Developing an HIV Vaccine
Interview with
Chris - When HIV was first discovered about 30 years ago, there was significant optimism that we'd soon have a vaccine with which we could tackle that problem. But three decades later, there still isn't one and to explain why, and how he's trying to solve the problem, from the National Institute of Allergy and Infectious Diseases in Maryland, is Peter Kwong. Hello, Peter.
Peter - Hi, Chris. How are you doing?
Chris - Very well, thank you. So what's the problem here? Why haven't we got a vaccine yet?
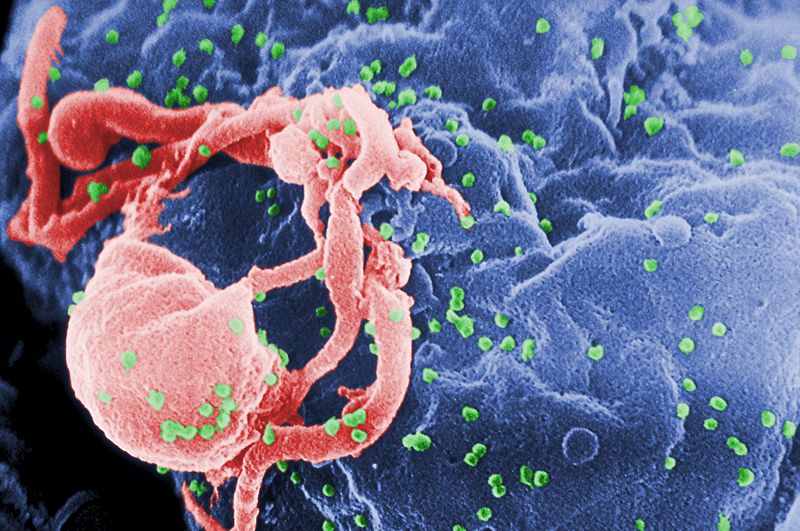
Peter - I think the reasons why we don't have the vaccine relate in part to some of the things that Mark was telling Kat, that is, the virus infects the human host, and that generate an immune response which is just not that effective. There's all this cellular machinery that the virus uses to cloak itself in different ways and moreover, the virus is able to integrate in such a way into T-cells that hides itself from the immune system. So you have the virus hiding out and you also have it provoking a particular response that is not so effective. So for both of those two reasons, the fact that it hides and it also provokes an inactive immune response, that has really complicated the search for a vaccine. What we really want are these broadly neutralising antibodies, antibodies who generally fight viruses and lead to good vaccines.
Chris - So what are you trying to do to combat this problem?
 Peter - Well there's been a lot of research to try to figure out what antibodies could actually effectively fight the virus. And for a long time, people thought, "There's just aren't any, people's immune systems don't effectively fight the virus". Recently however, there's been a rash of broadly neutralising antibodies that had been found in infected individuals. So if you take a screen of several thousand people, the top 1% or so turn out to have very, very good effective antibodies that can fight off the virus. And so, there's been a change in thinking from the idea that the human immune system is unable to fight the virus. And now, the change of thinking is that the human immune system can fight off the virus, or at least make broadly neutralising antibodies. It just takes it a bit of time to figure out how to do it. There's road blocks to developing those things. But fortunately for us, if we're immunising people, we have potentially a lot of time to teach the immune system, before you actually get exposed to the virus.
Peter - Well there's been a lot of research to try to figure out what antibodies could actually effectively fight the virus. And for a long time, people thought, "There's just aren't any, people's immune systems don't effectively fight the virus". Recently however, there's been a rash of broadly neutralising antibodies that had been found in infected individuals. So if you take a screen of several thousand people, the top 1% or so turn out to have very, very good effective antibodies that can fight off the virus. And so, there's been a change in thinking from the idea that the human immune system is unable to fight the virus. And now, the change of thinking is that the human immune system can fight off the virus, or at least make broadly neutralising antibodies. It just takes it a bit of time to figure out how to do it. There's road blocks to developing those things. But fortunately for us, if we're immunising people, we have potentially a lot of time to teach the immune system, before you actually get exposed to the virus.
Chris - So in your view, the way in which we need to tackle HIV is to prevent people becoming infected in the first place. So we've got to make people make that broadly neutralising immune response from a vaccine so that that repertoire of immune responses is there waiting in the uninfected person. So if they're challenged with HIV, they can fight it off because if we go in and they've already got it, it's too late.
