Yeast Leads the Way for New Drugs
Interview with
In tropical climates, parasitic infections such as Malaria are a huge problem and new drugs need to be continually developed to fight the disease. Now a new screening method for potential drugs has been developed using yeast to help identify effective compounds.
To find out more, we're joined by Dr Elizabeth Bilsland from the Cambridge Systems Biology Centre.
Chris - So first of all, how do you find anti-parasitic drugs in the first 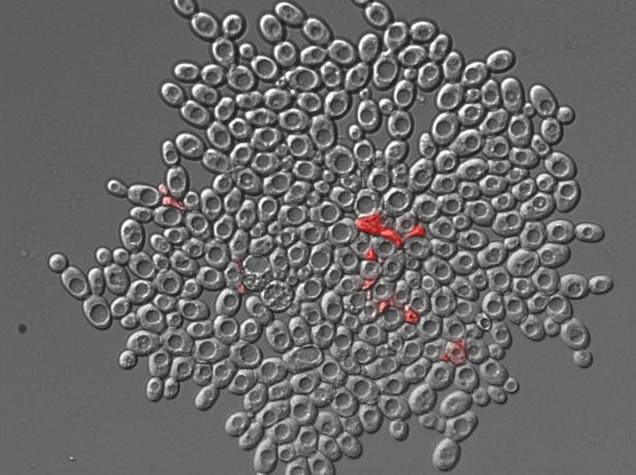 place using traditional methods? What's the usual way of doing this?
place using traditional methods? What's the usual way of doing this?
Elizabeth - Companies like GlaxoSmithKline and Novartis, they cultivate their parasites in the lab and that is possible for the African malaria so Plasmodium falciparum and treat them with loads of different chemicals. So, they have hundreds of thousands of different chemical compounds that they treat these parasites with and see what survives and what doesn't, and then for the best candidate, they test against toxicity in human cells.
Chris - Yes, I was going to say, it doesn't sound like a quick thing to do because then you can try it against the parasite, but then you've got to prove that the drug is toxic for the parasite, but safe for the host, the human?
Elizabeth - For the human, exactly.
Chris - So, you've got two rounds of testing to do for everything?
Elizabeth - Yes, and it is with the parasites that most of the work is being done and still we wonder if it's possible to do the highest throughput with the current methods. But there are several different parasites like Plasmodium vivax that cannot be cultivated in a lab or cannot have a full cycle of cultivation in the lab.
Chris - This is one of the other strains of malaria, isn't it?
Elizabeth - Yes, another strain of malaria that affects South America and Southeast Asia. It's the most widespread form of malaria, and the biology of that parasite is very different from the African malaria. But you just adapt the drugs from the falciparum malaria to the vivax, and hope that it works.
 Chris - And it may not necessarily be the best solution to the problem?
Chris - And it may not necessarily be the best solution to the problem?
Elizabeth - No. If for example, it does not target the liver stages then there are the recurrent stages of the vivax malaria.
Chris - I see. So, what have your group come up with as an alternative which solves a lot of those problems?
Elizabeth - We engineer strains where we remove genes that are essential for yeast to survive and replace those with genes that are essential for the Plasmodium to survive, or for the parasite, it causes sleeping sickness or chagas disease, or schistosomiasis. And we also did the same, replacing the same gene with a human gene. The idea is that we can grow the yeast strains in a way, grow them in a tube, treat them with the drug and see if the yeast with a parasite gene dies, but not the yeast with a human gene.
Chris - So, you're turning the yeast into a sort of surrogate parasite - so, by putting the parasite genes into the yeast and then testing those drugs on the yeast, if the yeast dies off with the parasite gene, that's good? When it's got the human equivalent, it stays safe, that's good, and it means you can do this much more quickly because you're growing yeast which is easy to grow?
Elizabeth - And from the start of the experiment, we have a direct measure of toxicity. So, we know that it's not having the possible side effects in humans. We know that the drug goes into the living organism, and we know which target is hitting because when you treat the entire parasite, you don't know how the drug is acting at all, so you can't optimise the drug if you don't know what it's hitting.
Chris - Is it working? Have you got some compounds out of this that prove this technique does work?
Elizabeth - Yes, definitely. In the yeast strain, we selected for example, 36 compounds that kill the yeast with the Trypanosoma brucei that's the agent that causes sleeping sickness. So, out of these 36 compounds, we tested them in purified parasites in the lab and we saw that 60% of them actually killed the parasite at 10 micromolar. With the same concentration of drug, if you test it straight in a parasite, you would have about 0.1% of hit rate. So, from 0.1% to 60%, I think that it's quite a good improvement. In the cases of parasites that you can cultivate easily in the lab, maybe that's not so important, but with the case of vivax malaria (that's a South American malaria), if you want to test if the drug is working, you have to be based on the area where that malaria is endemic, extract blood from about 50 patients infected with malaria, purify the parasite, treat that with the drug, and see if it works.
So, to have 50 sick volunteers for each drug, it would really not be realistic, but if you select 15 candidates in drugs then you can start to consider. And that's the stage that we are at the moment. We have some drugs that are in a state that we're going to take to the lab in Manaus with a collaborator from Brazil.
Chris - Wonderful piece of news, given that there are something like 500 million cases of malaria every year and perhaps as many as a million deaths. And also, coming in the year when we're celebrating 200 years since the birth of Dr. David Livingston who was of course the famous missionary who got malaria himself 27 times, I'm told. That's Elizabeth Bilsland from Cambridge University and she published that work this week in the journal, Open Biology.










Comments
Add a comment