Scientists have found a way to alter the botulinum toxin (botox), which is often used to iron out skin wrinkles, so that it can be 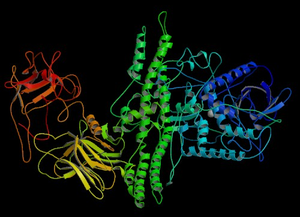 used to treat cystic fibrosis and other lung conditions.
used to treat cystic fibrosis and other lung conditions.
Writing in PNAS, Sheng Chen and Joseph Barbieri from Wisconsin medical college explain how they have discovered what makes botox so specific for nerve cells. The toxin enters motor nerve terminals at the point known as the nerve terminus where they link with muscles. Inside the nerve ending botox breaks up a protein called SNAP25, which is essential for nerve cells to release the nerve transmitter chemicals with which they communicate with target muscles.
In other non-neuronal cells, however, SNAP25 is replaced with a related molecule called SNAP23, which is subtlely different in its chemical make up. Botox can't break down SNAP23, which is why the toxin only targets motor nerve cells. But, by comparing the structures of SNAP25 and SNAP23 and botox itself then researchers were able to pinpoint which part of the SNAP23 molecule was making it resistant to botox breakdown.
Using this knowledge, and by genetically altering the structure of botox very slightly, the scientists were able to produce a form of botox that can attack SNAP23. This means that they can stop non-neuronal cells from releasing substances like mucus, which could be used to cut down the production of sticky mucus in the lungs of patients with cystic fibrosis. It could also be used to prevent immune cells from producing inflammatory hormones, helping to damp down damage in autoimmune diseases.










Comments
Add a comment