This week we step out of the lab and into the hospital to celebrate one of our most treasured institutions. We find out about the technology that could be changing the future of healthcare and Connie tries her hand as a medical student. Plus, a potential treatment for Sickle Cell disease and do ice baths really soothe sore muscles?
In this episode

00:58 - Brain implant that restores touch
Brain implant that restores touch
with Dr Robert Gaunt, The University of Pittsburgh
Patients with spinal injuries can be robbed of the ability to move or experience  sensations from most of their bodies. And while scientists have begun to develop systems to eavesdrop on the brain's motor pathways and turn thoughts into movements - of robots and prosthetic devices - there's still no way to return any sense of touch. Now a team at the University of Pittsburgh have begun a series of experiments using brain implants that can begin to restore some of these sensations as Chris Smith heard from Robert Gaunt.
sensations from most of their bodies. And while scientists have begun to develop systems to eavesdrop on the brain's motor pathways and turn thoughts into movements - of robots and prosthetic devices - there's still no way to return any sense of touch. Now a team at the University of Pittsburgh have begun a series of experiments using brain implants that can begin to restore some of these sensations as Chris Smith heard from Robert Gaunt.
Robert - When people have a spinal cord injury, and this can happen for many reasons (a common reason is a motor vehicle accident), the connection between the brain and the rest of the body is lost, and if that injury occurs at your neck level, many people end up with paralysed legs and paralysed arms. The brain remains functional and it does its normal thing, it's just that its ability to communicate with the limbs (the hands and arms) is lost.
Chris - How might one try and surmount that problem?
Robert - Well, there's a number of different approaches that people all over the world are taking. One of the things that certainly has a lot of promise; people are actually trying to regenerate and regrow the damaged portion of the spinal cord so that that connection between the brain and the limbs are restored.
The way that we're tackling this problem is to actually implant little tiny wires into different regions of the brain that actually control movement and that are normally responsible for feeling the hand. And so we implant these devices into the brain and by listening to these signals and then actually pumping in information, we hope to be able to reconnect the brain to a device such as a prosthetic limb, or to a computer, computer cursors, things like that.
Chris - Have people not done this before though?
Robert - People actually have. There's been a series of work over a number of years now by a few groups, including our own here at the University of Pittsburgh, where people have been implanting these little grids of wires into the brain and listening to the signals. And people have used those signals to be able to control a robotic arm so that they could reach out and grab objects, but one of the key things that's been missing in that is the ability to feel that object. When you reach out and grab an object with this robotic arm, you can't feel it, you don't know if you're holding it. You can see it but you can't feel it, and so what we're doing now is trying to restore that feeling, that sense of touch, when the robot arm goes out to grab it.
Chris - You've said you send signals into the brain but actually talk me through the nuts and bolts of how you do that physically...
Robert - We know the parts of the brain that are actually normally responsible for processing this information or listening to the signals that normally come from the hand and so what we did in this study is we put these same grids of electrodes into the region of the brain that we know is responsible for normally listening to and processing information that comes from the hand. So what we do here is actually use little tiny electrical pulses, and these little electrical pulses make these neurons become active. And when these cells become active, the person that we're working with can perceive touch coming from that part of the hand that that part of the brain is responsible for.
Chris - So you actually did this in a spinal injury patient?
Robert - That's right. We've been working with the person injured about ten years before we did the implant and we've had these implants in place now for about a year and a half and so, when we stimulate, he feels as though sensations are coming from his own hand.
Chris - What sorts of sensations does he say he "feels" when you do this?
Robert - That's a great question and it's turned out to be a really interesting part of the study. The types of things that the person we're working with will say is that he feels sensations of pressure, occasionally he'll say it feels like light touch; he also says things like electrical or buzzing. But really what we show here is that when you do provide these stimulus strains it feels as though it is your own hand being touched. We've got a lot of work to do on making that feel more natural in some cases, but it really sort of lays the groundwork for showing that these sensations can actually be provided through a direct interface with the brain where we actually go in and sort of tickle these neurons with a little bit of electrical stimulation.
Chris - And how does the patient take to this - does he feel a bit strange feeling that he's feeling his body doing things which it's not doing?
Robert - He has used all sorts of different words and phrases to describe this sensation and sometimes he will say that it does feel strange. It's hard to describe what it feels like to have this part of your hand touched or stimulated that you haven't felt in a decade but he's able to understand those sensations very naturally. So he knows exactly if it's his pinkie finger that's being touched or his index finger that's being touched.

