Cancer vaccines: Empowering the immune system
Recently, doctors announced some extremely encouraging news about a jab for people with advanced forms of several types of malignancy, including melanoma, lung cancer and other solid organ tumours. The vaccine is called mRNA-4359 and has been developed by the pharmaceutical company Moderna, of Covid vaccine fame. The trials have been conducted here in the UK, and we’ll hear from the man running the study. Also, the success of the HPV vaccine in preventing cervical cancer, and how a Lynch syndrome vaccine could prevent a variety of malginancies...
In this episode
00:49 - Why the immune system holds the key to cancer treatment
Why the immune system holds the key to cancer treatment
Charlie Swanton, UCL
We’re going to examine how cancer develops; how it has traditionally been treated; and how these new cancer vaccines look set to become a revolutionary tool in the fight against this disease. Here’s Charlie Swanton. He’s Cancer Research UK's chief clinician, a principal group leader at the Francis Crick Institute, and a thoracic oncologist at University College London Hospital…
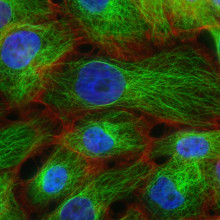
Charlie - Cancer refers to an uncontrolled proliferation of cells that ultimately derive from a single cell of clonal origin that, due to their uncontrolled proliferation, invade the tissues around them and ultimately invade and spread across the body.
Chris - What proportion of the population will have a run in with cancer? If I'm an average person, which I hope I am, what would be my lifetime risk of this happening to me?
Charlie - Cancer Research UK estimates that over a lifetime one's risk of cancer is somewhere between one in three and one in two.
Chris - Quite high, isn't it?
Charlie - It's high and it is a disease of ageing for the most part.
Chris - Why does it happen, though? Why is it that when I'm young you don't seem to see very many people who have a malignancy but, as we get older, it tends to occur more commonly?
Charlie - There are many theories. The first is that as we age we accumulate more mutations in our cells. But what has become apparent over the last five or six years is that actually our normal cells in our body, our normal tissues, are a patchwork of mutant clones. And actually, whilst mutations may be necessary for tumour initiation, they're not sufficient. And so other aspects are required, and that probably relates to chronic inflammation that's required to initiate the first tumour cell with mutations and possibly local tissue disorder, disruption of normal tissue architecture that can occur with ageing.
Chris - So it's a range of things that have got to go wrong, the odds of which increase as we get older. So it's almost like aligning all the holes in the Swiss cheese to get exactly an aligned hole that enables cancer to escape and become a problem.
Charlie - That's exactly right, Chris. Yes.
Chris - What sorts of other things are controlling cancers normally, then, that mean that a young person doesn't have a tumour?
Charlie - First of all, a young person has many fewer mutations than somebody like me in his mid fifties. Younger individuals just simply have fewer mutations in their normal cells. They're less exposed to the chronic inflammatory stimuli that I referred to. Their tissues are more ordered and more structured in a normal manner. But, in addition, the body's own immune system plays an important role in keeping malignant clones at bay. Indeed, it's been postulated that tumours are initiating much of the time in elderly individuals and are being controlled by the body's own immune system and being prevented from initiating and evolving.
Chris - That's fascinating. Many of us could have cancer at any one moment, but then the immune system stamps on it?
Charlie - The answer to that question is hard to prove. Where we have evidence for it, we can look at the archaeology of cancers that have evolved in patients and find very strong evidence for what's called immune editing. That is, a footprint, or a fossil record if you like, of prior immune activity against the tumour. That is, it has essentially annihilated malignant sub clones with what we call immunogenic potential. That is, the potential to alert themselves to the immune system. So we have evidence from looking at tumours that they have been predated upon, if you like, by a functioning immune system in the past.
Chris - Can I paraphrase that and say, basically, the body's trying to produce cancers from time to time because it develops changes in the DNA, mutations that make a tumour try to appear. The immune system responds and stamps it out, and you can see in the genetic record of the immune system, or in the tumour itself, the fact that has happened. But then, eventually, there's some kind of breakthrough that enables the tumour to occur. Is that because there's a loophole in our immune system and cancers are just basically probing our immunity until they find the chink in our armour?
Charlie - It's a very good question. The answer is that there are ways that the cancer cell evolves to evade alerting the immune system to its presence. That can occur from ways in which the tumour can mutate DNA: it can mutate specific genes that are required to be recognised by the immune system such that the cancer begins to evolve and develop below the radar, so to speak.
