Sepsis: From Infection To AI
In recognition of World Sepsis Day on the 13th, we’re unpicking the science of this dangerous syndrome - from the infections that cause it, to the genes that make us more susceptible, and how artificial intelligence can help us to crack it... Plus, in the news, sending hydrogen to houses through the gas network to cut our carbon footprint. How a high fat diet could be disrupting your sleep; and the Ig Nobel prizes - for science that “makes people laugh, then think” - are announced. We’ll hear who’s won what...
In this episode

01:07 - Mixing hydrogen and natural gas to heat homes
Mixing hydrogen and natural gas to heat homes
Angie Needle, Cadent Gas
The world needs to leave most of its coal, oil and gas in the ground between now and 2050, if we’re to stand any chance of keeping climate change to within a 1.5 degrees Celsius level of average warming. And that includes the UK. But according to a 2021 survey by the UK Department for Business Energy & Industrial Strategy, 77% of respondents said they use gas central heating. How do we cut our carbon footprint while not leaving three quarters of the country out in the cold? One answer might be to send something different down the pipelines: hydrogen. When this burns, it releases only water as a waste product. As a first step, if we replaced some of the natural gas - or methane - with hydrogen, assuming that people’s appliances worked satisfactorily, we could cut the carbon footprint of the process without having to change anything else. One company has tried this recently - in a small scale way - with Keele University and they announced the results this week, as Angie Needle explained to Chris Smith...
Angie - I'm Dr. Angie Needle. I'm the Strategy Director at Cadent. Cadent is a gas network provider, so we deliver natural gas to 11 million homes and businesses across the UK in those yellow pipes that you see. In this instance, we were exploring how we can introduce a proportion of hydrogen into the existing natural gas network, so that we can reduce the carbon emissions of the energy that's used in people's homes.
Chris - Why can't we just put hydrogen down those pipes rather than natural gas? Because if one looks back in history - before we were using natural gas, we were using town gas, or coal gas, and that contained a lot of hydrogen. So were we not already kind of familiar with how this works anyway?
Angie - Yeah, I would agree that that is true. Town gas had up to 50% hydrogen in it. The bits of our gas network will have seen this before, but it's the end-user appliances - the boilers and the cookers and the fires - that haven't. And so what we want to be sure of is that when we start introducing hydrogen and people are using a lower carbon gas, that the experience in the home is exactly the same. And that's what this project is looking at - making sure that when we introduce small amounts of hydrogen, it makes no difference to the appliances and they can continue as normal.
Chris - Where did you do it?
Angie - So Keele University has got its own gas network - it owns it itself. And so we got together with Keele on their campus, which has about 100 domestic buildings of all different shapes and sizes, some which lecturers and whatnot live in, and some which are privately owned, and about 30 University buildings. And so we built a compound there - we made the hydrogen on the site - and we blended it through what we call a Grid Entry Unit, a new piece of kit, into their gas network. This had never been done before and was massively successful, because nobody knew any different. The consumer experience was - "We didn't even know this was happening. We couldn't see any changes."
Chris - How much hydrogen were you adding to the gas supply?
Angie - We added up to 20%, and that's quite important because most of the cookers and fires and things that are out there today can take up to about 23% in the way that they're built and tested. 20% allows about a 7% carbon emission saving.
Chris - And is it easy to do this hydrogen admixture? To put it into the gas supply?
Angie - Largely all we do is to take a bit of the gas out - the natural gas - blend in the hydrogen, make sure it's mixed up really well, and put it back into the gas. The main challenge is actually having enough hydrogen and making sure we can have low carbon hydrogen to put into the gas network. But the first-of-their-kind equipment that we developed, we can see that you can scale and replicate quite easily. So you can start putting in hydrogen at different places in our gas network.
Chris - In practical terms, were we to start doing this across the country, how much energy is actually being provided by the same volume of gas? Is hydrogen as energy dense as natural gas? In other words, are people going to have to burn more of it to get the same bang for their buck?
Angie - Hydrogen has actually got a huge amount of energy content in it, but it takes up quite a lot of space. It's quite a light molecule. So what happens is that 20% hydrogen by volume is actually only 7% by energy. We're working at the moment to make sure that the existing pressures that are on our pipes can take the extra flow, if you like, of hydrogen. So you need to use a bit more hydrogen to get to the same calories, or energy, as you get today with methane, but the most important thing is hydrogen doesn't produce any carbon dioxide.
Chris - So you would regard the present situation then as a stepping stone towards the full-on 100% hydrogen energy economy?
Angie - In parts, yes, a 20% blend helps us get the infrastructure and the hydrogen production going. We need lots of hydrogen to get to net zero, almost regardless of what it's used for, and in the UK we don't make much today, so we need to get production going. But I think there will ultimately be a blend of different uses of energy in the future - renewable electricity and hydrogen. And regarding consumers, we need to help them understand whether their home is suitable for electric solutions or whether it's suitable for hydrogen, so that there is choice. Choice is good, because if we put all our eggs in the same basket when it comes to energy, we tend to find that each one has limitations that need the other to balance it out. So I'm very much supportive of having choice, but also that we help consumers make that choice.