Cholera in Haiti
with Dr Nick Thompson, The Wellcome Trust Sanger Institute
Hurricane Matthew caused devastation recently when it swept through the 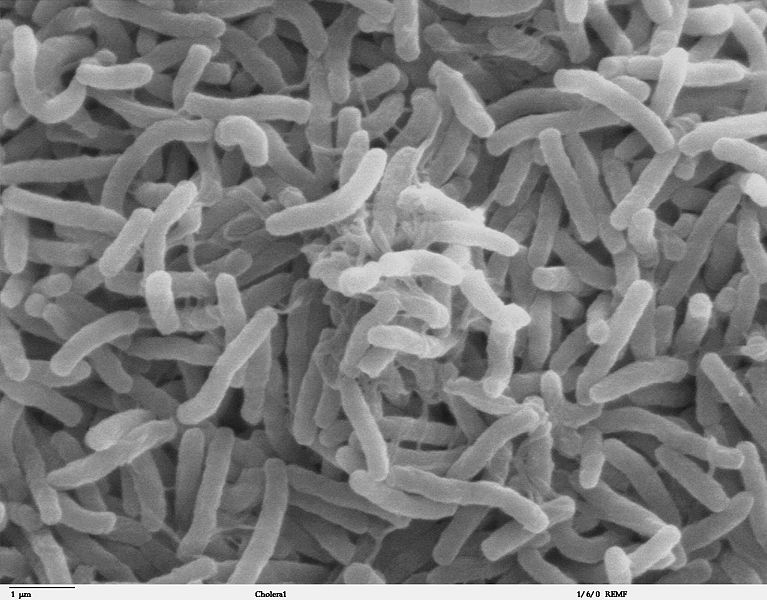 Caribbean. The country worst hit was Haiti, and one legacy of the destruction is an outbreak of cholera. This bacterial infection produces a relentless watery diarrhoea so severe that it leads to serious dehydration, low blood pressure and even fatal organ failure. What's so sad is that Haiti had been cholera free until a well-meaning aid effort a few years ago brought the bug back there. Chris Smith heard how from The Wellcome Trust Sanger Institute's Nick Thompson...
Caribbean. The country worst hit was Haiti, and one legacy of the destruction is an outbreak of cholera. This bacterial infection produces a relentless watery diarrhoea so severe that it leads to serious dehydration, low blood pressure and even fatal organ failure. What's so sad is that Haiti had been cholera free until a well-meaning aid effort a few years ago brought the bug back there. Chris Smith heard how from The Wellcome Trust Sanger Institute's Nick Thompson...
Nick - Haiti's recent encounter with cholera started in 2010. Prior to that Haiti had been cholera free for about one hundred years and it really wasn't a country you would have associated with cholera outbreaks. But it was a country that was actually under world scrutiny in that the U.N. had sent a mission to Haiti to rebuild infrastructure in 2004 and cholera broke out in 2010. That timing, the 2010 outbreak of cholera and the circumstances that led up to that were very strongly associated with a fresh group of U.N. peacekeepers arriving from Nepal into Haiti to help rebuild infrastructure. And the U.N. have just admitted their role in the introduction of cholera into Haiti because the cholera that broke out in 2010 are very closely linked to those strains circulating within north India and Nepal at the same time.
Connie - So it was actually carried there from this rebuilding mission, the cholera was actually carried over to Haiti?
Nick - That's right. It's tragic really because, actually, the mission had incredibly positive and good intentions.
Connie - That's really quite devastating! So Haiti has just been hit by this huge hurricane and one of the big things that's being reported back from this is a massive surge in cholera - why is that and what's going on?
Nick - The whole point of the U.N. working in Haiti was to rebuild infrastructure in a country that didn't really have any infrastructure, and the reason that cholera took hold in Haiti was because most of the accommodation after the earthquake in 2010 was destroyed. People live in very ramshackled accommodation with almost no sanitation and access to drinking water and so there's been a lot of effort to improve that. And, of course, that's all been wiped away by the latest hurricanes, so Hurricane Matthew has destroyed much of the good work that's been done in trying to rebuild that infrastructure.
And so any destruction in the infrastructure, the sanitation, mixing of human waste and drinking water means that that population becomes incredibly vulnerable to this diarrheal disease. And cholera, epidemiologically, it's such an explosive disease, it can go from a very small number of cases to hundreds, or even thousands of cases in a very short period of time.
Connie - What can we do now to move forward and try to deal with this situation?
Nick - The primary treatment for cholera is oral rehydration. And so people get dehydrated very quickly but if they continue to resupply their body with contaminated water then they're just reinfecting themselves. So the classic response to cholera is to provide clean drinking water and to rehydrate those people that are most affected.
A vaccine to cholera is something that is one of the main strategies for treating and preventing outbreaks that we see in places like Haiti. And so there are several candidate vaccines that are being used and so investment in vaccination strategies is something that we hope to see more in the future.

10:39 - Do ice baths soothe sore muscles?
Do ice baths soothe sore muscles?
with Dr Kat Arney, The Naked Scientists
It's time for our regular mythconception, and this week Kat's been chilling out - literally.
Kat - If you're an elite athlete at the top of your game - or even just a keen amateur or weekend warrior - you'll want to know how best to look after your body. One technique, used by sportspeople ranging from Andy Murray to Jessica Ennis-Hill is to pop yourself in an ice bath after exercise, to speed up recovery, reduce inflammation in the muscles and boost repair. At least, that's the theory, but an increasing number of research studies are showing that it doesn't actually have that effect.
The latest research, led by Australian and Norwegian scientists, looked at nine young men who were training a few times a week. They either sat in water at a chilly 10 degrees Celsius, or did a low-intensity warm down on an exercise bike. The scientists took small samples from the sporty chaps' muscles, and discovered that exercise causes the muscles to flood with inflammatory immune cells, and increase the activity levels of genes involved in inflammation. Yet there was no difference between the two 'cool downs' in terms of the levels of molecules associated with stress and inflammation. Of course, this was only a small study, and was just men, but it's not the only one to show that ice baths don't help recovery.
A 2007 study in the Journal of Sports Sciences found that men who plunged themselves into an ice bath after a gruelling 90 minute sprint session had no differences in the levels of a molecule called creatine kinase - which is a marker of muscle damage - compared with those who skipped the cold soaking, although there were a few other molecular markers of recovery that did reduce with a dunking. A 2014 study of rugby players taking part in a simulated match showed that cold water baths had no effect on their recovery. People have even tested different timings and temperatures - but it doesn't make a difference. Other studies have even found that ice baths might actually delay the recovery process. For example, one study testing sprinting cyclists found that a ten-minute cold water bath reduced their performance when they were asked to sprint again an hour later, compared with an active warm down.