Peter - Absolutely, Chris. The problem with a vaccine in general is that you can only fight off the virus with the vaccination, prior to infection. And so, it appears that most viruses can't be solved with drugs. If one has the flu for example, there aren't that many drugs that one can take that maybe ameliorate the disease a little bit, but that's very difficult. What's much more effective is if you come in beforehand with a vaccine to teach the immune system to fight off the virus when we have that moment of infection. And the reason for that is that, when you're initially infected, maybe only one virion, two virions, a very little number of virions will cross over. And so, if you have a vaccine that can kill, say, 99% of those, then one can protect 99% of the people that might be infected by one or so virion. On the other hand, once you're infected, you might have billions of virions. And so, if a person has a treatment that might kill 99% of them, a billion virions, if you still kill off 99%, you have 10 million left and so, one doesn't have much of an effect on an infected individual. You really want to get it at the time of infection.
 Chris - Sounding rather like a TV advert for certain kinds of surface cleaning agent! What do we think is going to take then in order to produce a vaccine that will elicit these kinds of broadly neutralising responses? What's got to go into that vaccine? What sort of response are we trying to drive against - what target on the virus?
Chris - Sounding rather like a TV advert for certain kinds of surface cleaning agent! What do we think is going to take then in order to produce a vaccine that will elicit these kinds of broadly neutralising responses? What's got to go into that vaccine? What sort of response are we trying to drive against - what target on the virus?
Peter - There are two really exciting things that have come out lately in terms of how to develop a vaccine. The first is that there was just a trial, the RV144 trial that was conducted in Thailand, where they're actually stimulated with gp120 envelope glycoproteins and found a response that's able to prevent infection or reduce the rate of infection by about 30%.
Chris - This is using the outer coat of the virus - gp120 is part of the surface marker on the virus, isn't it?
Peter - Absolutely and so, before this, people thought, "An HIV vaccine, that's just going to be impossible. That's something like going to Pluto or something. It's not something that we can actually do." With this human trial, they actually showed then HIV vaccine is possible, actually made one that's about 30% effective. Now 30% isn't that great, but if one just increases the efficacy by a factor of three, you'd be up to around 90%. So, they've already shown that it's possible and the question is how to improve it. Now, when we know that human immune systems can generate these broadly neutralising antibodies, those antibodies basically become templates for vaccine design. You basically have a useful solution, something that the human immune system can make on its own that tells you what you want to get in a vaccine. And so, there's potential sites of vulnerability, places on the virus that the human immune system can attack. Now there's just a couple of them, like the CD4 binding site, places where the virus latches on to the cell, that's the site of CD4 attachment, or some types of antibodies that are called quaternary specific, those things that only functionally work with respect to the trimer. What that means is that there are absolutely ways that the human immune system can neutralise the virus, but they're relatively complex, and we're trying to figure out exactly how to make more antibodies. But we already know that the human immune system can make these antibodies. So it's just a matter of figuring out how to trigger the human immune system to do what we already know what it can do, which is to make this effective neutralising antibodies.
Chris - How close are we to making that happen because it sounds from what you're saying, like you're thinking quite optimistically?
 Peter - Absolutely. There's an air of optimism, but then you're asking for the timeframe on that and I think that that becomes a little bit difficult to say because just the trials alone, once we come up with something that teaches the immune system of an animal to make broadly neutralising antibodies, it's going to be at least 5 years from that stage to actually getting to work and getting into humans, and going to phase 1, 2, or 3 trials. So, the actual vaccination development process does take decades potentially, but what we're really excited about is the first couple of steps where we can show in the laboratory that this is actually going to work. And those experiments are going forwards and once you know it's in the laboratory working, then it's just a matter of time before it actually becomes a working product.
Peter - Absolutely. There's an air of optimism, but then you're asking for the timeframe on that and I think that that becomes a little bit difficult to say because just the trials alone, once we come up with something that teaches the immune system of an animal to make broadly neutralising antibodies, it's going to be at least 5 years from that stage to actually getting to work and getting into humans, and going to phase 1, 2, or 3 trials. So, the actual vaccination development process does take decades potentially, but what we're really excited about is the first couple of steps where we can show in the laboratory that this is actually going to work. And those experiments are going forwards and once you know it's in the laboratory working, then it's just a matter of time before it actually becomes a working product.










Comments
Add a comment