Chris - On the basis of what you've just told me, there is a precedent for expecting the immune system to be able to control cancer. We can see that it has done that in our own bodies in the past. Therefore, it's a question of when we have manifest malignancy. It's a question of making it work again, but this time work against that particular tumour. It's a bit like saying, we know fusion can work because the sun's doing it, but we've got to get it to work on Earth. We've got to get it to work in the body against a cancer that has broken through.
Charlie - Except that there is one caveat, which is we've already proven this works. There is very good evidence now that boosting the immune system by releasing the brakes on T cells can improve outcomes for many different tumour types, both in terms of progression-free survival, overall survival, and even cures in the context of, for instance, solid tumours like advanced melanoma.
Chris - Talk us through how this actually works, then. What is the approach to to trying to get the immune system to stop ignoring something that it had previously overlooked?
Charlie - The way in which this works is that there's a subgroup of cells in the immune system called T cells, and these T cells have evolved over billions of years of evolution to essentially recognise non-self. But what we discussed in the last few minutes is that tumours also develop mutations and can appear to the immune system as non-self, but the tumours also in their evolution adapt and suppress t-cell activation. What we've learned through some seminal work from Jim Allison and Honjo who won the Nobel Prize for medicine for this discovery, is that there are specific brakes on T cells that are activated by the cancer cells that one can intervene on and block. By doing so, you can release T cell activity to attract them to tumours and recognise tumours and essentially annihilate them.
Chris - And are you involved in any of them specifically?
Charlie - I'm very involved in lung cancer treatment with immunotherapy, either through vaccine developments, T cell therapies, or immunotherapies. So yes, very much so.
Chris - And the outcomes from these treatments, do they buy time or do we dare to use the 'c' word and say, well, we're actually looking at potentially curing people?
Charlie - Well, that's not a word I use terribly often in advanced lung cancer. That said, we do have a number of patients who have been on these drugs for a long time who are in long term remission. I haven't yet used the word cure openly but, privately, I'm thinking that for a small minority of patients treated with these drugs, probably. I'd say it's a small minority in which we're achieving long-term remissions and possibly cure. In melanoma, it's much higher. Upwards of 30, possibly 40% of patients with advanced melanoma can expect to be in long-term remission and even be cured with these drugs. We're in the very early chapters of this story, and I think over the next 50 years we're going to see continual improvements in outcomes as a result of immune therapies like vaccines, T cell adoptive therapies and checkpoints, inhibitor therapies.

09:21 - HPV vaccine eradicates cervical cancer
HPV vaccine eradicates cervical cancer
Margaret Stanley, University of Cambridge
There’s one other anti-cancer vaccine that’s been incredibly successful to the extent that it’s nearly wiped out a formerly common disease in a whole generation of young people. It’s the cervical cancer vaccine, which works not by targeting the cancer itself, but by preventing infection with the human papillomavirus - HPV - that causes the majority of cervical cancers to form. It’s one of the biggest success stories in vaccine and cancer medicine the world has seen. And almost twenty years ago to the day, before it was widely known about, one of the scientists who helped to make this vaccine a reality appeared on this programme to explain what would - in the years ahead - be rolled out and how it would work. Now emeritus professor of Pathology at Cambridge University Margaret Stanley is back with a recap on how this vaccine works, how effective it has turned out to be, and why the human papillomavirus causes cancer in the first place…
Margaret - It's because the virus makes different proteins and two of these proteins actually can control cells dividing and they can grow too much and they don't age. It sticks the cell in its early juvenile state and then there are accidents in the DNA and bits of the virus get incorporated into the cellular DNA. They then control what the cell does and that's the start.
Chris - Why are some of these viruses better at doing that and causing cancer than others? Because it's a big family of viruses, the papilloma viruses, and some are linked to this specifically. How is that achieved?
Margaret - You call the viruses a family. Like all families, they have white sheep and black sheep. The black sheep are those that encode proteins that have this capacity to deregulate the cell. Now these proteins are essential for the virus to make its virus DNA and, if they're made at the wrong time, that's when things happen in the cell. It's only a few of the black sheep viruses that have these proteins. It's specific to a group of viruses, even though it's a huge family.
Chris - And before the vaccines came along, what fraction of the population, if I picked a person at random from the population, would be carrying, or infected by, or have had a run in with some of these viruses capable of causing things like cervical cancer?
Margaret - Well actually 80% of us either will have had one of these viruses, are going to get one of these viruses, or have one at the time. But most of us get rid of them. We have great immune systems and the immune system gets rid of the virus. But some of us are unlucky. We're unlucky in our genes and when we get the virus we are unlucky in the age at which we get it. That's when you get a group of things that really increase your risk. It's not necessarily going to happen, but you've got a big risk of it happening.
