A mouse given a human immune system has enabled scientists to take the first steps in testing a new treatment for HIV, the immune-disabling agent that causes AIDS.
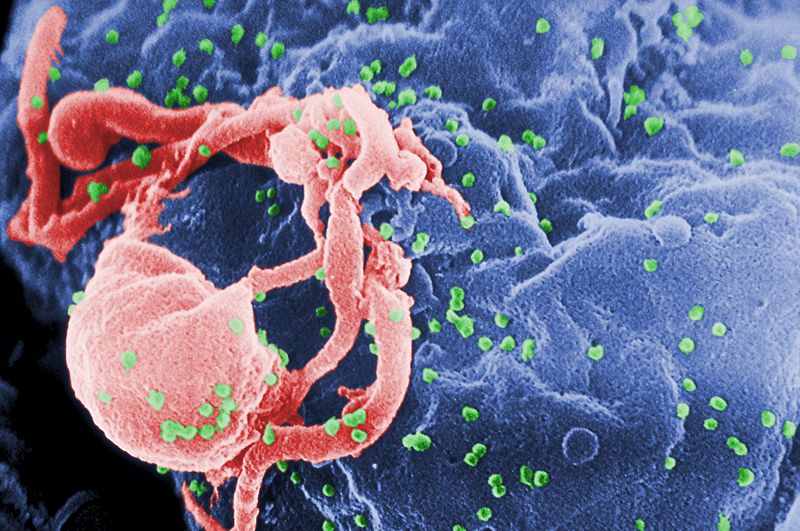
Currently, HIV-infected individuals are managed using a strategy called HAART - highly active anti-retroviral therapy - which involves the simultaneous combined use of several drugs that target different components of the virus lifecycle. And whilst this approach has been very successful, helping many patients to maintain good health, the drugs themselves often have significant side-effects making them hard to tolerate for some patients, and the gradual emergence of resistance still remains a problem. But recently scientists have found another way to disable the virus, using short pieces of genetic material.
One approach is to design short sequences of nucleic acid called siRNAs - small interfering RNAs - which are the genetic mirror image of certain essential viral or host genes. When these siRNAs enter infected cells they "cancel out" their target gene, preventing the virus from reproducing.
 Effective though it is, a significant problem is delivering sufficient quantities of these so-called functional RNAs into virally-infected cells in the first place.
Effective though it is, a significant problem is delivering sufficient quantities of these so-called functional RNAs into virally-infected cells in the first place.
Now Colorado State University scientist Charles Neff and his colleagues, writing in Science Translational Medicine, have solved the problem by using another short piece of genetic material, this one known as an aptamer. These are molecules of RNA selected on the basis of their ability to fold into a certain shape so they lock tightly onto a target structures.
The Colorado team have developed on of these aptamers to recognise an HIV protein called gp120, which the virus uses to infect susceptible immune cells. Alone, and when tested on cultured cells in a petri dish, this aptamer is very effective at neutralising HIV.
But the team have now gone a step further. By coupling their aptamer, which they call A-1, to an siRNA molecule that targets two key HIV genes, they've found they can simultaneously deliver the small interfering RNA selectively to infected cells and with very high efficiency, whilst also directly neutralising viral particles using the aptamer.
They tested this chimaeric molecule - called Ch A-1 - in mice that had been treated with human stem cells so that they make human white blood cells and can be infected with HIV. Compared with untreated control animals that maintained very high levels of circulating HIV and showed a 50% decline in CD4 white blood cells over an 18 week period, those receiving the new treatment rapidly developed an undetectable viral load in the bloodstream and maintained a normal CD4 count.
The team checked these animals for signs of viral mutations that might lead to resistance to the new agent, but did not detect any consistent or reproducible dominant mutations.
This suggests that this strategy could provide doctors with a potent new weapon with which to combat HIV, including HIV that has become resistant to existing therapies. The next step, say the researchers, will be to translate the treatment to a human clinical trial to assess its efficacy in real patients.










Comments
Add a comment