The other thing to consider here is that although a cool shower after getting all hot and sweaty on the track or pitch might be lovely, freezing ice baths are pretty unpleasant. And given the lack of solid evidence showing that it's helpful - and some showing that it's actively not - why do people still go for a dunk in the ice? In fact, the main benefit seems to be psychological - athletes think that such a horrible thing must be doing them good, and there's enough sciencey-sounding stuff about reducing inflammation to make it seem like a good idea. Plus, ice bath studies suggest that people who take the plunge say they feel less sore than they would have been without the ice bath. So what do we know about the scientifically-proven ways to recover after exercise? One thing that's often mentioned is massage. However, an analysis compiling many studies of massage, known as a meta-analysis, carried out in 2016 concluded that the benefits of massage - if any - are small, and may only apply for certain types of exercise rather than a panacea for every athlete. But, again, it does feel very nice and probably has a psychological benefit if not a physical one.
Anyway, as far as I'm concerned, the only ice I'm interested in after exercise is the stuff that clinks in my glass of gin and tonic. Cheers!
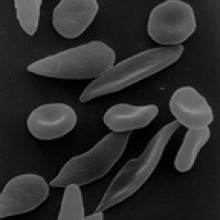
14:25 - New treatment for sickle cell disease?
New treatment for sickle cell disease?
with Dr Mark DeWitt, University of California, Berkeley
Sickle cell anaemia is an inherited blood disease. About a quarter of a million  children are born with it every year and they suffer low blood counts, joint and bone pain as well as other health difficulties. At the moment treatments are quite limited, but now a team at the University of California, Berkeley, have developed a technique to genetically edit the bone marrow cells that produce the affected blood cells and fix the problem. So far they've proved it works in a dish and also in mice given human blood cells. Researcher Mark DeWitt told Chris Smith how...
children are born with it every year and they suffer low blood counts, joint and bone pain as well as other health difficulties. At the moment treatments are quite limited, but now a team at the University of California, Berkeley, have developed a technique to genetically edit the bone marrow cells that produce the affected blood cells and fix the problem. So far they've proved it works in a dish and also in mice given human blood cells. Researcher Mark DeWitt told Chris Smith how...
Mark - Individuals that have sickle cell disease produce red blood cells that have an abnormal or sickle shape and these so-called sickle red blood cells can clog blood vessels. And in so doing it can also cause chronic pain, organ failure, pulmonary hypertension so individuals that have the disease have a dramatically reduced quality of life. And even in developed countries like the U.K. or the United States, only live until about an average age of forty.
Chris - How is the disease managed if someone presents with sickle cell disease - how do we look after them?
Mark - Individuals with sickle disease are often managed using blood transfusions, so you transfuse healthy blood to replace the sickle blood. There is a pharmacological intervention, hydroxyurea, which has serious side effects but can reduce the manifestations of sickle disease. There is a treatment for the disease and that's a bone marrow transplant.
Chris - And how does that work?
Mark - The same as if you're getting a bone transplant for leukemia. You find a suitable bone marrow donor and you what we call ablate, or basically kill off the bone marrow in the recipient and then you take bone marrow from a healthy donor and infuse it into the recipient. And so you, basically, you get new bone marrow and then you're effectively cured.
Chris - The rationale, of course, being that the new bone marrow doesn't have the genetic problem that makes sickle cells disease which is why the people are better. But it's obviously a very radical step to take isn't it, with a lot of risk attached so what are you trying to do instead?
Mark - We're developing methods to correct an individual's own bone marrow. We know exactly the nature of the mutation, we know exactly where it is in the genome. The sort of idea is that we would take the bone marrow out from the patient, you would correct it using the technology called CRISPR-Cas9, and then you take the corrected bone marrow and put it back inside the patient.
Chris - How practical is this - do you think that you could treat enough cells and edit them in this way to put the gene right and then get enough of them back into the patient to make the disease symptoms go away?
Mark - We think that we can. One only needs to correct a small minority of the bone marrow for the patient to be functionally cured of the disease because the healthy cells will outcompete the diseased cells in your blood and in your bone marrow.
Chris - So what evidence have you got that this is going to work?
Mark - What we did in this study was we obtained bone marrow cells from an individual with sickle cell disease and then we corrected the mutation using CRISPR-Cas9, and then we confirmed that they appeared to be healthy; they produced significant quantities of adult hemoglobin, and then engrafted the edited cells into a mouse model. The edited cells can successfully engraft in a mouse and persist over a period of four months and this tells us that the edited stem cells are viable for a transplant type procedure.
Chris - Indeed, that you haven't rendered them unhealthy that they can survive and, presumably, were they to do into a patient they would have a good prospect of finding their way to the bone marrow and then setting up the production of fresh, healthy red blood cells that could make up for the problem the patient previously had?
Mark - Correct.
Chris - So how do you actually do the edit process, as in once you've got those cells in a dish in front of you - how easy is it to do this genome switch to get rid of the sickle cell change and render the cells genetically healthy?
Mark - It turns out it's actually quite easy. The way we do it is we take purified Cas9 protein and we mix it with this thing called a guide RNA, which is exactly what it sounds like, it's a little piece of RNA that guides the Cas9 protein to the the sickle mutation inside the cell's genome. We also provide a short piece of DNA that programmes and edit; in this case from sickle to wild type. Cas9 makes the cut, the short piece of DNA past in and voila - it's all fixed.

