Decoding the Cancer Genome
Interview with
Andrew - What we set out to do was to try to understand what role a specific set of genes that occur in the genomes of all individuals, called Kinases, have on the progression of the disease (cancer). These cells are very interesting because they govern most of the molecular processes in the cell. They act like molecular switches, turning things on and off. Cancer cells are those that grow when they shouldn't, where they shouldn't and how they shouldn't and nearly all of these processes have a Kinase involved somewhere in the pathway that governs that process. We were interested to know which of those genes to think about in terms of drug targets. We knew also from the past 20 years of research that if you look at the genes known to be mutating, protein Kinases show up more frequently than any other gene family at the moment.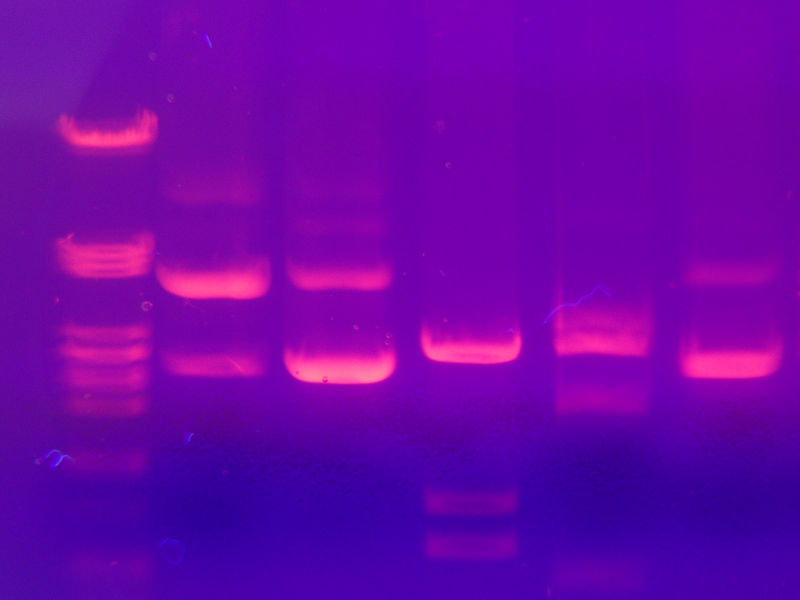 Kat - So they are the real bad guys?Andrew - At the moment they appear to be the bad guys we understand the most about. The linchpin for deciding to work on those genes, out of all the 20-odd thousand that exist in the human genome, was that it's the one gene family that we know how to make drugs against. There are several startling examples of understanding the genetics of a tumour via a mutated protein Kinase and developing a small molecule that has a high level of efficacy in patients. So we wanted to understand the genetics of cancer and also start a family where if we found something there would be shorter route to translation in terms of patient benefit.Kat - You have looked at 500 genes in 200 types of cancer. How do you go about looking at that many genes for that much information?Andrew - We used what will in a couple of years be called 'stone age' technology, the same technology we used to sequence the human genome; called Capillary Based Gene Sequencing. Out of those 500 genes we looked at all the bits that encode them, amplified them using a polymerase chain reaction from all 200 samples across these 500 genes, which works out to be about 10,000 fragments per sample, and sequenced them from both ends.Kat - That's a lot of work! How do you cope with that much information? Presumably you have incredible computers to process it all.Andrew - Yes, we have an excellent group of 14 people in the cancer genome project who are bioinformatitians. They are a brilliant group who organise the data and give it to us in terms we can understand. They actually allow us to find a single experiment amongst the millions that have been done, which is very important. It's collaboration between lab scientists, computer scientists and the people who integrate the information between the two.Kat - So what were you expecting to find?Andrew - Well, from the work that we had done earlier we found a frequently mutated Kinase called B-raf in the tumor type called melanoma. This particular Kinase is mutated in about 60% to 70% of this lethal disease. We were hoping to find the same sort of pattern when we look at Kinases across a broader set of cancers. If 60% of a gene is mutated in a tumour it would make a good drug target, if you can make a molecule to turn that gene off.So we when we started looking at these 200 cancers we quickly began to understand that this particular example looks like the exception rather than the rule. The rule looks like a more widely distributed set of mutations across a larger number of genes, so we found about 1000 mutations in 200 samples, and we believe about 100 of those are driving cancers in that group of 200.Kat - So this is more than you expected?Andrew - It's quite a bit more than I would have expected. We hoped it would be lots of spikes rather than this rumble of noise, because it's more tractable to deal with spikes in terms of therapeutic development.Kat - So do you think that means you've potentially more targets to have a go at?Andrew - I think that's exactly right. What it does is it opens up a window into understanding just how complex the disease is and that's a daunting prospective. I think what it also does is allow you to begin to integrate this information into understanding what processes, pathways and signalling circuitry is turned on or off in particular cancers, it may give you the opportunity to not only go after the gene itself but also the pathway.Cancer is a complex disease we can't get away from that so we're going to get in there, roll up our sleeves and get to grips with the ugly reality of it.Kat - So you've looked at Kinases, this particular group of signalling molecules. Are there any other molecules or family of molecules that are next on your hit list?Andrew - We started a study running towards the end of the Kinase study looking at another group of about 4000 genes. We're also going to use a larger number of tumours, about 100 cancers per set. This is comprised of essentially any gene family where there is already one member known to be mutated in cancer, promoting the idea that they may be clustered by family or by function. For example we know that DNA repair is not working particularly well in a lot of cancers. This would involve things like phosphatase, which turns things back off after Kinases turn them on, or other gene families that are involved in signalling pro-growth or pro-apoptosis cell growth division. These are all the usual suspects or at least as good as we can come up with on that list at the time.Kat - so that's going to keep you busy for a while!Andrew - Yes, sadly, I don't think we'll be working our way out of a job anytime soon.
