New breakthroughs enabling rapid reading of DNA sequences promise to deliver a revolution in healthcare and are a powerful weapon in the fight against the hospital superbug, a meeting in London concluded last week.
Since the human genome project finished in 2003, sequencing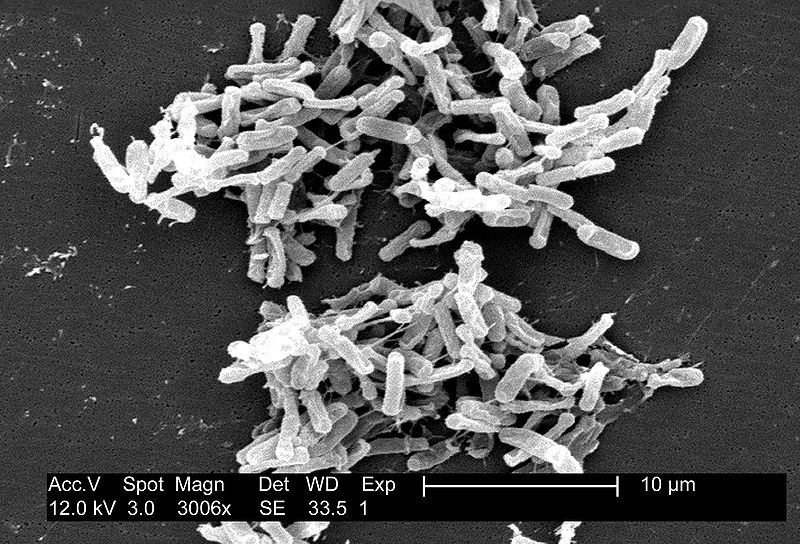 technology has taken a huge leap forward. Not only can we study the genome of a single human, now millions of organisms' genomes can be sequenced and analysed at once. These new techniques make up the field of meta-genomics, and using them we can study microbial communities to a level of detail which was previously impossible.
technology has taken a huge leap forward. Not only can we study the genome of a single human, now millions of organisms' genomes can be sequenced and analysed at once. These new techniques make up the field of meta-genomics, and using them we can study microbial communities to a level of detail which was previously impossible.
It is becoming increasingly clear that the communities of microorganisms that live inside us, and cover practically everything we interact with, have a huge effect on our health. Studies have shown that the bacteria in and around our bodies can affect how easily we put on weight, our mental state, how drugs interact with our bodies, and even how likely we are to be bitten by mosquitoes.
A meeting held in the UK Department of Health this week focused on how progress in meta-genomics could be used to understand how bacteria move around hospitals, and how this could help us understand how superbugs evolve and spread.
Dr Jack Gilbert, from Argonne National Laboratories in Illinois, is running a study of microbial populations in hospitals and people. Using meta-genomics, Gilbert's group is able to sequence the genomes of all of the microorganisms in a hospital room - on all of the surfaces, on and within the patients, and even organisms that the staff are carrying. Using this data he claims we can learn "how they interact with you as a host, and how they can survive in the environment". Public health officials are hoping that this knowledge will show us exactly how these super-bugs are spreading.
Currently, we aren't sure who is spreading superbug infections, whether it is patients transmitting them amongst themselves from from one bed occupant to the next, if hospital staff are the culprits, or if the bacteria are sneaking in some other way, in non-symptomatic carriers or perhaps living in the patients all along waiting to emerge at an opportune moment. Soon we'll find out what these mechanisms of bacterial - including superbug - spread actually are.
Studies on the microbial communities that live in our guts - called our 'personal microbiome' have already provided some interesting findings. Antibiotic resistant infections such as Clostridium difficile (C. diff), and inflammatory conditions including irritable bowel syndrome (IBS), have been tackled from a microbiome perspective. Doctors have replaced patients' gut bacteria with samples from a healthy person's faeces in a so-called 'poo transplant'. This might seem unpalatable, but Dr Julian Parkhill Head of Pathogen Genomics at the Sanger Institute in Cambridge said "the results were stunning" in an experiment comparing vancomycin (a powerful antibiotic) to poo transplants when treating C. diff infections - the poo transplant had a much greater success rate than the antibiotic.
Through studies like this scientists and doctors are starting to realise that some problems cannot be solved by focusing on single pathogens. Complex inflammatory diseases like IBS, obesity and Crohn's disease aren't caused by a single pathogen, but might be influenced by our personal microbiomes. Likewise, hospital superbugs like MRSA and C. diff might be best tackled by looking in a broader microbiome context.
Jack Gilbert is hoping to discover which combinations of microorganisms might increase your susceptibility to superbug infections. He's hoping this knowledge might be used to identify patients at higher risk of picking up an infection in hospital, or those who might be bringing in potentially dangerous bacteria.
But this experiment isn't limited to personal microbiomes; they are also looking at the bacteria present in the physical environment around a hospital. Dr Gilbert explained that from previous experiments on environmental microbiomes, things like opening a window or owning a dog can drastically affect the composition of the microbiome.
Understanding the dynamics of microbial communities in a hospital will be particularly important, and should allow doctors to better track superbugs' spread around hospitals, as well as assess the risk of post surgery infections.
The organisers of the meeting think that this research could make a big difference to hospital care in the UK, and public health officials and microbiologists present seemed excited at the prospect of running experiments like this in the UK.
It is early days for meta-genomics, and even Gilbert admits "the complex mess [of data] takes major computational power to put together". But advances mean that one day patients might have their microbiomes examined as - or even before - they enter the hospital, informing doctors as to the likelihood of catching or spreading a superbug infection, and hospital rooms of the future could be designed with microbiomes in mind, to further reduce the risk of complications...
- Previous Invasive Species
- Next Diagnosing Emerging Disorders










Comments
Add a comment