Chris - And how has the vaccine made a difference to that process?
Margaret - It prevents the virus infecting because the virus has to stick to the outside of the target cell and get inside to start its business. Now, the vaccine causes antibodies and they bind to the surface of the virus and prevent it actually entering the cell. They prevent infection in what's called a sterilising immunity. And because you've prevented infection, you ain't got no virus there, so the sequence of events I've described doesn't happen.
Chris - If one looks at what has happened in the years since we introduced the vaccine in a number of countries, what difference has that made to cervical cancer rates?
Margaret - In the UK we vaccinate school kids, I think it's year seven, year eight. Before Covid we were getting 80 to 90% coverage. After Covid it dropped, but it's starting to come back and everybody's working hard. If you get that high coverage, then I can tell you the number of precancers caused by these viruses has virtually disappeared. In women under 30 invasive cervical cancer has virtually disappeared. It hasn't disappeared in the older women because they haven't been vaccinated, but the women under 30 have been vaccinated. If you've been vaccinated, you will not get the cancers caused by these viruses.
Chris - That's quite a turnaround, isn't it? I remember when I went to medical school, learning about cervical cancer, and more than a thousand women a year in the UK alone were losing their lives to cervical cancer. And you are saying now that if we follow the cohort of people who are about 30 and below, that number will effectively be zero?
Margaret - It will. In the UK we've actually controlled cervix cancer very well. Our screening program, despite all the things shouted about it, works well, but you have to come and participate in it for it to work. Before the vaccine, we had something like 3 to 4,000 cases of cervix cancer a year and about a thousand women died. Now, with the vaccine, we have something like 200 cases of cervix cancer and the mortality has fallen equivalently.
Chris - Really encouraging stuff. In terms of the virus itself, is there a risk that because we vaccinate against certain types of the virus, that some other rarer forms will become more prominent because they're not represented in the vaccine? Or does the vaccine end up suppressing those as well because it is a big family of viruses?
Margaret - I don't think so. This of course is something that the scientific community is taking note of and there are big, big studies all over the Nordic countries where you can follow people very easily. So far there's no evidence of what we call type replacement. The other thing is, these are DNA viruses and they're incredibly stable. In fact, they use our body's own DNA repair mechanisms to repair themselves. So these are viruses that do not mutate. So far it looks as though type replacement is not an issue to worry about.
Chris - Will the viruses disappear in the population, effectively, eventually?
Margaret - That's the idea providing we immunise enough people. The name of the game is vaccine coverage. You've got to be in it to win it. You've got to have your vaccine because then you are protected. If there's hardly any virus, you can't infect anybody: the virus has nowhere to go. It has to move to another person to make more viruses. If that other person is vaccinated, you can't infect them.

17:25 - Covid style mRNA cancer vaccines enter clinical trials
Covid style mRNA cancer vaccines enter clinical trials
Debashis Sarker, King’s College London
We’re going to examine messenger RNA - or mRNA - cancer vaccines. These can help the immune system detect and destroy cancer cells. They work by introducing short pieces of the genetic material mRNA into the body; this is picked up by immune cells, then translated to produce antigens similar to those displayed on cancers. This triggers an immune response against that target, and it’s also how the Covid-19 mRNA vaccines work. Debashis Sarker at King’s College London has been conducting clinical trials for patients with lung cancer, melanoma and other solid tumours and has been telling me how they work…
Debashis - mRNA, it's like an instruction manual or recipe. It tells your cells how to make a specific protein. For a cancer vaccine, the mRNA is the recipe for making a tiny part of that cancer cell, what we call the cancer antigen. When a doctor gives a cancer mRNA vaccine, it basically delivers that mRNA or that recipe into some of your cells, and those cells can read the recipe and make that specific cancer antigen. Once that is made, that is shown to your immune system, just like a wanted poster of the cancer cell. Now that your immune system has seen the abnormal antigen, it learns how to recognise it and your immune system can then go around your body looking for cells that have that same antigen, which are actually cancer cells, and use the immune system to better recognise those cancer cells to try and attack and destroy them.
Chris - How do you pick your target? When you've got a cancer in front of you in a patient, how do you say, well, that's the bit of the cancer I'm going to persuade the immune system to go after?
Debashis - The first is what we call a personalised vaccine where one of the things that we can do is what's called gene sequencing to try and understand what are the abnormal mutations that a cancer cell is producing, and then produce a specific personalised vaccine individual to that patient. That's one approach and certainly there are a number of these mRNA cancer vaccines which have that particular approach. There are other cancer vaccines, more what we call off the shelf vaccines, which look at common tumour antigens which occur across a whole range of different cancers, and using that RNA vaccine technology to target those specific antigens.