19:13 - Hacking illegal animal trafficking
Hacking illegal animal trafficking
with Sophie Maxwell, ZSL London Zoo, Mahvash Siddiqui, US embassy, Zack, Eddie, Caroline, Zoo-hackers
After habitat loss, the buying and selling of illegal animal products, as decorations, medicine, jewellery or meat, is the biggest threat to wildlife conservation worldwide. But it's a complex problem to solve - do you tackle the demand, the trafficking or the poaching? Well, maybe the solution lies a little outside the box. Georgia Mills went down to ZSL London Zoo where, last weekend, when they weren't trying to track down an escaping gorilla, they were participating in a big global event...
medicine, jewellery or meat, is the biggest threat to wildlife conservation worldwide. But it's a complex problem to solve - do you tackle the demand, the trafficking or the poaching? Well, maybe the solution lies a little outside the box. Georgia Mills went down to ZSL London Zoo where, last weekend, when they weren't trying to track down an escaping gorilla, they were participating in a big global event...
Georgia - This is is a sound from a room in the heart of ZSL London Zoo. Instead of the usual fare of lions or penguins, this room is full of programmers and conservationists who've been up for about two days straight - this is a hackathon.
Sophie - My name's Sophie Maxwell and I lead the conservation technology team here at ZSL...
Mahvash - Hi. My name is Mahvash Siddiqui. I'm the science diplomat at the US Embassy in London.
Sophie - So this is the first ever global ZooHackathon event. It's organised with the US State Department and it brings together zoos from around the world to come up with solutions to the illegal wildlife trade.
Mahvash - Well, for the US, wildlife trafficking basically is a Presidential priority. So our President has basically asked for the US Government to look for solutions which are out of the box, twenty-first century solutions to basically deal with twenty-first century challenges.
Sophie - So, there are a hundred and fifty participants who have all come together to answer some problem statements; these problem statements have been set for them my conservationists. So conservationists have come together around the world and said - what's really going to transform and solve this problem.
Mahvash - People have been involved in curbing wildlife trafficking for decades and yet the trade is burgeoning - it's a ninety billion dollar trade.
Sophie - Some are doing coding, they're using lots of different scripting languages. They're using massive data sets here that we have as part of ZSL so we have big ecology data sets that they can use to feed their solutions. They're using newsfeeds from APIs to bust criminal networks. They're using creative solutions as well. So we've got strategic people, coders, designers, all coming together in a real team mix to pool their skills to pull this off in a forty-eight hour period.
Georgia - Can a group of volunteers build something from scratch fueled only by copious amounts of coffee and the odd burrito, which could then be used to tackle the complex problem of the illegal wildlife trade? I met with some of the teams...
Zack - Hi I'm Zack Baynham-Herd. I'm a PhD student at Edinburgh University. Our team name's "the underdogs" but our products is wild coin.
Georgia - Talk me through - what's wild coin?
Zack - Essentially, wild coin is peer to peer conservation. A platform for people who have the financial resources to invest in fund conservation and those on the ground who are actually doing conservation. The idea being anyone could be a conservationist.
Georgia - Okay. So how would this work - is this something people can download?
Zack - Yes but this would be an app that you can download on your smartphone or it's accessible to the internet. And you search for any species that you care about, that you want to preserve or any cause such as illegal wildlife trafficking. You can search and you can find the people and the organisations on the ground who are actually doing this stuff and you can decided how much you want to fund, and who you want to fund, and what you want to fund.
Georgia - Oh, I see. So say I'm like I want to save the tiny red panda, I can find out exactly who is doing that work?
Zack - And if the tiny red panda isn't being funded you can post or you can say that you want to fund this. And then conservationists who have the resources to actually do conservation but maybe don't have funding can be like - hey, here's someone willing to fund this; we can do this.
Eddie - I'm Eddie. This is the team - we are reading palms and we are working on palm oil potential conflict zones. Deforestation and native forest land for palm oil plantations is disinheriting orangutans from their native habitat. There are poachers who use the networks created by the palm oil trade when they're going into native forests they're creating roads which are then give access to poachers.
Georgia - What's your creation going to do about this?
Eddie - We're creating an app which alerts people on the ground to changes in land use. So there's a data set from the copernicus satellite from the European Space Agency; they have two which orbit the Earth every ten days giving us an ability to update satellite imagery every five days. From that we can extrapolate any change of land use to be able to identify uncertified palm plantations and new sources of habitat destruction and stop that from happening.
Georgia - A matchmaking service for conservationists and an eye in the sky monitoring illegal deforestation. Pretty impressive for forty-eight hours.
And that was only the start. There was also an app for people to anonymously whistle blow on poaching, a facebook bot which could tell you if there was pangolin in your stew, and a fun looking game which raises awareness about the ivory trade. And then...
Caroline - erm So "look out" is basically a very user oriented web app.
Georgia - This is Caroline Fletcher, slightly buzzing after her team were just announced victorious. Caroline's team had designed a system which alerted tourists about the illegal products on sale in countries they're about to visit.
Caroline - So a lot of people are unknowingly buying, so for example, Macaw earrings, which look really beautiful. Like you see feathers all the time - why shouldn't you buy it. It doesn't really make sense but, actually, they're really endangered. And it's creating that awareness, creating that knowledge about unknown illegal wildlife trafficking.