Kat - So they are the real bad guys?Andrew - At the moment they appear to be the bad guys we understand the most about. The linchpin for deciding to work on those genes, out of all the 20-odd thousand that exist in the human genome, was that it's the one gene family that we know how to make drugs against. There are several startling examples of understanding the genetics of a tumour via a mutated protein Kinase and developing a small molecule that has a high level of efficacy in patients. So we wanted to understand the genetics of cancer and also start a family where if we found something there would be shorter route to translation in terms of patient benefit.Kat - You have looked at 500 genes in 200 types of cancer. How do you go about looking at that many genes for that much information?Andrew - We used what will in a couple of years be called 'stone age' technology, the same technology we used to sequence the human genome; called Capillary Based Gene Sequencing. Out of those 500 genes we looked at all the bits that encode them, amplified them using a polymerase chain reaction from all 200 samples across these 500 genes, which works out to be about 10,000 fragments per sample, and sequenced them from both ends.Kat - That's a lot of work! How do you cope with that much information? Presumably you have incredible computers to process it all.Andrew - Yes, we have an excellent group of 14 people in the cancer genome project who are bioinformatitians. They are a brilliant group who organise the data and give it to us in terms we can understand. They actually allow us to find a single experiment amongst the millions that have been done, which is very important. It's collaboration between lab scientists, computer scientists and the people who integrate the information between the two.Kat - So what were you expecting to find?Andrew - Well, from the work that we had done earlier we found a frequently mutated Kinase called B-raf in the tumor type called melanoma. This particular Kinase is mutated in about 60% to 70% of this lethal disease. We were hoping to find the same sort of pattern when we look at Kinases across a broader set of cancers. If 60% of a gene is mutated in a tumour it would make a good drug target, if you can make a molecule to turn that gene off.So we when we started looking at these 200 cancers we quickly began to understand that this particular example looks like the exception rather than the rule. The rule looks like a more widely distributed set of mutations across a larger number of genes, so we found about 1000 mutations in 200 samples, and we believe about 100 of those are driving cancers in that group of 200.Kat - So this is more than you expected?Andrew - It's quite a bit more than I would have expected. We hoped it would be lots of spikes rather than this rumble of noise, because it's more tractable to deal with spikes in terms of therapeutic development.Kat - So do you think that means you've potentially more targets to have a go at?Andrew - I think that's exactly right. What it does is it opens up a window into understanding just how complex the disease is and that's a daunting prospective. I think what it also does is allow you to begin to integrate this information into understanding what processes, pathways and signalling circuitry is turned on or off in particular cancers, it may give you the opportunity to not only go after the gene itself but also the pathway.Cancer is a complex disease we can't get away from that so we're going to get in there, roll up our sleeves and get to grips with the ugly reality of it.Kat - So you've looked at Kinases, this particular group of signalling molecules. Are there any other molecules or family of molecules that are next on your hit list?Andrew - We started a study running towards the end of the Kinase study looking at another group of about 4000 genes. We're also going to use a larger number of tumours, about 100 cancers per set. This is comprised of essentially any gene family where there is already one member known to be mutated in cancer, promoting the idea that they may be clustered by family or by function. For example we know that DNA repair is not working particularly well in a lot of cancers. This would involve things like phosphatase, which turns things back off after Kinases turn them on, or other gene families that are involved in signalling pro-growth or pro-apoptosis cell growth division. These are all the usual suspects or at least as good as we can come up with on that list at the time.Kat - so that's going to keep you busy for a while!Andrew - Yes, sadly, I don't think we'll be working our way out of a job anytime soon.
- Previous Cancer and Stem Cells
- Next Science Update - Puberty and Death










Comments
Add a comment