07:10 - Limiting fossil fuel exploration
Limiting fossil fuel exploration
Dan Welsby, University College London
According to a paper in the journal Nature this week, the world needs to leave a substantial part of its fossil fuel reserves in the ground, if we’re to stand any chance of curtailing the worst impacts of climate change. In 2015 researchers at UCL estimated these limits. Now, Daniel Welsby is back and he’s taken advantage of more recent research and energy consumption trends to improve on that previous study. Harry Lewis asked him what the figures show...
Dan - 60% of global oil and gas reserves and 90% of global coal reserves need to remain in the ground. In comparison to the 2015 paper, that's nearly a doubling of oil reserves that need to remain in the ground.
Harry - Globally, right now, what does our fuel consumption or production look like? Is it on the rise or is it on the decline?
Dan - It's very regional dependent. For example, in Europe and in the United States, we've seen quite considerable scale back in terms of our consumption of coal, but then that's been almost entirely offset by consumption increases in China and India and other parts of developing Asia. There is no indication from fossil fuel producers to scale back production on anything like the scale that we've suggested. And IEA's net zero report suggests that those trajectories are going up when we need to be going down.
Harry - And your model predicts how much fossil fuel a region of the globe can actually extract from its own reserves. So for some of the big hitters out there, like the US say, what changes in production behaviour do we need to see according to your model?
Dan - Actually the US's average annual decline rate for gas production is 8%, which is a very, very quick decline.
Harry - That's what's needed?
Dan - Yeah, that's what's required.
Harry - What about for the rest of the globe?
Dan - I think probably for oil and for coal, generally, we see the vast majority of regions have reached peak production in 2020. I think probably where this really came through in the modelling was for gas. For example, we saw an average of an 8% decline in US gas production, and in Europe, it's about 7%. That's then offset until 2030 by production increases in places like the Middle East. So, actually, globally between 2020 and 2030, we do have a bit of a plateau, but that's highly dependent on things like, if one region is adding a unit to the global supply, then another region has to do much more than that to ensure that the decline pathway is maintained.
Harry - Sure. And if we do make the suggested cuts and we do keep this amount of fossil fuel in the ground, it's not 100% guaranteed we prevent ourselves from reaching that 1.5 degree Marc up in the climate, is it?
Dan - Absolutely.
Harry - It feels like this is a big ask. It feels like it's too late to stop this stuff from leaving the ground.
Dan - A lot of this is down to political will. We don't really have any time to take another five years discussing reversals of production and things, but hopefully what will happen at COP is that there will be a kind of movement towards a degree of transparency in terms of who is producing different oil, gas and coal assets, how much is out there, and trying to develop mechanisms whereby global production is declining. But then really one of the main messages from this work is that those really heavily dependent regions like the Middle East for oil - they're going to have to start to diversify their economies. And there does seem to be some movement on that. I'm not sure it's looking particularly rosy at the moment in terms of plans and projects to come online as well.
Harry - What are governments putting in place to try and reduce fossil fuels? Because surely that's the one main thing we can do?
Dan - Absolutely. There are shoots of activity - the banning of new petrol and diesel cars or internal combustion engines in the United Kingdom was announced and DenMarc has refused any new exploration licenses for oil and gas. This needs to be taken to another, I'd say, good few levels.
Harry - What do those, in your opinion, good few levels resemble? What do they look like?
Dan - In the future, it's some form of carbon pricing, which is in place in some regions at the moment, but needs to be expanded globally and kind of ramped up in their incidence.

12:58 - Ig Nobel Prizes 2021
Ig Nobel Prizes 2021
Marc Abrahams, Improbable Research
One of the most eagerly awaited dates on the scientific calendar has just arrived with the announcement of the winners of this year's ignobel prizes. Every year, some of the most unusual scientific studies - that famously make people laugh, but then stop and think - win this great honour. Chris Smith spoke with Marc Abrahams who founded the Ig Nobel Prizes and oversees the ceremony to talk through this year’s crop of the cream of scientific endeavour...
Marc - These are prizes for something unusual. So they may strike you as being important or completely worthless or whatever, but there's more to them than you expect. We've been doing this, as you point out, for 31 years now
Chris - When you set them up, did you think you'd be having a conversation with me 31 years later, or at least anyone, about this initiative?
Marc - I believe I did not have that very specific wish, but generally we hope that it will continue for a long time. We've been very happy to see that it has been, and we hope will be, continuing for quite a while
Chris - You came to Cambridge once and did a presentation during the Cambridge Science Festival on this and made everyone roar with laughter, but when you normally run them you normally do this on stage and people come to visit you for them. Obviously that hasn't happened because of the pandemic, has it?