Georgia - So Caroline's team won this prize but... what's next for all these other ideas? Back to Sophie Maxwell...
Sophie - Well, we were just having conversations about that now and we have a portal called "Wild Labs." We're encouraging everybody to register on Wild Labs to connect donors, corporations, commercial environments with ZSL, with this talent who has come to us today, to take these to the next level because ZSL is wholly committed to really furthering these solutions to make impact on the ground. So we can take away some today and actually start using those things and really, what we want to do is just make sure that those evolve, they don't die, they live on, and they make impact.

26:25 - Taking the history of hospitals
Taking the history of hospitals
with Professor Jonathan Reinarz, The University of Birmingham
How have hospitals become such huge institutions? Medical historian Jonathan Reinarz talked Chris Smith through the history of hospitals starting with the very first ones...
Jonathan - Well, I think the first hospital would have been much smaller than what we have today. You have to think - that moment when you have a large group of patients together in one place, and this often happened on military campaigns, for example, when you have empires expanding, like the Roman Empire. Hospitals might have been set up alongside camps to treat a large number of wounded soldiers at one time. But also, across countries, you would have had these religious buildings like monasteries developed which had facilities, which we might describe as hospitals. A place which offered hospitality but often people who were very weak and weary from extensive travel who had maybe acquired some sickness and, eventually, people realised the benefits of having care organised in this sort of way.
Chris - Were hospitals initially for everybody or was this somewhere that only the needy went?
Jonathan - Absolutely! Now this is a very important distinction. From the earliest days hospitals were institutions for people who couldn't ordinarily afford to have a private practitioner treating them within their own home, and a home of a size which would have allowed one bedroom to be essentially set aside as a ward, or a private ward essentially. So yes the poor, but not all the poor. In the sense that people were going to fund this institution often locally and what they wanted to ensure was that the health of people who worked in local industries and who had helped people locally develop wealth and power. So, essentially, these institutions were for a particular type of poor which many people described as "the deserving poor." And they were deserving because they had ordinarily worked but then became sick, and in order to avoid these people and entire families falling into destitution the best idea was to aid their recovery as speedily as possible by providing care in an institution like a hospital.
Chris - When did it dawn on doctors that actually having hospitals is a good thing because all the time that they are dealing with people in hospital, they're not having to do long journeys out to random places to see one person - they can see lots of people all at once and possibly learn lots of things at the same time?
Jonathan - Absolutely. I would say that one misconception is that these institutions were run for the poor with medical practitioners volunteering their time through altruism, that they simply wanted to help the poor. It's clear that they offered a lot of benefits and for medical practitioners who ordinarily were collecting fees from paying patients, they quickly realised if they got a post at a local hospital, they would be recognised as the leading practitioners locally, so it advertised your expertise. So people would do this work free of charge because it set them apart from all the other competition and pretenders. It was a very crowded medical market place and if there were only a few hospital positions, well then people saw the advantage of having one of these.
But, at the same time, anybody that was associated with these institutions very quickly realised that they would see more patients of a particular condition than they might have seen during their entire career in private practice. And this is something that was reiterated by everyone who was involved in setting up some of the first specialist hospitals, so whether it was Moorfields Eye Hospital or a children's hospital, people emphasised that by spending a few weeks or even months on the wards, they would see more cases than any other private practitioner would have seen through their careers. And that immediately translated into expertise that you could have by affiliating yourself with hospitals, and people certainly recognised that advantage and that would lead a lot of practitioners to spend time in hospitals.
Chris - And, presumably, underpinned the whole ethos and idea of a teaching hospital?
Jonathan - Well absolutely. Once you get these teams together then one of the natural affiliations is to connect these hospitals with the medical schools locally. So, eventually, any reputable medical school would only be recognised in the Victorian period if it had a sizable teaching hospital connected to it, like Addenbrooke's, like Charing Cross, like any teaching hospital today.
It started with a certain number of beds, usually about a hundred. Not a dozen as might have existed in the first general hospital when it appeared locally, but guaranteeing at least a certain number of patients and enough space to bring an entire medical school into the hospital. So this tradition of walking the wards was very much there when you look at the first provincial medical schools in this country, for example.
Chris - And when did this seeming transformation occur which took us from this small stable with a handful of patients in it to the huge great institutions that hospitals are globally today?
Jonathan - Well, I think that that transition is really one that depends on the local economy and I think if you're talking about a hospital in a capital city, of course there's a lot of national pride involved. People will certainly invest in this sort of institution. You have to understand when these hospitals were first established, there were very few large buildings like this in most communities. People took notice and they often include hospitals in their visits; royalty coming from other countries to this country would have included a hospital visit on their visit and gradually as you see this kind of development in other countries, the primary institution to ensure is established is a hospital. So in a lot of other countries around the world it was clearly an object of civic pride and the bigger the hospital the stronger the economy, the stronger the nation. And especially in countries like China today, they build hospitals bigger than any we've seen before and that is just one more indication of how large and strong their economies have become.

32:50 - See one, do one, teach one
See one, do one, teach one
with Calum Worsley, The University of Cambridge, Professor Annie Cushing, Queen Mary University of London
Hospitals have become a place of training and they're where all our future doctors take their first steps into medicine. But how on earth do you train a doctor in the many varied and technical skills required to be able to treat everyone that comes through the doors? Well, in medicine the best way to learn is to do, so Connie Orbach popped down to Cambridge University's clinical skills lab to get some training of her own...
Calum - So, a couple of needles; tubes for blood; a couple of wipes to clean the skin; some swabs for afterwards...
