Foetal Gene Therapy
Interview with
Chris - With genetic disorders, one concern is that the damage caused by a particular disease could peak early on in development, even while a baby is still in the womb. With such conditions, gene therapy before birth could improve a child's life expectancy. This is a field that Simon Waddington from University College London is working on. Hello, Simon.
Simon - Hello, there.
 Chris - What's your research actually looking at? What are you doing?
Chris - What's your research actually looking at? What are you doing?
Simon - One of the things that we look into is the concept of delivering the genes in-utero, in other words before birth. There are many diseases, many genetic diseases, where the onset is very early and can be lethal. So in other words, the baby actually is born with a genetic disease and that genetic disease has already damaged the baby's tissues to the extent that you can't reverse the illness. And so, what we're looking at is the idea of actually treating or preventing the disease from ever occurring by transplanting of the genes while the baby is in the mother's tummy.
Chris - How would you make the diagnosis? How would you know the baby has or is destined to get the condition?
Simon - That is a very interesting question. I think the first thing to say about this is that quite often, a family has a baby, finds out the baby has a genetic disease, and the child may then die. And then, we know of course that the parents are carriers of the disease and so, that actually is one way to then start to screen for the disease. Another thing to say is that for many diseases that are early and lethal, genetic testing is not performed because there is no treatment and so, there is not the same sort of driver to actually test the whole population.
However, the improvements that we see in genetic testing now - the speed of the technology and the accessibility of the technology - means that we can screen for a lot more genetic diseases a lot less expensively. The other thing is that over the past couple of years, there have been some very exciting developments where you can actually isolate cells that are circulating in the mother's circulation but they actually come from the foetus. And so, you can isolate those cells and then you can actually test the genetics of the foetus without actually interfering, sticking a needle into the foetus, at all.
Chris - So you could do genetic diagnosis from nothing more than just a maternal blood sample.
Simon - That's right.
Chris - This will give you some warning especially if you know it might be an at risk population.
Simon - Yes, that's right.
Chris - But is doing gene therapy on an unborn baby just the same as doing gene therapy on a person who's actually say, an adult? Is there a different constraint entirely in trying to do that? Will the techniques that we're investigating in petri-dishes and in adults actually apply in utero?
Simon - In one sense, at least in our research, it's easier to deliver the genes to a foetus than it is to an adult. With an adult, the immune system has already seen these viruses and you've actually developed an anti-virus immunity. One has to bear in mind that many gene therapy vectors are based upon an archetypal virus. So that's one problem that we avoid by going in early into the foetus. Another point is actually that you can put more copies, more genes, into the foetus and therefore, you might actually be able to get a wider distribution in the foetus too.
But I think that one of the things that we have to consider is that you're actually dealing with two patients of course. You've got to consider the health of the mother as well as the foetus and this is something that we've obviously been considering in our research for the past 10 years.
Chris - How do you do your research? It's already a very emotionally charged area - looking at pregnancy and children that haven't been born yet that might have a problem. Is there an animal model you can induce which will give you a faithful representation of what might happen in a human?
Simon - We work primarily with mouse models and so, actually we're able to deliver the genes into the foetal mouse by the same routes as one would be able to do a blood sample in a foetal human. Obviously the mouse model is a long way away from the human in terms of physiology but the principles are the same, and I think we're seeing this through the various gene therapy trials that are being performed anyway. Obviously, you have to test the safety of these in lower animal models before you scale it up to human beings.
Chris - What techniques are you investigating that you're trying to use? What gene transfer techniques are you investigating that you're trying to use?
Simon - What we're looking at, for example, is that we've been interested in neurodegenerative diseases. One particular interest of ours is Gaucher's disease which is a deficiency in the enzyme glucocerebrosidase. Humans with the severe form of this disease, called neuronopathic Gaucher disease, will only expect to live for 2 years after birth.
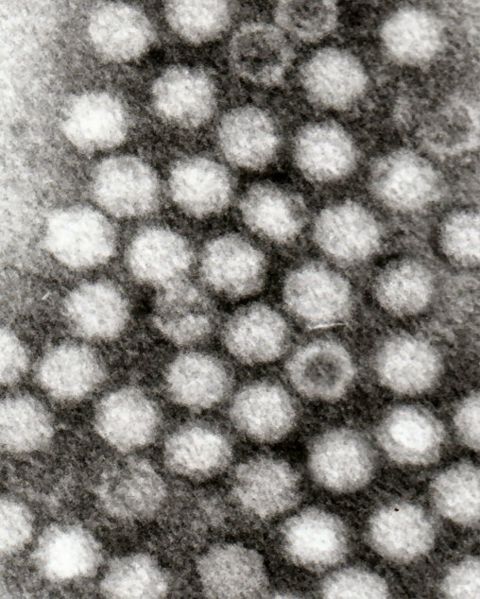 We have a mouse model of this where the mice only lived for 14 days after birth. We're using a vector called AAV9 which is Adeno-Associated Virus 9. People found a couple of years ago that when you injected this in the circulation, you could cross the blood-brain barrier and could actually deliver the genes to the central and peripheral nervous system. This is the main problem with neuronopathic Gaucher disease. you can't get anything into the brain. We're hoping to be able to deliver additional copies of glucocerebrosidase in order to at least cure the mouse model.
We have a mouse model of this where the mice only lived for 14 days after birth. We're using a vector called AAV9 which is Adeno-Associated Virus 9. People found a couple of years ago that when you injected this in the circulation, you could cross the blood-brain barrier and could actually deliver the genes to the central and peripheral nervous system. This is the main problem with neuronopathic Gaucher disease. you can't get anything into the brain. We're hoping to be able to deliver additional copies of glucocerebrosidase in order to at least cure the mouse model.
Chris - And the fact that you're going into a brain which is smaller than it will be when you're trying to cure a much bigger child or adult makes it easier because you're able to hit cells when they're at the stem cell stage, so then all of the daughter cells will inherit that change.
Simon - Well the thing is with the brain is that at birth, you're not actually adding any more cells or not adding many more cells to your brain. Your neurons are already in place so we are using a vector that doesn't integrate itself into the host genome, but actually because your brain is no longer dividing, these vectors can then stay around for the rest of the lifetime.
Chris - So you should get lifelong protection?
Simon - That's right, yes.
Chris - Any risks?
Simon - Well, I think as a community, we've always been very aware of any potential risks. So, the risks in terms of foetal gene transfer would be that you are also putting a needle into the mum and there's always a small, but still actual risk of damaging the foetus or causing birth.
Chris - Are you physically injecting this into the bloodstream of the foetus? Is that what you've got to do to get it into the brain? How are you doing that?
Simon - That's right. One of the big problems with brain gene therapy has been that you have to stick a needle into the brain in multiple sites because it doesn't spread through the brain naturally. Whereas these new and exciting vectors, you can put it into the bloodstream and then it can actually deliver genes throughout the entire brain and to the spinal cord.
There's some exciting work coming out on spinal muscular atrophy in mouse models and actually in larger animal models. In the mouse model, actually they cured the disease - the spinal muscular atrophy - which was completely stunning. And so, these researchers are actually now looking at the large models before considering clinical trials.
- Previous A Virus to Combat Cancer
- Next Gene Therapy for Inherited Blindness










Comments
Add a comment