Marc - Normally this happens at Harvard University here in the US inside the biggest theatre there, so there are 1100 people jammed into the audience and winners come - 10 winners a year - from around the World. We have a bunch of Nobel Prize winners there to shake their hands, and everybody's throwing paper aeroplanes at each other for an hour and a half. But yes, we couldn't do that because of the pandemic. So last year, and again this year, we've done the whole thing online, which is much more complicated, at least in a different way
Chris - What sorts of entries have you considered though? Because obviously that hasn't changed - people are still doing fantastic science around the World, despite the best efforts of coronavirus to thwart science
Marc - Yeah, we still get many thousands of new nominations every year. Let me just dive into a few of this year's. One of them was the Biology Prize, which went to a team in Sweden - Susanne Schötz and her colleagues. They analysed variations in purring, chirping, chattering, trilling, tweedling, murmuring, meowing, moaning, squeaking, hissing, yowling, growling and other modes of cat-human communication
Chris - I think we've actually got a clip of that one. Let's have a listen to her. This is her actually doing the cat noises...
<CAT NOISES>
Chris - I bet she's great fun at dinner parties
Marc - Yes, I bet you're right about that
Chris - The other one that caught my eye this year, as a microbiologist with an interest in all things microbes, was this paper on people looking at what's living in chewing gum. I love that
Marc - Yeah, this is a team in Valencia, Spain, that analysed chewing gum that they took off pavements in many different countries and they analysed what kinds of bacteria are living in those wads of chewing gum
Chris - And what did they conclude?
Marc - It's different. And also that if the gum has been there on the sidewalk for quite a while, if somebody goes and very carefully analyses that hunk of chewed chewing gum, you can get a sort of history of what was happening there on the bacterial level, because it changes from the surface down into the interior, about how things progressed during the long period that the gum was living on the sidewalk
Chris - Any other prizes that particularly stand out?
Marc - The explosion of press coverage initially seems to centre on the Transportation Prize we gave to a large international team for some work that they did in Namibia. They did some experiments to try to see whether it's safer to transport an airborne rhinoceros upside down. They were trying to move some of the rhinoceroses who are growing scarce from areas where they live now, which are becoming extremely dangerous, to areas quite a distance away that would probably be much safer places for them to live, but it's not such a simple thing to transport a rhinoceros. It was too far to do it easily and well by truck. So they were using helicopters. And the question came, how do you do this in a way that's safest for the rhinoceroses? They did some tests and discovered that health-wise, it seems to be notably better for the rhinoceroses to be dangled upside down by their legs. Before they did this with the rhinoceroses, they ran a bunch of tests on human beings - on themselves - dangling each other upside down
Chris - I've been on a few flights where it's been uncomfortable and leg room has been an issue. I hope this doesn't give our low-cost airlines any ideas
Marc - Possibly you haven't thought this through
Chris - Go on
Marc - Possibly this is a good idea
Chris - But did they actually do the experiment? Have they actually done the experiment with real rhinos, Marc?
Marc - Yeah, this has been going on for quite a while, and this has become now the standard method for transporting rhinos. And they're also starting to use this as a fairly standard method for transporting other very large animals - elephants and others. They have experiments planned for possibly giraffes and some additional kinds of animals
Chris - So this must be one wonderful example of how an Ig Nobel Prize winning paper was serious science that has not just made people laugh and think, but also translated into real positive action
Marc - Yeah, it's a good reminder that almost all science, when it's in its very first stage, involves just a small number of people doing something that might look kind of crazy to everybody except themselves
Chris - I'm going to keep my thinking cap on. We did make a chocolate teapot once. Maybe I'll send you our manuscript on the making of a chocolate teapot to test whether it really does actually hold water
Marc - That would be so kind of you, thank you

20:01 - High fat diets can destroy the body clock
High fat diets can destroy the body clock
Lucasz Chrobok, Jagiellonian University
Do you like a snack at bedtime? We certainly do, and so do rats, at least ones allowed to feast on a high fat diet. And now, new research has shown that rats fed on a high fat diet end up with broken body clocks and disrupted eating and sleeping patterns. Cells in the brainstem that would normally make you hungry in the day and not-hungry at night appear to be disturbed by the high fat diet. There are implications for how we might treat human obesity in the future. Eva Higginbotham spoke to lead author Lucasz Chrobok to find out more...
Lucasz - In this new study, we found that in rats fed a high-fat diet, the activity of this brainstem clock is actually severely disturbed. And at the same time, these high fat diet fed rats increased their food intake during the day, the time these nocturnal rodents should normally spend on sleep and rest rather than feeding
Eva - You basically fed some rats a healthy diet, some rats a high fat diet, and saw that their sleeping behaviour changed?
Lucasz - We did not really measure the sleep behaviour, but we measured the food intake around 24 hours. What we saw in this well-balanced healthy group; that their food intake was limited to their active phase. With the high-fat diet fed rats; their food intake was all over the place. They would eat during the active phase but they would also eat during their behaviourally quiet time, which is day for these nocturnal rodents.
Eva - How high fat is high fat for a rat?
Lucasz - The standard high diet is 70% calories from fat. It's a really high fat diet.