Connie - Taking blood - one of the many skills that all medics learn before they graduate. But how do you teach such a thing? Well instead of sending a first timer to stick a needle in a patient's arm, students are sent to the clinical skills lab - a practice room fully kitted out with plastic arms and bags of blood. I persuaded fifth year student, Calum Worsley, to take me along and give me a taste of being a medical student. First up - choose your arm...
Calum - The choice is yours - they've all got these little name bands on them. Who've we got here - Moe Szyslak.
Connie - Isn't he the bartender in The Simpsons?
Calum - Yes, yes, yes.
Connie - He's' not yellow at all.
Calum - Well... not yet.
Connie - Not until I've got hold of him. Okay so what's next?
Calum - Wash your hands; gloves on. Part of the realism of this is to talk to this arm as if you would to a patient.
Connie - Next, add a tourniquet around the upper arm to increase the blood pressure and it's time to pick your vein.
Calum - If you just run your finger, you can feel a little bump where the vein is, and if you press on it feels a bit sort of spongy.
Connie - Then, give the arm a wash, grab your needle and...
Calum - Mr Szyslak - sharp scratch coming up, okay? Here we are, so we're in the right place, so we pull this back, point at the tube and we've got nice red stuff in the tube.
Connie - Success! It's easy right?
Calum - Now we'll just as Mr Szyslak to press on there for a couple of minutes to make sure you're not bleeding any more. And we'll label these to make sure they go to the right place ... perfect!
Connie - Well, I mean you did that one.
Calum - Seen one. Do you want to do one?
Connie - Yes, I guess so. You're going to have to hold the microphone.
Calum - That's fine.
Connie - Calum took me back through the steps one by one and it didn't go too badly, or at least Mr Szyslak didn't complain. But a plastic arm is a far cry from a real one and that's why, in medical school, students will practice on each other for a more realistic experience. So Calum, how about it - would I be able to practice it on you?
Calum - I hate it but we'll find you someone.
Connie - Okay, I'll see if we can persuade someone around this building to let me... Not so keen then. Well luckily for the unsuspecting staff of the Deacon Centre, I managed to persuade Calum to do his bit for radio. You're going to let me take your blood after having said it's something that really freaks you out?
Calum - Well you get a bit used to it. We all try doing it on each other.
Connie - Okay, the pressure is definitely on me. This is not the right thing to say but now I know I'm going to do it I've actually got butterflies in my stomach. Not very reassuring. Luckily Calum didn't change his mind and successfully coached me to taking his blood but I don't think I'll be hanging up the microphone just yet.
Now I'm just going to... just prod it in.
Calum - Yes, done.
Connie - Oh and it's filling.
Calum - Perfect.
Connie - And this one doesn't look like ribena, it looks like real blood.
Calum - That's it now and just relax.
Connie - You're the one who's having your blood taken and I'm the one who's hands are shaking. Clearly I have a lot to learn and, even if I did manage to hit the vein first time, my shaky hands and anxiety would not have put the patient at ease. And that's a lot of what is taught at medical school - how to act with patients. But how much of a difference can a good bedside manner really make? Well, according to Annie Cushing from Queen Mary University in London... quite a lot!
Annie - Physical health like blood pressure and blood sugar control in diabetics are shown to be improved as well as emotional health. Women with breast cancer are better able to adapt to their diagnosis, and less likely to have depression, when they feel their communication with their doctors is good. Communication is, obviously, important in helping patients manage their condition, such as lifestyle changes and we do know that a high proportion of drugs (between a half and two thirds) are not taken properly or as recommended by patients. So it has been suggested that improving medicines taking by patients may have a far greater impact on clinical outcome than any improvements in new treatment methods.
Connie - So the way a doctor communicates is important. But, how do you teach this sort of thing - send them off with a list of the right and wrong things to say?
Annie - We have particular sessions where we use actors who can play the part of a patient with a particular condition or problem and the students get to practice. We sometimes video record them so that they can see themselves, and they get feedback from the patient on what was working for the patient or what they found difficult in terms of understanding the student or in terms of aspects of the kind of non-verbal side. Whether they felt the student was interested in them and how they detected that. We also encourage our students to actually ask patients for feedback when they're out there in clinic, to ask for any comments on how they found it talking to the student. And in these ways we deliberately approach the learning of communication skills as part of good medical practice.

39:03 - Infection control to the rescue!
Infection control to the rescue!
with Cheryl Trundle, Addenbrooke's Hospital
The hospital may be the safest place to be when you're acutely ill but bringing so many vulnerable people together is not without risk - primarily owing to infection. Luckily, most hospitals these days have a dedicated team in place to spot threats before they become a problem. Connie Orbach went to Addenbrooke's hospital to find out how it's done.
many vulnerable people together is not without risk - primarily owing to infection. Luckily, most hospitals these days have a dedicated team in place to spot threats before they become a problem. Connie Orbach went to Addenbrooke's hospital to find out how it's done.
Good afternoon, infection control... Hello, how can I help you?
Cheryl - My name's Cheryl Trundle. I'm one of a team of infection control nurses. I've been working at Addenbrooke's for a long time time now so I've seen most things.
Does he still have diarrhea? I'm assuming if he's going home, he doesn't have diarrhea. So does he have diarrhea or not?
Cheryl - Depending on the signs and symptoms, viral diarrhea and vomiting, certainly in a gram stools, in a gram of poop, there are millions of viral particles. So obviously it's very infectious and easily picked up by anyone in the near vicinity, so we need to get on top of these things as quickly as we can.