Chris - And do you crosscheck to make sure that they're unique to the cancer, these antigens, so you don't then provoke the immune system to go running after your own tissue and effectively cause autoimmune disease, which could otherwise happen?
Debashis - I think part of this is for these types of vaccines to train the immune system to recognise these antigens as the bad guy. One of the theoretical advantages of this type of technology is that it should be very specific for the cancer cells and not target your body's normal cells. The safety of these types of vaccines should be very good because, unlike things like chemotherapy, which are also attacking your body's normal cells, those should be relatively spared.
Chris - You've been running some trials against a range of different cancers, melanoma - a kind of skin cancer - lung cancers and things. You've just been presenting the results of those trials. What have you been showing?
Debashis - The trial that I'm currently involved with is a very early stage trial. It's what we call a phase one trial of a new mRNA based cancer vaccine. The principle behind it is to try and help the body's immune system target and attack cancer cells and it actually is designed to target two specific proteins or antigens, as we've been describing, which can sometimes help the tumour to escape the immune system. So in the trial that I've just presented recently, we've tested this vaccine in patients for the first time. Now, because it's a phase one clinical trial, the main aim of this particular trial is really to test how safe and tolerable the drug is and work out what dose of the vaccine we should be giving. In this particular study, what I reported is 19 patients with a whole range of different types of cancers who had often received multiple types of previous treatment including multiple lots of chemotherapies. This particular vaccine is given as an injection into the muscle every three weeks. What we looked at was how safe the vaccine was, how well tolerated it was, and also whether it was able really to generate that immune response that we wanted to see to be able to take the drug into further development. The findings that I presented were really to show that the vaccine was well tolerated with no serious side effects, which is what we would expect from an mRNA Covid type vaccine. We demonstrated that the drug can activate the immune system in many patients in the way that we would want. In some of the patients that we treated, we were able to show that, for a period of time, the cancer didn't continue to grow in the way that it had been prior to the study. Very preliminary results, but exciting. We are now testing this particular drug in more patients and in particular for patients with melanoma and lung cancers, really to try and see genuinely whether it's effective and can be potentially used as a treatment in the future.
Chris - Have you gone in and taken pieces of the tumours out in these patients to see if you are now seeing an intensification of the immune response which, if the vaccine is provoking the immune system to attack better, perhaps you'd expect to see?
Debashis - We have done that on a small number of patients and in fact that work is ongoing at the moment in other patients who are participating in the trial. What we have been able to see so far in some of those patients is that we've been able to elicit that immune response that we wanted to see in terms of activating those specific immune cells. And also, that impact on what we call the microenvironment: the ability to activate important immune cells against the cancer, but also to down regulate, or to reduce the activity of cells that sometimes suppress the immune system. I think those are important findings that show the validity of this approach. But hopefully with more information coming through from other patients treated on the trial, we'll be able to get more stronger and robust data.
24:20 - Lynch syndrome vaccine: Cancer treatment of the future?
Lynch syndrome vaccine: Cancer treatment of the future?
David Church, University of Oxford
We’re going to conclude today’s programme by examining the next generation of cancer vaccines. Scientists at the University of Oxford are hoping to develop a vaccine for people with a genetic disease called Lynch syndrome; affected patients have an increased risk of developing cancer in a number of different organs. The project is called Lynchvax, and it’s been funded by Cancer Research UK. Here’s David Church, an oncologist at the University of Oxford who leads the project…
David - Lynch syndrome is a genetic condition, and it's the commonest cause of genetic cancer, hereditary cancer, that's cancer that runs in families, in the UK and globally. It's caused by a faulty copy of a gene. These are a combination of genes that are responsible for ensuring that when our DNA is copied, before our cells divide, that copying is accurate. What happens is that we're born with two copies of each of these genes and people with Lynch syndrome are born with one faulty copy of those genes. That means that, during their lives, if they have a defect in the backup copy, their cells lose the ability to copy their DNA accurately. As a consequence of that, there are errors, and we call them mutations, and then collectively, cumulatively, over multiple cell divisions, those errors can affect genes which are critical for growth of cells or death of cells and that can cause cancer.
Chris - Does it affect any tissue in the body, then? If it's affecting all your cells, does that mean that everywhere could develop a cancer or are there hotspots in the body?
David - The latter. It is interesting that, even though this is a universal process, the tissues, the organs of the body that are affected, are particular ones. The biggest risk for cancer is the bowel. For women, cancers of the womb, and also other cancer types like the stomach, the piping that connects the kidneys to the bladder, and elsewhere.
