A recently-discovered antimicrobial can also combat chronic, deep-rooted infections previously regarded as resistant to treatment, US scientists have 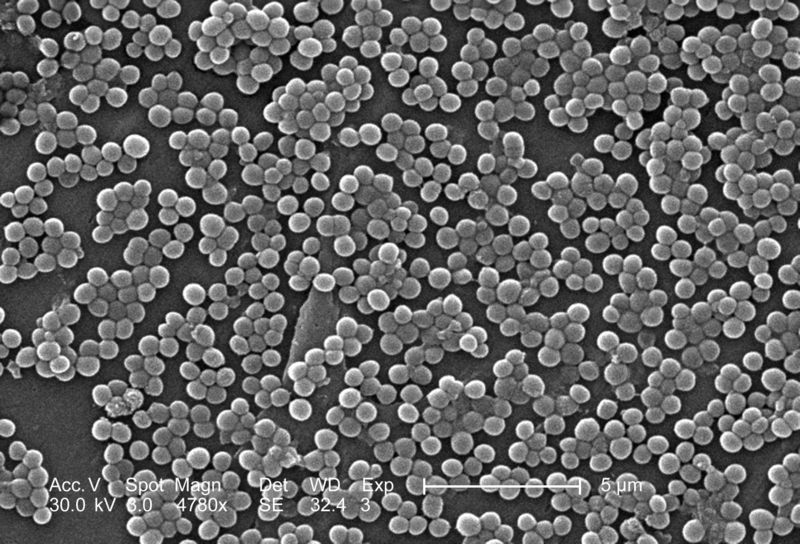 shown.
shown.
Dubbed ADEPs, the acyldepsipeptide antibiotics were first described in 2006. These molecules are made by a soil bacterium called Streptomyces hawaiiensis, which uses them to fend off attacks from other micro-organisms.
They work by activating a system inside bacterial cells called ClpP; this works as a mincing machine, grinding up and disposing of distorted or mis-folded proteins that could otherwise adversely affect the functioning of the bacterial cell.
Defective materials earmarked for destruction are threaded into the ClpP mincer through a small pore at its centre, which limits the size of the molecules that can be chewed up. But when the ADEP antibiotic is added, it crowbars-open the pore so that much larger proteins can fall in and be pulverised, including healthy proteins critical for the survival of the microbe.
Following treatment with the agent, bacteria effectively smash themselves to pieces from the inside and die. That much was known, but now Northeastern University, Boston scientist Kim Lewis and his colleagues have found that the ADEPs, including some synthetic derivatives that are now being made, may also be able to help in situations where other treatments have failed.
Specifically, writing in Nature, the US team have found that the agents are extremely effective against bacteria known as "persisters". This term describes a phenomenon - first noted 70 years ago - of microbes that crop up within a culture only at a rate of about 1 in a million bacterial cells but have the ability to grow only very slowly.
Effectively they exist in a state of suspended animation, remaining perfectly viable but with a very reduced metabolism, which places them beyond the reach of the majority of antibiotics because these tend to target chiefly fast-growing bacteria.
Consequently these persistent, resistant bugs are a major healthcare headache, causing recurrent tissue infections as well as colonisation of implants and catheters. Lewis and his team tested one ADEP - ADEP4 - against Staphylococcus aureus persister cells.
Coupled with an existing antibiotic, rifampicin, ADEP4 completely sterilised a culture of Staphylococcus aureus bacteria; it also eradicated bugs from within a biofilm, which is a drug- and immune-repelling protective structure formed by bacteria when they grow on certain surfaces, such as medical implants.
Mice with deep-rooted Staph tissue injuries, which are traditionally very hard to treat completely, were also cured. Control animals with similar infections treated using conventional antibiotic therapy all relapsed when drug administration ceased.
Tests on bacteria subjected to ADEP treatment showed that more than 200 key proteins had been dismantled within their cells, rendering them inviable.
Coupling a conventional antibiotic alongside the ADEP agent also prevented the bugs from becoming resistant by attacking any non-persistent "fast-growing" bacteria that would otherwise be capable of mutating to combat the action of the drug.
But it may not be just bacteria that can be targeted with this type of treatment. Concluding their paper, Kim Lewis and his colleagues speculate that, "this general principle of killing might be applied to other organisms as well as prove effective in developing therapeutics to treat fungal infections and cancer."










Comments
Add a comment