth. So, you need less power to escape the gravitational field.
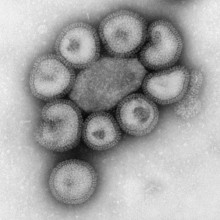
23:57 - The Evolution of a New Flu Outbreak
The Evolution of a New Flu Outbreak
with Dr Colin Russell, Deptartment of Zoology, University of Cambridge
In March, a brand new strain of the influenza or flu virus called H7N9 was detected in China. In the month since its detection, 100 people have been infected and 1/5 of those have died. We were joined in the studio by Dr. Colin Russell from the Department of Zoology at the University of Cambridge who's an expert on how viruses like H7N9 can evolve to become serious threats.
Kat - Now, just explain, what is H7N9 and why is it different from previous flu strains?
Colin - So, H7N9 is an influenza A virus that is not fundamentally dissimilar to the H5N1 virus or the bird flu virus that we've been so concerned about over the last 15 years. Now, H7N9 is of particular concern because it's something that we haven't seen infect humans before and prior to March, we hadn't seen this virus in any humans ever. Now, since that time, we've seen 130 humans infected with the virus and of those, approximately 20% of them have died. And so, in these particular circumstances where we have a new influenza virus emerging in the human population, it is of course a serious concern.
Kat - I'm sure all of us know about the massive flu pandemics. Before we come to talk about some of the scary stuff, I just had a question. Why are these flu viruses called H-something, N-something? What do those letters designate?
Colin - Well, all influenza A viruses are called H-something, N-something because influenza viruses are characterised by the proteins that are on the surface of the virus.
So, there are two proteins on the surface of the virus. There's the hemagglutinin protein which gives us the H and the neuraminidase protein which gives us the N. There are 16 known hemagglutinins in birds and 9 known neuraminidases which can give us a tremendous number of combinations of viruses that could cause infections in humans.
But so far, we've only seen H1N1, H2N2, and H3N2 cause pandemics in 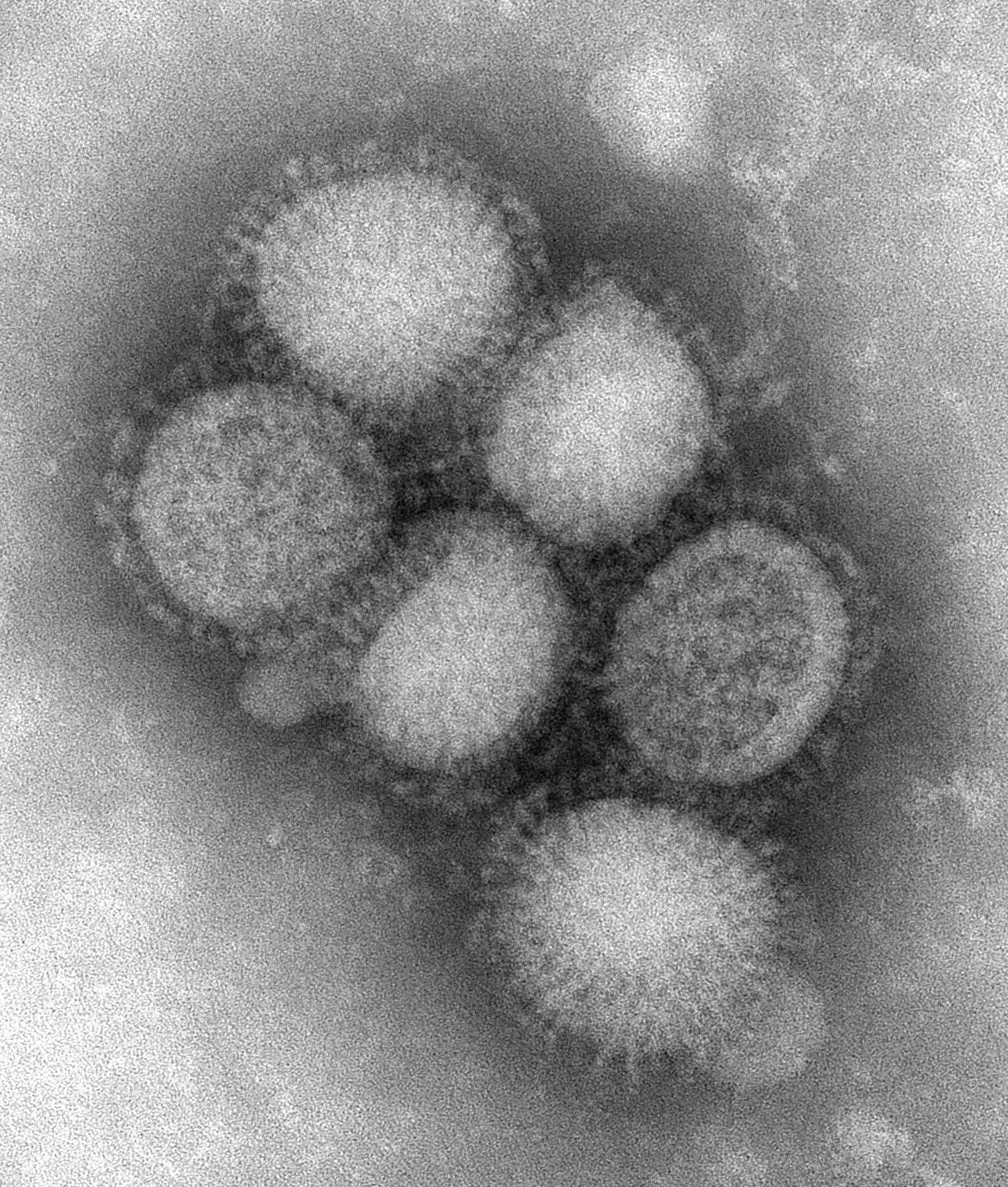 humans. So, the fact that we now have an H7N9 virus causing infections is something new. Now along these lines, we've also seen H5N1 viruses infect humans too, but we've never seen massive human to human spread of any of these viruses other than the H1N1, H2N2, and H3N2 viruses.
humans. So, the fact that we now have an H7N9 virus causing infections is something new. Now along these lines, we've also seen H5N1 viruses infect humans too, but we've never seen massive human to human spread of any of these viruses other than the H1N1, H2N2, and H3N2 viruses.