Eva - Have you tasted it? What does it taste like?
Lucasz - I haven't tasted it, but it smells amazing, like cookies.
Eva - Amazing. When you looked at the actual nerve cells of the brain that are involved in setting the circadian rhythm, did you see that they were behaving differently?
Lucasz - Yes. Normally under a standard well-balanced diet, the neural activity of the brainstem clock is very rhythmic. During the day the activity goes up, it peaks at the late day. Then the activity slowly goes down during the night. And in the high-fat diet the neuronal activity of this brainstem clock is nearly totally flat. It does not really distinguish the time of the day.
Eva - That's really amazing. Do you think then that there's something about the fat in the diet that was affecting the clock? Or do you think it was something more about the rat's behaviour because they love the high-fat food so much?
Lucasz - We don't know the answer to this question because it either can be the calorie content of the diet itself, the fat that actually affects the brain cells, but it also may be a behaviour that as a feedback affects the brain. Because of the high tastiness of the food, rats eat it all the time. Then because the feeding pattern actually affects the clock, it just destroys it.
Eva - Rats are nocturnal aren't they? How applicable do you think their circadian rhythm and food intake system is to humans when we're obviously supposed to be up during the day and asleep at night?
Lucasz - Yes. One must be really cautious to extrapolate results from rodents to humans. However, with the brainstem being so evolutionary ancient, we really hope that this basic clock mechanism may be conserved among species
Eva - Do you think any of this could be linked to shift workers? People who are working during the night and then sleeping during the day?
Lucasz - Definitely. I think it's relevant to shift work in general. We know that in shift workers there is a high increase of obesity, some kind of cancer and cardiovascular disease. It is actually now speculated that it is good to lock your feeding patterns to the light dark cycle rather than to your activity cycles. If you are a shift worker and you actually work during the night, it would be good for you to even wake up during the day, which is a time you should eat, and eat during the day.

25:13 - What is sepsis?
What is sepsis?
Colin Begg, Paediatric Intensive Care Unit Glasgow
Sepsis has been known by a lot of different names in the past, from blood poisoning and septicaemia to ‘blood rot’ back in the 11th Century. But these terms all refer to the same dangerous condition, where the body’s exaggerated reaction to an infection causes severe collateral damage to its own organs and tissues. It’s a medical emergency, and the WHO estimates that it kills around 11 million people each year. Thankfully, prompt diagnosis and treatment can turn the tables on the condition. Eva Higginbotham spoke to Suzanne, a sepsis survivor, to hear her story...
Eva - Suzanne was a healthy 40 year old woman who, like many of us, seemed to catch a bit of a cold in the stressful run-up to Christmas three years ago.
Suzanne - I just started to get worse and worse, and I thought I was developing the flu. It came round to Christmas day and I was feeling really, really unwell but I managed to get to my family and my parents' house to spend an hour with them, when I was meant to be spending the whole day. I had to go home, just feeling really unwell. I was feeling terrible. Couldn't sleep. At four o'clock in the morning I was Googling symptoms about flu and for some reason thought maybe it's not flu, maybe I've got pneumonia. Quite quickly realised that my symptoms were much more like pneumonia rather than influenza. The advice was you must go and see your GP as soon as possible.
Eva - By this point she was so weak her husband had to drive her the hundred meters to her GPS office for her appointment the next morning
Suzanne - She did look a bit concerned, I think, when she saw me, but she put their sensor on my finger that measures your blood oxygen. It was in the 80 something percent, which is not good at all. I very clearly remember her saying, "I don't mean to alarm you, but I will be calling an ambulance and we'll be taking you to the Queen Elizabeth. You're not very well. You need to get to hospital as soon as possible."
Eva - Although Suzanne remembers the GP appointment, her memory pretty much goes blank for the next two weeks. She's had to rely on friends and family's descriptions of what happened next. She was rushed to hospital and put in intensive care before being put on a ventilator with her family waiting outside.
Suzanne - The consultant came back and said that things had spiralled out of control. I guess at some point in all of that, that's when it became apparent that I had sepsis. I don't really know at what point it was first diagnosed. I was on the ventilator, but my body had just kind of gone out of control and the oxygen that I was receiving through the ventilator wasn't enough to sustain me, to keep me going...
So, let’s explore what sepsis actually is, and how doctors treat it. Chris Smith spoke to Colin Begg from the Paediatric Intensive Care Unit in Glasgow...
Colin - The straight medical definition is essentially where your body gets an infection and then your immune system's reaction to that infection causes damage to your organs.
Chris - And how would a person who's going down that path know it's happening to them?
Colin - That's the million dollar question Chris. Really the initial signs of sepsis can be quite nonspecific. What we as medical professionals try to do is separate those people who have sepsis from those people who perhaps just have a bad infection. All sepsis starts with an infection and it's trying to identify those people who are going to progress on to sepsis. That is probably the hardest part of our job at times.
