A new technique to block antibiotic resistance in bacteria has been discovered by scientists in Denmark.
With the drug development pipeline 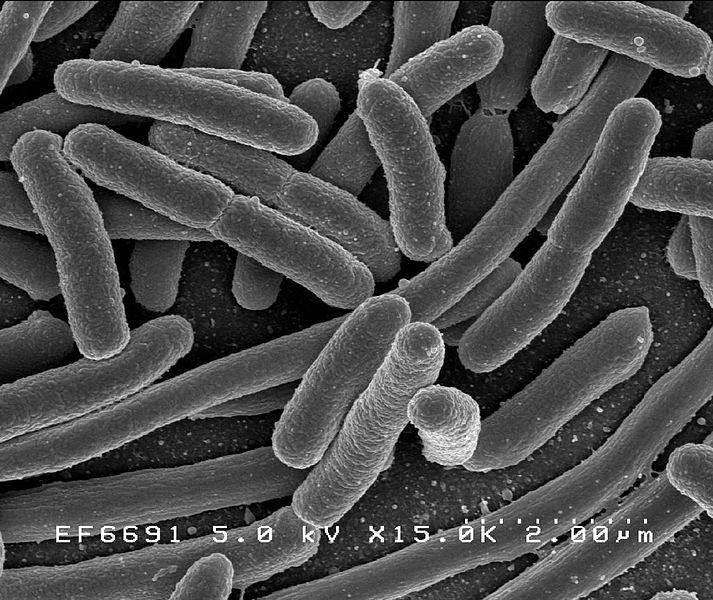 at an all-time low, there couldn't really be a worse time for rates of microbial resistance to be steadily rising.
at an all-time low, there couldn't really be a worse time for rates of microbial resistance to be steadily rising.
Policy makers in many countries, including the UK's Chief Medical Officer Dame Sally Davies are even warning that, within a matter of a decade or so, the antibiotic arsenal will be on its last legs.
So the announcement this week from Technical University of Denmark researchers Lejla Imamovic and Morten Sommer of the discovery of a new way to prevent resistance - but using only existing rather than any new drugs - might be just the shot in the arm that the sector needs.
Published in Science Translational Medicine, the Danish duo's approach depends upon a principle termed "collateral sensitivity".
Put simply, in order to become resistant to one class of antibiotic drugs - call it drug A, bacteria often have to drop their guard and become super-sensitised to another antibiotic - drug B. This can happen because the clusters of genes that are activated to defend against A can switch off the very genes needed to fortify the bacteria against B. And thus, the first bugs to die when exposed to drug B would actually be the very ones that were showing resistance to drug A.
So, Imamovic and Sommer reasoned, if the right antibiotics are administered in the right order, it should be possible to prevent the establishment drug-resistant bugs in the first place.
To test this theory, cultures of E. coli bacteria that were individually resistant to one of 23 different antibiotics were tested against the other 22 antibiotics to see which, if any, of the drugs they were more or less sensitive to.
Seventeen of the 23 drugs tested showed the theorised collateral sensitivity to a second antibiotic ranging from them being two- to eight-fold more vulnerable to the drug compared with non-resistant bugs.
Using this information, the researchers were able to draw up over 200 drug cycles - sequences of 2, 3 or 4 antibiotics - that if administered successively over a short period to bugs with resistance to a given drug should destroy those bugs and thus prevent further resistance developing.
Tested on two clinical strains of E. coli that were resistant to 8 of the 23 antibiotics studied, the drug cycles successfully destroyed all of the bugs as predicted.
According to the researchers, "This study provides proof of principle that an underappreciated side effect of resistance, collateral sensitivity, can be used to target drug resistance when selected drugs are cycled optimally."
They go on to speculate that collateral sensitivity cycles like those established by their study could be effective for treating a wide range of E. coli pathogens, which are now a leading cause of hospital-acquired multi-drug resistance infections...
- Previous New nose grown on forehead
- Next Mind Boggling Bog Bodies










Comments
Add a comment