Kat - So, this new H7N9, why does it seem to have such a high mortality rate? Why does it kill proportionally more people than some of the other flus?
Colin - Well, as compared to the known cases for H5N1 (bird flu), this H7N9 virus is comparatively less lethal. So, for H5N1, there has been about 600 known cases so far and approximately 50% of those cases have resulted in mortality. Now, in the case of H7N9, we have a situation where we've seen about 130 cases to date and about 20% of those have died. But we don't know that there aren't cases that we don't know about. So, in this particular case, we could just be seeing the tip of the iceberg.
Kat - Where did this virus actually come from because it's originated in birds as bird flu did as well? Where do we think it started and what created it?
Colin - Well, this is a good question and it's one at the tip of everyone's tongue right now because we don't really know where this virus came from. Now, there are some things that we've managed to learn about the virus from analysing its genetic sequences.
So, myself and many others have looked at the genetic sequences of these viruses and we found that these viruses were actually the product of three different influenza viruses. So, influenza viruses, their genes are each coded by individual segments of RNA and they have 8 genes in total. So, the H gene, the hemagglutinin, and the N gene, the neuraminidase account for just 2 of those 8 genes. Now, we know that the H gene came from an H7 virus and that the N gene came from an N9 virus.
But interestingly, the internal proteins, these are the ones that aren't on the surface of the virus, all appeared to have come from an H9N2 virus. Now interestingly, when we look at the genetic relationships among these viruses, we see that the internal proteins, those that came from this H9N2 virus, all are most closely related to viruses that either came from wild birds or from poultry, in the areas around where the original cases emerged. So, we have a good sense in this particular case that we have at least seen the geographic region where the earliest cases have emerged.
Kat - So, there's been some kind of genetic mix and match going on in a bird to make this new virus. So then it sort of spread in birds I guess. How does it get from birds into humans?
Colin - Now, that's a good question as well. So, for influenza viruses, there's a particular term for this. It's called re-assortment because the influenza genes are on each on different segments. The viruses, if they co-infect a host, the genes can get all mixed up or re-assort.