So there are all sorts of reasons why it's good to prevent infections and reduce them too as much as we can. And the statistics for Europe say that over four million patients are infected by hospital acquired infection or healthcare associated infections every year, which is a huge number. And that can lead to six million extra days of hospital stay and three hundred and seventy thousand deaths due to infection, and the costs of that are enormous - over seven billion euros.
Connie - Hospitals are places of healing, but they're not without risk and, in particular, the spread of disease. To minimise these risks there's a specialised team of people ready to jump into action at a moment's notice from the wards.
Cheryl - The sorts of questions we would need to know are: names of patients; what they're underlying diagnosis was; what were their current signs and symptoms that would have made her anxious and would have caused her to call us; how many patients were affected; were any staff affected. So it's really getting all the information we can to build up a picture to help us to move forward.
Connie - Once the team have all the info, they'll collect stool samples to send to the lab for analysis. These results come back pretty quickly, but to stop the virus spreading, action is often taken straight away. Communication is key and other hospital teams are quickly alerted, as well as the local community; old people's homes and GP surgeries all have a hotline to the hospital.
Cheryl - First of all perhaps close a bay if patients were infected or involved, or perhaps two bays on a ward. If it's more than that then we would close the ward down; we would stop patients from going back to nursing homes; we would also restrict visitors, and staff movements would be restricted as far as we could.
Connie - After a flurry of activity, the team have done all they can and the next few hours become a waiting game.
Cheryl - There's no specific treatment for most viral illnesses, including diarrhea and vomiting. We'd make sure the patients were well hydrated, kept comfortable; it's usually something that only lasts between forty-eight to seventy-two hours and the patients usually gets better without any specific treatment.
Early recognition is the most important thing, so making sure ward staff know what to look for and, as soon as they think there's a problem, they phone us. Once it's got a hold, you can imagine on a ward of thirty-six patients, that's a lot of people to go through and can have serious consequences.
Connie - Because often a lot of these people are very vulnerable?
Cheryl - Absolutely, absolutely! And while you and I would get better in twenty-four, forty-eight hours, some of these people will suffer for longer.

42:59 - Technology: transforming healthcare?
Technology: transforming healthcare?
with Dr Ali Parsa, Babylon Health
Another solution to tackling infection would be to keep people out of hospitals - or the doctor's surgery - altogether. A new App called Babylon Health claims it can bring a medical diagnosis to a user's pocket. Founder and CEO Ali Parsa took Chris Smith through the fine print...
or the doctor's surgery - altogether. A new App called Babylon Health claims it can bring a medical diagnosis to a user's pocket. Founder and CEO Ali Parsa took Chris Smith through the fine print...
Ali - It's an app that brings you to your doctor as much as possible in your pocket, wherever you are. So you can make appointments in seconds, see a doctor on your mobile phone as you facetime with anybody else within minutes. If you have a symptom you can triage yourself and we have one of the world's most advanced artificial intelligence that will look at billions of variations of symptoms and very accurately will tell you what you should do next.
We have the ability to monitor you; everything from the health of your liver to your kidney to your heart and have it all in your pocket for you to see. We keep your clinical records and we can do tests and send you kits when necessary. We connect you with the specialists and psychologists, again in the same way.
Chris - So just to unpack that a little bit - so people with a smartphone, you would download this app and install it and then it would be what, a pay per go system or is it free - how does it work?
Ali - You could do all of the above. And if you want to buy it and use it yourself, you either pay five pounds per month and you have unlimited access to a GP, or you just pay twenty-five pounds and use it when you want to see a GP. But if you ask a question and you check your symptoms, all of the rest is free.
Chris - Let's talk about the AI (artificial intelligence) bit for a second then. So you're saying that you have got a clever system running here that can compare my symptoms, that I would just tap in and tell the app what I am experiencing and it would intuitively begin to work out what might be wrong with me?
Ali - That's correct.
Chris - Tell me how it works.
Ali - So it looks at a variety of probability of the combination of various symptoms and say what could possibly be wrong with you according to the combinations of the symptoms you have given it. No different than a chess player, for instance, playing chess. It looks at the probabilities of different moves and where that can end up. So we've launched a symptom checker that triages, so it does what a clinical nurse will do in a triage in an A & E and it will tell you whether you should go see a doctor or go to a pharmacy or the kind of stuff NHS 111 does, but it does it in an average of one minute. It's free, it's done by a machine rather than any human being involved and we published a paper when we launched it that shows that it's more accurate than a nurse and a doctor. And you would expect it to be because no human brain can look at billions of variations.
Chris - But if I may - the thing is I went to medical school for a long time to learn to ask people about things that they might not think to volunteer. So yes, if they're saying I've got this symptom and this symptom, but what your system can't do is to take a look at that pers - or can it - and spot the things that they haven't though are relevant but which, actually, are pretty important or are more important than the thing they think is wrong with them?
Ali - And you are absolutely right Chris. So it's a system that does nothing else but check with artificial intelligence and tell you what's wrong with you. You're right, it's not the right system for the kind of technology that exists today so that's we will let you know that you need to talk to one of our doctors, book and appointment, and within a few minutes a human doctor will appear on your screen and you will talk to a human doctor.
Chris - Well, you make the case very well for what happens in a country like the UK, a rich country, it has GPs on tap, it has an NHS, but there must be places in the world where this sort of technology could be very readily harnessed and bring enormous benefits over and above what anything you could achieve here.