Chris - How quickly is it clear that someone is on that slippery slope from just what could be a trivial infection for most people to life-threatening overwhelming sepsis in that person?
Colin - It can be very fast. Sepsis is one of the few conditions in the modern world that can kill a healthy adult in a matter of hours. Globally it's still the number one cause of preventable death. Often we can get an idea within minutes by looking at somebody's vital signs and certain other simple tests that they are progressing to a more severe case of sepsis.
Chris - When we make the diagnosis, do we actually know, right this person's definitely got sepsis? Is that more a judgment call on the part of a doctor like you, who's putting together various measures and thinking, this person's not going in the right direction, they're heading towards this situation? Or are there some clear indicators this person has got sepsis?
Colin - There are clear indicators, but those can be quite non-specific. What I teach my registrars is, can they say for certain that this is not sepsis? Because the treatment is really broadly simple measures. By initiating those measures you can stop the cascade of sepsis very early and prevent people progressing to multiorgan failure, which is what you want to do. Really it's almost a 'shoot first ask questions later' approach a lot of the time in terms of the simple things we deliver like - oxygen, antibiotics, intravenous fluids. Then it's a question of going back and constantly reassessing the patient. It's one of those situations where expertise can be key, bringing a senior person in to see the patient can often make a difference.
Chris - Are there certain groups of patients that are particularly vulnerable to this happening that we need to watch out for?
Colin - Yeah. Like many diseases. Sepsis affects disproportionately the very young and the very old, particularly the preschool toddler/infant group and also the elderly, people over the age of 70, and people that have got any sort of immune problems. Patients who are immunosuppressed because of cancer, HIV, rheumatological disease, they're all more vulnerable to sepsis than the general.
Chris - Are there any particular diseases that we associate with sepsis happening more frequently? If one person is diagnosed with them we know to watch out?
Colin - Particularly simple things like pneumonia, a chest infection, or certain types of skin infection like cellulitis, certain urine infections. All of those can progress towards sepsis fairly easily depending on the bug that is involved.
Chris - How long does it take for a person to turn the corner and then recover after a bout of sepsis?
Colin - Again, that varies. It very much depends on the person's premorbid state. If they were healthy beforehand then generally they will recover quicker but that is not always the case. Sepsis can take a terrible toll, particularly the multiorgan failure aspect of it. If you spend a fortnight in ICU on support, that takes a toll on your muscle strength, on your physical ability to do simple things like move and breathe. It can take a long process of rehabilitation before you get back to your normal self and some people say they never fully recover.
Chris - What fraction of people don't make it?
Colin - Globally, the fatality from sepsis varies. In the UK it's probably in the order of 15 to 25% mortality, which is high. That's in adults. In my own field in paediatrics our baseline mortality is in the order of 3%. For every hundred people who come into children's intensive care; sadly three of them will not make it through. For sepsis the fatality rate, the mortality is much higher than that, probably in the order of about 10 to 15%.
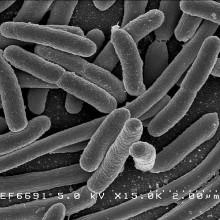
32:40 - What microbes cause sepsis?
What microbes cause sepsis?
Andrew Conway-Morris, University of Cambridge
Sepsis can arise from all sorts of illnesses, but what about the microorganisms themselves that cause the initial infection? Eva Higginbotham spoke to Andrew Conway Morris, an intensive care doctor specialising in sepsis at the University of Cambridge...
Andrew - You can get sepsis from bacteria, you can get sepsis from viruses. You can get sepsis from fungal organisms. And so really across the range, and equally some parasites, such as malaria in the severe forms, would also meet our definitions of sepsis. In terms of the common organisms that we see, the most common are certainly bacteria. And again, they come from a range of different types of bacteria. If we split bacteria, broadly speaking, into gram-negative and gram-positive, which is how they stain under a microscope, we see common gram-positive organisms, such as staphylococcus aureus, and many of your listeners may have heard of MRSA. Other common organisms would be E. coli and pseudomonas. And these are organisms that often we get from the gut or from the urinary tract. So it's a pretty broad field of organisms. And it's a very interesting question as to why you get the sepsis syndrome, how much of that is due to the bug and how much of that is due to the host response
Eva - And what is it that the host is responding to when they have an infection with something like e. coli?
Andrew - So the surface of the microbes, the bacteria and so forth, are covered in molecules. And what the body does, the immune system is able to recognise those patterns and says, this is an abnormal thing that shouldn't be here, and therefore I'm going to launch an attack because it shouldn't be here and it needs to go. Now, the key thing with sepsis is that that response is not localised to a specific area, but rather spills out into the rest of the body. And again, why that happens is one of the key questions of sepsis and one that we don't fully understand. There is almost certainly an interaction there between the bacteria and the host immune system. And some of that will be dictated by the host's own genetic background. Some of it may also be due to the experience of the immune system, whether they've encountered that bug before and also where in the body it's encountered. So e. coli one commonly has in one's gut. They live there without causing any harm most of the time, but if they spill out of the gut and they get into say, for instance, your abdominal cavity, to the space around the gut, or they get into your bloodstream, then your body mounts a very vigorous response to that, and that is probably what triggers sepsis.