Kat - So mix and match basically.
Colin - Exactly. But in the context of how it gets into humans, in the case of this particular virus, we don't really know where it's coming from. I mean, we certainly suspect that it's coming from birds, but we don't really know.
Now, for H5N1, we have a much better picture of how humans typically get infected and the majority of individuals who've been infected with H5N1 over the last 15 years have been in close proximity to either fowl or domestic poultry. So, there's a particular story that I like which involves - it depends on who you hear the story from - a Thai duck farmer and this Thai duck farmer lives in his home with his ducks and he has a duck that has flu-like symptoms because frequently, when birds get highly pathogenic, avian influenza viruses, they have the same sort of symptoms that humans have. They cough, they sneeze, they have a runny nose.
Kat - They sit in front of the telly all day and feel terrible.
Colin - Well, if you've got a telly and your duck likes it, there's no reason not to watch it. But basically, this farmer, he sees his duck is suffering and this just isn't agreeable to him and he really wants to help. And of course, you can give a duck a tissue, but you can't make it blow its nose. And so, he decides that he's going to help and he does the only thing he can think of which is, he puts the bird's beak in his mouth and he blows.
Kat - Oh, no!
Colin - Now, this of course causes an evacuation of the bird's nostrils directly into the man's eyes. Now, one of the things that's really interesting about this particular case is that one of the primary reasons that we don't see bird viruses crossing in humans all the time is that bird viruses have a different cell surface receptor that they bind to, apart from what normal human influenza viruses bind to. But interestingly, we have those bird influenza receptors in our lower lungs and in our eyes.
Kat - Oh, my God! So, you basically have to get bird snot into your eyes.
Colin - Well, bird's snot into your eyes would be one way to do it, but otherwise, you need to get the virus deep into your lungs which is not a trivial thing to do.
Kat - You have to be breathing in bird snot basically.
Colin - Or definitely have a very close contact with birds indeed.
Kat - But about this new H7N9, do we know if it can transfer between humans and we know it can go from birds to humans, but what about from human to human because that's when stuff gets really scary?
Colin - Well, that's when it becomes of increasing concern. Right now, there are no known cases of human to human transmission and the Chinese government is doing an extreme amount of work in order to trace all of the contacts of the individuals who have been in close proximity with individuals who have tested positive for the H7N9 virus. And so far, none of these secondary contacts have tested positive for an H7N9 infection which suggests that we haven't seen human to human transmission yet. But that only involves the cases that we know have been - well, that have shown up in hospital.
Kat - So, there may be people out there with it that are just sick and haven't been kind of ticked off on the, "Oh, you've got that." I mean, should we be worried about this, now that we've identified it and we seem to have identified a group of people that have it as a general population and obviously we're in the UK and not in China - Should we be really worried about this or not too worried?
Colin - Well, there's two causes for concern. So one, anytime where we see a new influenza virus that is infecting more than a handful of people, it's a cause for concern because of course in the past, influenza viruses that have crossed from animals into humans have caused pandemics. Now in this particular case, we've seen a fair number of human cases in a relatively short period of time. So of course, that is a cause for concern. Now another cause for concern is that these viruses appear to have mutations that at least in the case of H5N1, could lead to easier transmissibility between humans. Now, that said, we still haven't seen human to human transmission yet, but because these viruses have some of these mutations, there is cause for concern that it might be easier for these viruses to evolve to become transmissible than other influenza viruses that we've seen crossing into humans in the past.
33:48 - Mapping Infectious Diseases
Mapping Infectious Diseases
with Dr Tom Koch, University of British Columbia; David Pigott, University of Oxford
Chris - Today, quick transport links between cities mean emerging infections can spread globally and very rapidly. So scientists need a way of following the course of the disease and Pete Skidmore has been finding out how medical mapping provides an insight into the dynamics of disease spread.
