Dismantling brain cells
Interview with
Though the idea of a long sleep may sound pretty tempting, animals actually put themselves through an awful lot. They are continually cooling and reheating their bodies, putting huge stress on their organs, and some even make themselves diabetic. Hibernation is clearly no picnic, and things get even 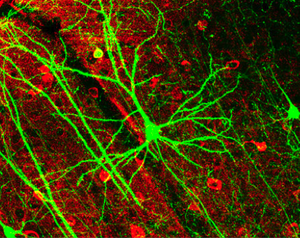 worse as, in an attempt to save energy, animals will dismantle the synapses in their brains. These are the parts of the neuron that send and receive signals and without them we're all pretty useless. But what's even more amazing is that when it's time to "wake up" they'll put them back together again, just as they were. Professor Giovanna Mallucci is a clinical neuroscientist at Cambridge University and she explains to Connie Orbach how this actually works.
worse as, in an attempt to save energy, animals will dismantle the synapses in their brains. These are the parts of the neuron that send and receive signals and without them we're all pretty useless. But what's even more amazing is that when it's time to "wake up" they'll put them back together again, just as they were. Professor Giovanna Mallucci is a clinical neuroscientist at Cambridge University and she explains to Connie Orbach how this actually works.
Giovanna - I think you've heard already from our other speakers, that there's lots of processes that slow down and are shut down for hibernation including metabolism. And one way to save energy is to stop the brain using its energy and the dismantling of synaptic connections between brain cells is a way of doing that. What happens is, on cooling there is a retraction of what we call the "dendritic arbour", you know all the connections and branches of a brain cell that's connecting to another and the actual contacts - it's like unplugging a plug from its socket, they are just removed so that no energy flows. When they rewarm there's a signal to reconnect these structures; how that exactly happens is absolutely not known and very, very interesting to us but we do know a lot about the processes that drive that regenerative capacity.
Connie - Is this happening all over the brain?
Giovanna - Yes, it's happening all over the brain and all of us all the time. So there's a balance between pruning and generation or regeneration to maintain a sort of status quo and learning and memory need new synapses and then you prune and get rid of all your excess synapses when you sleep and other conditions. But the capacity for regenerating synapses and refreshing them is part of repair and it's called "structural synaptic plasticity."
Connie - So let me just get this right. So what's happening with animals in hibernation is a much more extreme version of actually something that's happening all the time in humans and animals?
Giovanna - Correct, that's exactly right.
Connie - So how have you been using this then in your work?
Giovanna - So we know that in neurodegenerative diseases like Alzheimer's, which is the prototypical disease but also many of the others. The earliest thing that happens, before you get the brain cell degeneration, is that synapses are lost and as synapses are lost memory goes down - what we call cognitive function goes down, and it's just not clear why this is early loss of synapses which is such an important stage in these diseases, and it's important a) because it give you symptoms and b) because it's reversible. So that's the stage before the brain cells have died, before the neurons have died when, actually, if you can increase synapse number you can restore memory so it's a very attractive, targetable point of intervention. And our starting hypothesis was that the reason that synapses are lost early in Alzheimer's disease and early in Parkinson's disease and other disorders is because there's a failure of this regenerative capacity that is part of our normal structural plasticity. We used hibernation or induced laboratory hibernation in mice to test the ability of synapses to regenerate themselves in mouse neurodegeneration models.
Connie - And what did you find out - what's happening?
Giovanna - So first of all we found very interestingly that mice which don't normally hibernate, can hibernate in all the ways that you would normally expect. So if you cool them: they'll drop their body temperature, they'll dismantle their synapses and they'll go into torpor and then, when you re-warm them, they come completely back to normal again. And what we found out was that normal mice dismantle and reassemble their synapses but the mice that we used that had neurodegeneration models - that's Alzheimer type mice, and mice with prion disease - that's another neurodegenerative disease. They failed to reassemble their synapses so they could unplug the plugs but they couldn't put them back in again and this lack of degenerative capacity gives us a good idea of why there's such an early loss in synapses.
Connie - Did you get a bit deeper into this? Did you get to see the protein that's involved - is that right?
Giovanna - Yes we did. So hibernating and cooling does two things to you: it shuts down metabolism and it shuts down protein synthesis, but there's a group of proteins that are upregulated and these are called "cold-shock proteins," and they're a relatively new family of proteins. And one of these which is called "RBM3", which is RNA Binding Motif Protein 3, is highly expressed in the brain and by being upregulated during hibernation that protein keeps a number of really important critical Messenger RNAs, that you need for survival, ready to make into proteins when you wake up. And we found out that RBM3 is failing in the Alzheimer's brain, and if we put it back in, we can rescue them.
Connie - So you found this protein, RBM3 - where do you go now?
Giovanna - So, we didn't find the protein; I mean the proteins a known cold shock protein. What we've done is associate it with the failure of structural plasticity in neurodegenerative disease in Alzheimer type mouse models and what we now want to do is understand the relevance for human disease. Because what we found in the mice is that if you put the protein back in it's incredibly protective, it gives them new synapses, it stops them getting neurodegeneration, it stops them getting memory loss, and it protects them in the long term and you can do that by either cooling the mice early to boost their indodgenous or their own RBM3 levels, or by putting it in artificially. So now, obviously, this is a way in for neuroprotection for human disease but cooling itself is not realistic or practical in the long term. It is used medically; it's used in newborn babies that have had hypoxic damage; it's used in post-stroke and it's used in cardiac surgery, and in many forms of neurosurgery. So we thinks that that's acting through RBM3 and our ideal would be to be able to manipulate RBM3 levels for protection without having to cool.
- Previous Plants hibernate too!
- Next Harry Potter style newspapers created










Comments
Add a comment