Eva - And does the bacteria, or other infective organism, want this to happen? Like, is it in the gut trying to burrow through with some tools it might have in its toolkit? Or is that not exactly what it wants?
Andrew - There are clearly examples of organisms that have what we call invasive potential, who you get enteroinvasive e. coli, so that's e. coli that would invade through the wall of the bowel, or you get invasive streptococcal disease where you have a streptococcus pneumoniae, so causing pneumonia, and that spreads into the bloodstream, or sometimes into the central nervous system causing a meningitis as well as a pneumonia. And some of that will be due to virulence factors carried by those bacteria that have the potential for invasion. But some of it again is probably also down to the host response. If the area where the bacteria are becomes leaky and your barrier defenses break down, then that again, allows those bacteria that have the potential to cross, to cross into areas where they shouldn't be.
Eva - Can you always figure out, when you're treating someone for sepsis, what the microorganism was that caused the reaction?
Andrew - So, no, and in fact, it's very common, probably in around 50 to 60% of cases of infection that present to hospital we can't identify the infecting organism. In a relatively small proportion that will be because we got the diagnosis wrong, but most of the time it's because our tests for infecting microorganisms are just not very good. They are based on technology developed originally by pioneers, such as Louis Pastor, over a hundred years ago. And they rely on the growth of bacteria. And in order for the bacteria to grow, they need to be in the right conditions. And also the patient needs to have not been given antibiotics that suppress the growth of bacteria, and of course you must give antibiotics early. And so it is very common not to be able to identify the infecting organism. This is changing, technology is coming that allows us to identify organisms without relying on growth. So we can use molecular tests, things like PCR, polymerase chain reactions, which allow you to detect genetic material and doesn't rely on growth, but those tests are not yet widely available for bacteria. They're widely implemented for viruses, and that's exactly what we used for respiratory viruses like SARS-COV-2, to the cause of COVID. But for bacteria, they're not that well developed and we're forced to rely on broad spectrum, empiric antibiotics - so antibiotics that we pick because they're likely to cover the organisms we think will be there. And clearly that comes with risks of breeding resistance, of using antibiotics with a broader spectrum then we need to, possibly for longer than we need to. And there really is an urgent need for diagnostics in this area to allow us to rationalise our antibiotic therapy, to minimise the use of antibiotics and preserve them because they're a precious resource

38:43 - Sepsis: influenced by your genes
Sepsis: influenced by your genes
Kenneth Baillie, University of Edinburgh
Sepsis is an immune overreaction to infection that ultimately culminates in the body effectively shooting itself in the foot and damaging its own tissues, sometimes fatally. This is what nearly happened to Suzanne, who spoke to Eva Higginbotham a bit earlier...
Eva - After the ventilator in Glasgow wasn’t enough, Suzanne ended up being transferred through the night by a team of off-duty doctors and nurses to a hospital in Aberdeen who could deliver specialist treatment, which she thankfully responded well to despite being in liver and kidney failure already. Once back in Glasgow and doing better, her sedation was lifted…
Suzanne - The sedation was lifted when I came off the ventilator and it was, you know, trying to understand what had happened. Two weeks of my life had kind of disappeared, and I couldn't understand why I'd been in Aberdeen and what was going on. And then it was just kind of trying to recover from that, and being in intensive care and just lying in a bed for two week you lose a lot of your muscle mass. So it was, you know, I thought I could just stand up and get out of bed, but it took three or four physios to get me standing for the first time. Full recovery to full fitness was probably about a year, but I did go back to work on a phased return after about four months. It's amazing what one small pathogen can do, what a few small pathogens... I think that's the thing with sepsis, that so much of it is misunderstood, or not misunderstood, it's just not understood, why sepsis happens with one person and not another person
And that’s the key question: how an infection that’s relatively trivial for one person can cause a lethal catastrophic reaction in another. Some of that might be down to differences in our DNA. Kenneth Ballie studies the role of genetics in sepsis at the University of Edinburgh and spoke with Eva Higginbotham...
Kenneth - Well, your genes provide the code from which the whole of your immune system is created. So everything in your immune system is potentially altered by your genes
Eva - And how much variation is there between people's immune systems due to DNA, because of course, people's immune systems change all the time just from being in different parts of the world, being exposed to different infections, et cetera.
Kenneth - Yes, and you'd think that if you get an infection that the reason that's happened is because you've been exposed to a bug and that's what's causing you to become sick. But in fact, the degree of sickness you get is very strongly influenced by your genes. So in the 1980s, a group of scientists looked at people who were adopted in Scandinavia and found that if your adoptive parent died young of an infection, remember that's the person who brought you up, who you called mum or dad, and who may even have coughed on you during their final illness, you're no more likely to die of an infection yourself if you're adoptive parent died of one. But if your biological parents, someone you might never have met in your entire life, died of an infection, then you're six times more likely to die of infection yourself.