Pete - Plotting the spread of disease onto maps is an essential tool for 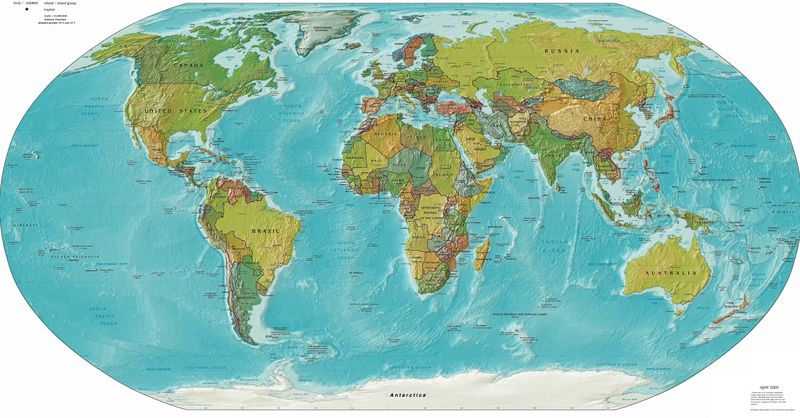 government and health organisations trying to stem the tide of epidemics because it allows them to plan more resources such as vaccines and sanitation. To find out more, I spoke to Dr. Tom Koch, a medical geographer from the University of British Columbia in Canada.
government and health organisations trying to stem the tide of epidemics because it allows them to plan more resources such as vaccines and sanitation. To find out more, I spoke to Dr. Tom Koch, a medical geographer from the University of British Columbia in Canada.
Tom - Medical mapping as a consistent tool in the study of public diseases began in 1796 with the study of yellow fever. It is the way in which we take a collection of events and then we plant them into a specific geography where we can have the relation between the occurrence and environment that either promotes or inhibits it.
Pete - Thinking about the modern world now, obviously, there's a lot more mobility between cities. There's a lot of figures going around that no city is 24 hours away from any other city. Is there any way that we can adapt to cope with the different epidemiological factors with our much more mobile society?
Tom - Globalisation really is just a speeded-up version of the mercantilism and then the industrialism which has long been in place. But it was really the Crusades, the travel between cities, which brought us the plague in the 14th century. It was globalisation and trade and it was the passage of people from one country to another which brought us cholera in the 19th century. So, the first thing to recognise is this is nothing new. It might have been speeded up some, but it's a difference of degree and not kind. What the rapidity of travel means is that it will be even harder despite all of our advances in technology to stop either the evolution of our microbial friends or the progression of the disease that they eventually hit upon.
Pete - Infections may be able to spread across the world more quickly now than in any other time in history, but surely, with the advances in global communication and social media, it's easy to track epidemics. I spoke to David Pigott, a DPhil student at the University of Oxford, who studies the different ways we build disease maps.
 David - We believe systems such as HealthMap and BioCaster, GenBank and potentially social media can help. HealthMap and BioCaster are websites that use data mining algorithms to trawl the web looking for non-conventional data sources. So, they look at news articles, other websites that wouldn't ordinarily come up if you're using a standard academic literature based search engine. And combined, they're bringing up about 400 new posts everyday pertaining to different diseases. And then finally, Twitter and social media at the minute represents an uncertain but very promising route nonetheless where we can use the tweets if they're relating to a disease, for instance. That would be the hardest task, trying to identify what key words are critical for which disease and trying to use information from that. But Twitter is a very noisy system when it comes to disease reporting. Previously, people have identified that Twitter trends for influenza and dengue predict trends in case reports from conventional systems like the CDC in America by up to 2 or 3 weeks before. So, it has the potential to help, but we need to do a lot of work to determine the accuracy of those data points.
David - We believe systems such as HealthMap and BioCaster, GenBank and potentially social media can help. HealthMap and BioCaster are websites that use data mining algorithms to trawl the web looking for non-conventional data sources. So, they look at news articles, other websites that wouldn't ordinarily come up if you're using a standard academic literature based search engine. And combined, they're bringing up about 400 new posts everyday pertaining to different diseases. And then finally, Twitter and social media at the minute represents an uncertain but very promising route nonetheless where we can use the tweets if they're relating to a disease, for instance. That would be the hardest task, trying to identify what key words are critical for which disease and trying to use information from that. But Twitter is a very noisy system when it comes to disease reporting. Previously, people have identified that Twitter trends for influenza and dengue predict trends in case reports from conventional systems like the CDC in America by up to 2 or 3 weeks before. So, it has the potential to help, but we need to do a lot of work to determine the accuracy of those data points.