Ali - That's correct. Precisely because of that Chris, we went to Rwanda, which is one of the poorest countries in the world and say that how can we give the same quality of care at the prices that the people of Rwanda can afford. And we launched in Rwanda about three weeks ago and the result has been amazing. Most people in Rwanda do have a mobile phone. It's early days yet but it's certainly our intention to try and put an affordable health care into the hands of everybody on earth.
Chris - I know I've spent a long time learning to talk to patients face to face but, if I'm now faced with talking to them on a screen where I can't physically reach out and touch them and the technology may be dubious, are doctors comfortable working like that - do they express any discomfort working that way?
Ali - No, they are very comfortable because first of all we train them, we vet them very carefully and make sure they are highly experienced doctors. We don't hire doctors who don't have an average of ten years experience and so on and so forth. Yut you're right, it is not a problem to be taken lightly but what is the alternative - think about it. In Britain one in five of us can't get to see a doctor that we want at the time we want. One in eight of us when we do so, and so on and so forth, but that is in Britain. In Rwanda or fifty percent of the world's population in developing countries there is no access, or very little access to healthcare. The alternative is much worse than the remote ability of getting to those patients.
Chris - And is this the direction in which you see healthcare going, or is this the next big healthcare revolution that you anticipate seeing?
Ali - Absolutely! I think what we're going to see in healthcare is what we've seen in every other area of human endeavour, where technology will come in and disrupt the old models of delivery and make it a lot better. What we are doing is just the very beginning of what can be done. You just look at what has happened in diagnostics, for instance, in the last ten years; it has improved at two times the rate of Moore's law. We will see the same improvement across the systems of delivery of healthcare and I think that soon we will do with healthcare what people like Google have done with information; make it affordable, accessible; put it in the hands of everybody on Earth. That is not a dream, it is an achievable.
Chris - And lastly Ali - what's to stop someone like me thinking well that's a blinking good idea and just copying it?
Ali - I would certainly hope you do because it is irrelevant who manages to put that into the hands of everybody. What matters to humanity is that our best brains, best talents, best resources, mobilise to solve one of the biggests challenges human beings have. The more people that participate in this endeavour the better for us all.
Chris - But I put it to you - if I'm on your app and it tells me in rural Rwanda, in the middle of nowhere, I'm having a heart attack really knowing that isn't going to change the game, is it, if I'm nowhere near a hospital that can help me?
Ali - Correct. But look you have to start somewhere right. It's like saying that if you put a car in my hand and I'm driving or you send me an ambulance but there is nothing on the other side and so on and so forth. Everything we do, every effort in technology starts somewhere and it gets better and better. So today we get you a doctor, tomorrow perhaps we can create the logistics to get you the drugs, and the day after we could do something else. There are so many people solving so many different areas of healthcare using technology that collectively, no-one on their own, collectively they will meld everything that is in existence in medicine today to create a completely new solution that would be miles better than what we have now. Just look at every other area from retail, to consumer shopping, to banking, what technology has done with it. And I'm sure healthcare will be another beneficiary.

51:12 - What would happen if I moved to Jupiter?
What would happen if I moved to Jupiter?
Kerstin Goepfrich put this question to Dr Stuart Higgins from Imperial College London...
Stuart - Okay, let's go to Jupiter.
Take the next left and proceed for four hundred and eighty-four million miles.
Stuart - Let's speed that up and pretend we could just teleport ourselves directly to Jupiter's gas surface. Jupiter is much bigger than the Earth; it has about three hundred and twenty times the mass - it's huge. Assuming we could live on Jupiter for fifty years and somehow survive the lack of oxygen, giant storms, and the fact that there's no real solid land to stand on, then the strong gravitational field of Jupiter's greater mass would have some peculiar effects.
Crucially, compared to a clock on the Earth, a clock on Jupiter would tick more slowly. According to Einstein's theory of relativity, time passes slower in a gravitational field. This is known as gravitational time dilation.
Kerstin - Being near a massive object makes time move more slowly. So on Jupiter, the big boy of our solar system, how much time would we save? On Facebook Aik suggested a hundred years. One point two three four five minutes was put forward by Martin. Stuart please don't leave me hanging any longer...
Stuart - Well, it's not much. For each second on Jupiter your wristwatch would be running roughly twenty nanoseconds slower than a clock left back on Earth. Over fifty years you'd end up being about thirty-one seconds younger compared to if you'd stayed on Earth. And yes, for general relativity fans, this is very much a simplification, not taking into account loads of other factors but it gives us an idea of the incredibly small size of this effect.
Kerstin - So a lot of effort for thirty-one seconds! But why do we even care about Einstein and all this time dilation?
Stuart - It turns out that even though the differences are tiny, they're big enough to cause huge problems with the global positioning system, GPS. The constellation of GPS satellites that orbit the Earth each have their own clock on board, which broadcasts its signal to receivers, such as your smartphone. By comparing how long it's taken the signal to reach you from different satellites, the system can work out where you are. But there's a problem, the clocks in space are further away from the Earth than your receiver is; they're in a weaker gravitational field. That means after taking into account other effects, time runs faster for the satellites and while the differences are tiny, over a single day it can build up so that your GPS receiver is wrong by a whopping ten kilometres.
Oh dear, I appear to be lost.
Luckily, the satellites have Einstein's equations built in so they account for gravitational time dilation.
- Previous Where do children get their intelligence?
- Next Practising Medicine









Comments
Add a comment