Eva - And is that then, that amazing statistic, is that then because your DNA has the code for making your white blood cells and the other cells that play important roles in your immune system?
Kenneth - Yes. So the immune system is an incredibly complex system, probably second only to consciousness in the level of complexity in the body. And of course, consciousness hasn't had to change since it first evolved, whereas your immune system changes the threats that it has to fight with each new generation of organisms. So it's become an incredibly complicated system. The other thing that makes it complicated is that the organisms themselves, the bugs that infect us directly, interfere in the function of your immune system. So if there's a vulnerability in it, the bugs find it. So trying to understand that system has been a colossally difficult challenge.
Eva - And so you've been trying to understand the link between people's genetics and sepsis. What have you been doing and what have you found so far?
Kenneth - We've been trying to use genetics to understand that system, to really find a shortcut to find the components of the immune system that change. The outcome for the patient and the reason of course we want to find those is because we want to find parts of the system that we might be able to change with a drug treatment. To do that we need to compare DNA from the right people, patients who are unfortunate enough to become desperately sick with sepsis and need care and intensive care units, and compare them to the rest of the population to find out what specifically in their DNA, what in their genes is different about them that's led to them becoming so desperately sick.
Eva - And have you identified any differences in the genes so far?
Kenneth - We find many differences in genes relating to COVID, but not in sepsis yet. So sepsis is a very difficult challenge. I think, as Andy hinted at in his interview, the definition of sepsis is very, very broad. So it's really hundreds of different diseases. And so in order to tackle that problem, using genetics, we're going to need to recruit very, very large numbers of patients. In fact, we've recruited many more patients with COVID into our studies than we have so far managed to recruit with sepsis. And of course, the reason for that is that intensive care medicine all over the world for the last year and a half has been very dominated by huge numbers of patients with COVID.
Eva - So seeing as your genetics has such an influence on your immune system, does that mean then that if you develop certain illnesses like sepsis or COVID that you just have a sort of weaker genetically defined immune system?
Kenneth - Not always, there are immunodeficiency diseases that often present in childhood in which part of the immune system is broken if the patient is born with that problem. But what we're teasing apart in COVID and sepsis is more the genetic tweaking of the immune system to make it better at one thing and worse at another. So the mantra in evolutionary biology is that adaptation comes at a cost. It's likely that the patients that we're seeing who are genetically susceptible to COVID or sepsis are probably resistant to something else. And we do have examples of that. So for example, in HIV, there was a group of sex workers in Africa who were exposed to HIV and never got it. And many of them were found to have a specific genetic mutation that made it hard for the virus to get into their cells. And that exact mutation that made them resistant to HIV, were the same people susceptible to a different virus called West Nile Virus, and in fact, a couple of other viruses. So those sorts of patterns probably exist across the whole immune system.
Eva - So how could a better understanding of the genetics lead to better outcomes for patients? How might this work in practice?
Kenneth - The effect of a gene is sometimes a bit like the effect of a drug. So it changes the way a bit of your immune system behaves at a molecular level. And in some cases we understand those mechanisms a bit. So where we find those sorts of signals, where we find that gene that changes your chance of becoming desperately sick with COVID or sepsis, and we've got some understanding of the biology of the molecular interactions that gene has, we might be able to design treatments that will have the same effect, the effect of preventing or ameliorating critical illness. And we've come quite close to doing that in COVID. There are two treatments that were inspired, at least in part, by genetic evidence that we provided early in the outbreak from a large study in intensive care units in the UK that are now being tested in the Recovery Trial. We don't have answers yet, but there's evidence from other trials that they might be effective.
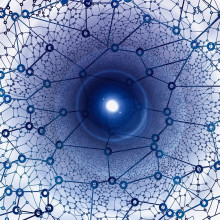
46:43 - Sepsis: using AI to find improve outcomes
Sepsis: using AI to find improve outcomes
Anthony Gordon, Imperial College London
Anthony Gordon looks for patterns in how different people’s bodies react to infections so we can pinpoint the best way to treat them. And he’s using artificial intelligence to help him. He's at Imperial College London and spoke with Chris Smith...
Anthony - We're trying to tackle this in a couple of ways. One is looking in the blood at what we call the gene expression, the message that comes from the DNA that Kenny has been talking about, that tells the body how to respond. And we're looking for patterns in that, so that if there are different patterns of how a patient is responding, we may then offer different treatments to those individuals.
Chris - In essence then, when someone's immune system is reacting, if they're going down the pathway that looks like they're developing sepsis, there will be different patterns of genes being turned on and off as their immune system goes into this metabolic tailspin. And you're saying, well, can we spot those?
Anthony - That's right. You've been hearing from the other speakers that it's a very complex system, so we're looking for these patterns. And we're sort of seeing that now, that maybe some patients have a lot of inflammation, and if we can spot that pattern they may benefit from anti-inflammatory treatments. And there may also be patients where their immune system is overwhelmed, and in fact they're a bit immune suppressed, and they need a boost to their immune system to help them fight any further infections. So that's the hope - that we can actually take these very non-specific signs that we usually use to diagnose patients and actually say, no, they're not always the same and can tailor our therapies appropriately.
