Screening Blood for Cancer
Interview with
Historically, cancer scientists have studied tumours by taking samples from 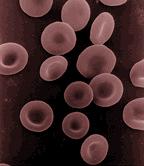 them and then looking at them under the microscope, or they've used scans to pinpoint where cancers are. The problem with this is that to do either of these things requires the cancer to be of a sufficient detectable size. By the time it is detectable, often, it's usually very advanced. But now, researchers at Cancer Research UK's Cambridge Institute are pioneering a way to track tumours using fragments of their DNA that they release into the bloodstream. This means that the behaviour and the response of the cancers to treatment and even tiny tumours can be followed up. Chris Smith went along to see Tim Forshew, one of the scientists behind this new technique, to see how it works.
them and then looking at them under the microscope, or they've used scans to pinpoint where cancers are. The problem with this is that to do either of these things requires the cancer to be of a sufficient detectable size. By the time it is detectable, often, it's usually very advanced. But now, researchers at Cancer Research UK's Cambridge Institute are pioneering a way to track tumours using fragments of their DNA that they release into the bloodstream. This means that the behaviour and the response of the cancers to treatment and even tiny tumours can be followed up. Chris Smith went along to see Tim Forshew, one of the scientists behind this new technique, to see how it works.
Tim - It's been known for a long time that if you take a blood sample and you centrifuge it to get rid of the cells, you get what's known as blood plasma. And if you look in this blood plasma, you'll find copies of your genome floating around cell free. So, this is you're instruction manual. It's equally been known that at least in certain cancer patients, you'll find higher levels of this DNA floating around, cell free. And so, it's been hoped that you could use this as a way of detecting or monitoring and analysing cancer.
Chris - Is that genetic material intact? Could you read it like a book with all of the pages in sequence, or is it broken up like someone has shaken the book and all the pages have come adrift?
Tim - It's not intact and that's been one of the biggest challenges. So, these instructions are typically something in the region of 150 to 160 letters in length. So, we've got very small fragmented bits of DNA and very few copies of this DNA floating around in the blood.
Chris - Roughly, how much is in there?
Tim - So, in healthy individual, you'll have somewhere in the region of 2,000 copies of your instruction manual floating around in 1 millilitre of blood plasma. In someone that's got cancer, you may end up with one or two copies of your cancer instruction floating around or may have many copies of your cancer instructions floating around.
Chris - How are you going to read then all these mixed up DNA which is basically 160 letters long out 3 billion in the average person and put it back together? So, you're putting all the pages back in the book in the right sequence.
Tim - So, for some time now, people have had methods where they can look for one particular fault that is known to cause cancer or maybe a couple of faults. But the focus of our research has been to see if we can actually, as you say, read these instructions and look at large regions of the genome and try and understand what is going wrong in cancer and see if we can detect or monitor cancer through looking in the blood. So, we've been doing this with an approach called Next Generation Sequencing. If you come through here, then I can show you the machines we've been using.
So, this is one of our Next Generation Sequencing machines, and the way that we use this is we first take a blood plasma sample and we extract the DNA from this. Then we use a process called the polymerase chain reaction, or PCR, and this is a process that allows you to copy just certain parts of your instruction manual. So, to do this, you design something called primers which are short bits of DNA which you target to the specific - in our case, cancer - gene that we would like to read. You use these to pick out and amplify just certain parts of the instruction manual that you're keen to analyse. Then what you do is you take these amplified copies of your instruction manual and you put it on to one of these next generation sequencing machines. This then allows you to go through and read letter by letter all of these instructions and try and find where faults may lie, where cancer-specific changes are.
Chris - So, some of the genes that are in the person's cancers have got genetic spelling mistakes, for want of a better phrase, and that makes the gene misfunction - go wrong - and that contributes to them having cancer or to the way their cancer behaves.
Tim - Exactly, right. So, cancer is essentially a fault with your instruction manual and it's where you get faults that give an advantage to a cell. This cell will then grow more than it should. By finding these faulty instructions, we have a way of looking in blood and understanding what's going wrong in the cancer and potentially, working out how big the cancer is, or how well your treatment is working, by quantifying how much of these faulty instructions are floating around.
Chris - And so equally, if someone has a certain gene that's gone wrong that leads to their cancer not responding to a certain drug, you're going to see that and that means you can predict that happening before the person even realizes it, and so, you could change the drug treatment for example.
Tim - This is certainly what we're hoping. So, we need to do more research in understanding different types of cancer, how much of this DNA is being released. But certainly, from the early results that we and other groups around the world are gettingg, it suggests that at least in certain types of cancer, you will, as you say, be able to understand what's going wrong in the cancer before you can even necessarily see it through other processes. And then start to tailor the way that you treat an individual patient.
Chris - And monitor their response going forward.
Tim - Absolutely. So, once you found these particular genetic changes that are floating around in the blood, we hope that, again, for at least certain types of cancer, you'll be able to see if a mutation is decreasing and your treatment is being successful, or if the levels are increasing and your treatment should potentially be changed. And indeed, whether new mutations, new faulty instructions are appearing, suggesting that the cancer has evolved and you now need a different treatment.
Chris - I suppose this must give you as a scientists a totally new insight into cancer though because where previously someone might have been able to give you a little bit of one part of one cancer from one person. Now, if you take just a blood sample, which is going to be better for the patient, you're going to get a cross section of potentially all of the tumours including those tumours that have spread around their body all at once.
Tim - Absolutely. So, the challenge is, how much of this DNA is released and this is still something we're assessing. But assuming sufficient quantities are released, then as you say, it allows you to profile different parts of the tumour and equally, throughout the course of an individual's treatment. So, where getting a biopsy is often not even possible, with blood, you can take blood samples very regularly and start to assess how a tumour is changing.
Chris - It's almost like a liquid biopsy.
Tim - Absolutely. So, this is the term that we're starting to use for it.
- Previous Cancer Screening Tools
- Next What is Cancer?










Comments
Add a comment