Pete - So, you mentioned BioCaster and HealthMap. Have these at all helped in the recent epidemics like H7N9 and SARS-like corona virus?
Tom - HealthMap and BioCaster have been used in maps particularly just picking up news reporting in China since but yeah, given there's a lag time between case reporting and national health service reporting level, it's the hope that HealthMap and BioCaster could try and reduce that lag in delay especially when it comes to a very novel infection where actually, it's the speed of information gathered that's the most important aspect.
Pete - So, where will the next pandemic come from? Tom Koch has the answers.
Tom - We know that the next pandemic is almost a certainty, I would say, within 10 years and it will start as pandemics always do, in a type of area which is densely settled, where there's huge social and economic inequality such that there will be a dense group of people living in poor surroundings often with their animals and then it will spread from there to a primary city and from there to other primary cities. So, it may be that it starts in China or Vietnam, a place where we have huge densities and huge income inequality and then it will spread with travellers first in a local area where the virus or bacteria gets set and then it will grab an airplane and fly on off.
Pete - And is mapping prepared for that?
Tom - Sure! As the data comes in, we can map it and we can very quickly predict, depending on the nature of the specific microbe, its rate of diffusion to primary and secondary sources. We know how to do that. More important is, can we, and why are we not, identifying the places where the disease is likely to come, and putting our international energy into the type of development which will limit the opportunity for the virus and bacteria to proliferate, mutate, and then spread.
Kat - So, new diseases are constantly emerging, but hopefully, new methods of mapping them will allow us to stop them in their tracks.
40:13 - Tackling Drug Resistant Tuberculosis
Tackling Drug Resistant Tuberculosis
with Dr Sani Aliyu, Addenbrooke’s Hospital, Professor Dean Felsher, Stanford School of Medicine
 Chris - We've been hearing a lot about new infections, but sometimes old enemies come back to haunt us. Tuberculosis, TB, is a disease which many of us think of as a thing of the past, but now, it's back on the rise in the UK and elsewhere in the western world. Part of that might be down to the recent discovery that TB can conceal itself in cells in our bone marrow, even in people who've ostensibly been cured of the infection.
Chris - We've been hearing a lot about new infections, but sometimes old enemies come back to haunt us. Tuberculosis, TB, is a disease which many of us think of as a thing of the past, but now, it's back on the rise in the UK and elsewhere in the western world. Part of that might be down to the recent discovery that TB can conceal itself in cells in our bone marrow, even in people who've ostensibly been cured of the infection.
We'll hear more about that in just a minute from Stanford physician Dean Felsher, but first, consultant microbiologist Sani Aliyu is with us to talk about other emerging threat from TB which is that the bug is rapidly becoming resistant to the majority of the antibiotics that we use to treat it. So, Sani first of all, what actually is TB and why is it such a problem?
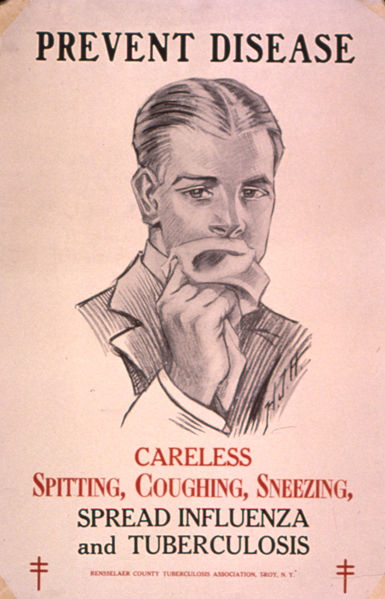
Sani - So, TB refers to tuberculosis. It's been with us for quite a while. It's an infection caused by a bacteria called Mycobacterium tuberculosis. It usually manifests with cough, respiratory symptoms, fever, night sweats and could affect any organ in the body really but mostly, the lungs.
Chris - How do people catch it in the first place?