Chris - Who gets this - age wise - and how would they know?
David - The increased cancer risk is from a young age. Young people with bowel cancer, we find they have Lynch syndrome. The critical thing with Lynch syndrome is that we only know about a small fraction of people that actually have the condition, so there's a large initiative to correct that.
Chris - You are trying to treat it in an innovative way. Can you just compare what we used to do for it with what you are doing now?
David - At the moment, people with Lynch syndrome are diagnosed typically because when we diagnose someone with a cancer we do some testing to see if there's the signature alteration that Lynch syndrome causes in the tumour, and then follow on testing to test the DNA that they were born with. That can tell us whether the person has Lynch syndrome or not. But of course that means that they've already been diagnosed with the cancer so they have all the standard cancer treatment: surgery to remove the cancer, possibly chemotherapy afterwards. In a proportion of cases that's all too high, by the time the cancer is diagnosed, it's already spread. What we need to do is to think about novel strategies to diagnose these people earlier, and also of course to prevent cancer in people with Lynch syndrome. But we are exploring an alternative approach, which is a vaccination.
Chris - I suppose the complexity here is, unlike someone who doesn't have Lynch syndrome and they do get a cancer (you treat that cancer, they can then regard themselves as in remission, let's say) if someone has Lynch syndrome, the same mechanism that caused them to have the cancer in one part of their body or one part of their bowel, it could put all of their bowel at risk so they're continually at risk. So having a way to keep the immune system on high alert has got to be the way forward?
David - Absolutely. What we're working towards is targeting the power of the immune system to recognise and, we hope in time, prevent cancer in people with Lynch syndrome. In so doing, our hope is that that would work in all the tissues of the body, not just the bowel, but also in the womb in women who have Lynch syndrome, and elsewhere.
Chris - Talk us through it then. How will this work? What do you actually do if you pick somebody up who's got it and you want to do this for them? What's involved?
David - We're analysing cancers and precancers in people with Lynch syndrome. Precancers are lumps, tumours, but they haven't actually had the alterations which mean that they're able to spread elsewhere in the body. There's a period before a precancer becomes an actual cancer and has the risk of spreading and all the consequences that entails, of course. Now, I've already mentioned that people with Lynch syndrome have an error in copying their DNA which means that the cells with this error accumulate errors or mutations. What this means is that those errors can cause abnormal proteins to be produced by the cells that carry this defect. Those abnormal proteins, we've known for some time, can be recognised by the immune system. It's similar to if we get an infection, the body recognises that the infection isn't part of our normal body and the immune system can target the abnormal proteins, the proteins that the infection causes. It's the same with cancer, and the abnormal proteins that cancer mates can be recognised by the immune system. We've known for some time because cancers in people with Lynch syndrome have a large number of DNA errors or mutations that can be recognised by the immune system, but the immune response is ineffective. It is unable to control the cancer in these people. What we are hoping to do is, by identifying these alterations in DNA and consequently in proteins, we can actually anticipate the development of cancer and, by vaccinating against them, turbocharge or prepare the immune system to recognise these abnormal proteins so they can intercept the precancer before it becomes a cancer. That's the ambition that we have.
Chris - Would it be different proteins or different constellations of proteins in each individual? In other words, this is almost personalised medicine in the respect that you go in and you've got to look and see which abnormal proteins this person's pre-cancer might be making and that's what you then turn into your vaccine. Or have you got a one size fits all strategy?
David - The latter. There is a lot of interest in personalised vaccines and there's a big initiative in the UK NHS to deliver personalised vaccines including for bowel cancer. However, what we are talking about and thinking about here is an off the shelf approach. What we know from the analysis that we and others have done is that cancers in Lynch syndrome have predictable alterations in their DNA and that really raises the possibility that we could develop a one size fits all vaccine.
Chris - Are you not worried, though, that in the same way that flu virologists know that when we vaccinate people around the world against flu, we basically force the flu virus to evolve in a different direction? It's a bit like herding sheep. If you start vaccinating people against particular predictable tumour types, is there not a danger that their disease might mutate to circumvent your vaccine and then you'll start to get new kinds of cancer that we miss with our vaccine initially?
David - It's a great question. We know that, in advanced cancer, that's the majority of cancers that we diagnose and treat, the cancers are able to do that. Like a virus, it adapts and is able to become resistant to that therapy. However, what we're hoping to do by going after multiple targets early in the disease process, before the cancer has had a chance to get that variability and that ability to evolve to become resistant, that we can intercept that and prevent that.










Comments
Add a comment