Chris - What sorts of signals can you bring to bear with your solution and how does AI help?
Anthony - These patterns that you look for, clusters in the data that you as a human can't see, but the computers can look for these patterns. Then if it's something biological like the gene expressions, you can go back and try and understand the biology and maybe develop new therapies. What we're also looking at though is how can AI help us improve the current therapies we're doing? So again, we've used large databases, many tens of thousands of patients and using artificial intelligence where a computer looks at all the decisions made by hundreds of doctors treating all these patients and worked out therapies that we use all the time -things like fluid and what we call vasopressors, drugs that help boost the blood pressure, just looking at which were the best treatments that were offered for all these patients. And try, again, to spot those patterns and then actually offer a sort of aid to doctors to help them just optimise all of these many decisions they make in an intensive care unit.
Chris - Obviously the big hope is that we can follow the old medical mantra of "prevention is better than cure, always". Are there any signals that you can tap into that warn us early a person's going in the wrong direction? And we can therefore effectively change the course for them before they end up in the hands of people in the intensive care unit?
Anthony - Yes. That's the hope, that if you can detect these things earlier, and even if we can't diagnose the infection yet, because it takes a while to grow bugs in a laboratory, the body has recognised that there's an infection, it mounts its immune system response. And if we can tap into that and use the body's own early warning systems, we could intervene earlier and hopefully prevent what may be a simple infection becoming a more severe case of sepsis.
Chris - And is it working?
Anthony - I think we're making good progress in that. Like all these things it takes time to develop, but we've now got the diagnostic devices, the sort of PCR tests that Andy mentioned that we use currently for COVID to detect viruses. Hopefully you can change literally the cartridge that fits in the device instead of looking for virus DNA or RNA, look for the patient's DNA and RNA. And we can do that rapidly, the technology exists to do it in less than an hour, and that's the sort of work we are testing at the moment, making sure it's safe before we bring it into the health system
Chris - Because obviously, just in 30 seconds, agility and speed must be everything here because people can deteriorate so quickly when they go down that slippery slope of sepsis.
Anthony - Yeah. You need a combination of experienced staff, and also if we can use these new technologies, which will be much quicker, I think this can help all clinicians make better decisions and treat patients more effectively and hopefully improve their outcome.

52:10 - QotW: What happens to light's lost energy?
QotW: What happens to light's lost energy?
Cameron Voisey went off to figure it out...
Cameron - Waves are just one way in which energy can be transferred from one place to another, whether that’s light waves lighting up your room, or sound waves taking my voice into your ear. You may be aware that waves, like light and sound, can stretch. Listen to this, for example.
As the ambulance moves away from us, the siren seems to slow down, which means the sound waves appear stretched - this is the Doppler effect, and the same thing happens with light - we say that it ‘redshifts’, since the light loses energy and becomes more red.
But in Mark’s question something slightly different is going on. The stretching he mentioned is because our Universe is expanding - as space expands, so too does the light within it, stretching it and so losing energy. So, where does all this energy go? I spoke to Enrico Pajer, a cosmologist from the University of Cambridge, to find out.
Enrico - This is an excellent question, and in fact one which, in one form or another, is often a source of heated debate among practitioners. Many of us are familiar with the idea that energy is conserved: it might change from one form to another, but when we add up all forms of energy the grand total does not change with time.
Cameron - For example, when you boil a kettle, electrical energy from your home is converted into thermal energy to heat up the water - the total energy does not change. So, what does the light’s lost energy convert into then?
Enrico - The short answer to the question is that energy is not conserved in an expanding universe such as ours, and so the energy that is lost by light as it shift its frequency to the red simply disappears.
Cameron - So the idea that ‘energy can't be created or destroyed’ doesn’t actually seem to apply to our Universe on its biggest scales. James Fergusson, another cosmologist at the University of Cambridge, explains why:
James - Now, conservation of energy can be shown mathematically to be a consequence of assuming something called "time translation invariance”. This just means that we expect the laws of physics will be the same tomorrow as they were today. However, in expanding space the background isn’t constant in time, so time translation invariance is broken and the energy conservation doesn’t hold in quite the same way.
Cameron - Because our Universe is expanding, the Universe looks different from day to day and so too do our cosmological experiments - standard energy conservation disappears. So the answer to Mark’s question? Light does lose energy as the Universe expands, but that’s okay! Regular rules about not losing energy as light is stretched don’t hold in our expanding Universe, and instead, cosmologists can consider ‘spacetime’ as a whole to have absorbed the energy. This restores a conservation principle, but not, perhaps, as we knew it. Thanks to Enrico and James! Next week, we'll be looking into this question from Margaharet...
Margaret - Have frogs been seen scratching an itch?










Comments
Add a comment