Sani - Transmission is usually called airborne, simply because when you cough or when you sneeze, or you talk, you have droplets that contain the bacteria. And the droplets can survive in the environment for prolonged periods of time. They tend to be suspended and if you inhale the droplets, the bacteria goes into your lungs and then you get infection. By inhaling the bacteria, you don't necessarily get active disease. You can get latent disease because it's estimated worldwide that 1 in 3 people are infected with TB, so it's very common.
Chris - When you say latent disease, what is actually going on? So, you've been infected but you don't have TB actively growing in you. Is that what you're saying?
Sani - That's right. So, you've been infected with the bacterium that's sitting dormant or latent in your body cells and it's hidden. It may not necessarily come up and cause symptoms. It's only when you have symptoms, that you have tuberculosis disease. The most cases of active TB arise from the latent form where you have the bacteria replicating and then it causes symptoms, usually, in relation to immunosuppression or old age.
Chris - What does it do in the body? Does it just cause chest disease problems or does it go elsewhere too?
Sani - TB can affect virtually any organ in the body. Severe tuberculosis for instance can affect the brain, can affect the meninges, so it can have meningitis. It can affect the bones. In the past, what we call Pott's disease where you have people with infection involving the spine, has been well-described. You can also have genitourinary tuberculosis, abdominal TB.
Chris - Now, when people talk about drug-resistant TB, first of all, how do you actually treat normal TB? What's the regimen?
Sani - The first drug that was produced and that was found to be quite effective for TB was streptomycin in 1944 and since the '60s where rifampicin came in, TB has been treated with a cocktail of at least 4 drugs. They're called first line drugs. So here in the UK for instance, we have rifampicin and isoniazid which are considered the core and most powerful anti-TB drugs available. Then you have pyrazinamide and ethambutol. You could also have injectables.
Chris - And you give those for quite a long period of time don't you?
Sani - That's right. For pulmonary disease, you give the cocktail of drugs for a total of 6 months.
Chris - And what's the reason why TB is now no longer responding reliably to that cocktail of drugs?
Sani - So, a combination of factors really. What's been happening for the last 20 years is we have a large cohort of people especially in the middle and low income countries where you have TB that's not really being treated properly. You have both misuse and mismanagement of the drugs. If you have patients with tuberculosis taking the drugs in a way that they're not supposed to, either taking one pill or taking an inadequate dose, or taking for a very short period of time, you tend to develop that resistance simply because you have that drug pressure which pushes the bacteria to develop mutations.
Chris - And so, what is the status of TB response to our medication now? How many cases of TB would we regard as resistant?
Sani - So, worldwide, we have what we call multi-drug resistant TB which essentially is resistance against the two core drugs rifampicin and isoniazid. It's estimated by the WHO that there are probably about 65,000 cases of multi-drug resistant TB, mostly in high incidence countries such as Sub-Saharan Africa, the Indian subcontinent and central Europe.
Chris - And what about the more resistant form, the XDR-TB that we're now beginning to hear about extensively drug-resistant TB? How does that differ?
Sani - So, extensively drug-resistant TB is really a progression of MDR-TB. In other words, in addition to resistance to rifampicin and isoniazid, you also have resistance to a class of antibiotics called the quinolones and to at least one injectable antibiotic. And what this confers is really a difficulty in managing the TB. You have to give a cocktail of drugs that are usually second or third line drugs that aren't as effective as the first line drugs. You have to give them for a longer period of time, they're much more toxic, they're more expensive and it's a nightmare really.
Chris - And how common is that form of TB?
Sani - Fortunately, in the UK, pretty rare. In 2011, this is based on information from the Public Health England website, more recently called the HPA, there are about 81 cases of multidrug-resistant TB up to the end of 2011, but only about 24 cases of XDR-TB in total, of which 6 were confirmed in 2011. So, it's a pretty rare disease fortunately in the UK.
Chris - But it's not 0 is it, which means we need to keep an eye on that. Thank you, Sani.
And Dean Felsher, now you've recently shown that TB can hide away inside the body and remain in a viable state even in people who have been what we would regard as cured.
Dean - Right. So, what we found was that tuberculosis can hide in a very unexpected site. It can hide in a rare population of bone marrow stem cells that have the special name, the mesenchymal stem cells. And they have multiple biologic properties that make them a perfect place for tuberculosis to hide away. They like to migrate around the body. They're naturally drug-resistant. They're naturally resistant to the immune system. They can tolerate living in a low-oxygen state which is typical of places where tuberculosis infects. So, in many ways, they represent a sort of perfect host cell. It's been known for a long time that tuberculosis can hide in other normal cells in the human body, but this population of bone marrow stem cells is rather surprising finding that we reported recently.
Chris - How did you discover that TB was lurking in those cells?
Dean - So, our work has very much been interested in the role of stem cell and stem cell kind of biology in disease processes and there was a very creative idea that tuberculosis maybe taking advantage of a normal stem cell population. And I decided to pursue this by studying whether or not tuberculosis could live in normal human stem cells and we were able to show that indeed they could preferentially infect and become dormant in these normal human stem cells and then we're even able to show evidence that this was true in human patients.
Chris - Now first of all, talk us through how you think TB gets to those stem cells in someone who gets infected via the lung or breathes in some TB, and then what happens to the TB once it's in the stem cell?
Dean - It's known that tuberculosis will form a structure that we call a tuberculosis granuloma and other scientists had reported that some of the body's stem cells like to migrate to the granuloma. And what we think happened is, that these special type of bone marrow mesenchymal stem cells are attracted to the site of infection and that tuberculosis has figured out a way to get into these cells and then use them as a way to escape the normal sorts of mechanisms that the host immune system is trying to use to get rid of the tuberculosis.
Chris - So, those cells get infected in that site in the lung and then they go back to the bone marrow, do they?
Dean - They can go back to the bone marrow because they're capable to migrate as well as go to other sites.
Chris - And how did you know that once the TB is in those cells that it's actually viable and that it remains in a viable state so it can come back to life from within those cells later?
Dean - Yeah, we were able to take from patients who have been treated extensively in a way that you would expect they were cured of tuberculosis, people we knew had tuberculosis, take their bone marrow out using a special procedure that we use as haematologists called a bone marrow biopsy and purify this subpopulation of bone marrow stem cells and show that we cannot only detect the DNA of tuberculosis, but we could actually recover viable tuberculosis using microbiological assays in the laboratory.
Chris - So, these are people who've had drugs that have cleared them of signs of being infected with TB, they would be regarded as cured, but actually, you can get stem cells out of their bone marrow and there's a viable TB living in there?
Dean - Exactly.
Chris - So, what are the implications of that?
Dean - Well, the implication is that it may be that if we can figure out a way to get rid of tuberculosis from these bone marrow stem cells, we might be able to come up with a better long term treatment for tuberculosis.
Chris - Let's hope so. Sani says, with one person in three carrying it, we need to move fast, don't we? Thank you very much to Dean Felsher from Stanford School of Medicine and also before him, Dr. Sani Aliyu who is from Addenbrooke's Hospital is Cambridge.

50:39 - Are city dwellers more immune to bugs?
Are city dwellers more immune to bugs?
Eleanor - So in principle, yes. People living in small isolated communities may experience a more limited number in diversity of infections and they can lack immunity to diseases which are actually quite common place in other environments. Some classical examples are those with epidemics of diseases such as measles and smallpox in small Amazonian communities when they first came into contact with outsiders. But these days, human populations are so mobile that actually, very few of these really isolated populations persist and you're as likely to contract the latest strain of flu whether you live in a huge city or in a smaller town or village nearby. And that's because people move around between these communities on such a regular basis that they move the virus around with them and we only have to look at how quickly the swine flu epidemic in 2009 reached almost every country in the world, including countries with really low population densities. And we can see from that that actually, from the perspective of the bug, we all now live in a single global community our immune resistance will reflect the fact that we are all exposed to very large numbers of infections.
Hannah - So, with frequent global travel, there's no rationale for rushing to live in the city since it won't boost our immune systems. However, pollution and stress from the city have both been linked with weakened immunity. Plus, there are studies that show that people who grow up in cities process stress differently and have an increased risk of getting mental health disorders such as Schizophrenia.










Comments
Add a comment