Drug Discovery: The Future of Pharma
This week; from Big Pharma to Little Pharma, we look at how new drugs are discovered. Plus, in the news - what powers the Northern Lights on Jupiter, why cuckoos have the last laugh, and 3 decades of a telescope that’s changed our view of the Universe.
In this episode

00:47 - Mice live longer on high fat diet
Mice live longer on high fat diet
with Jon Ramsey, University of California, Davis
For years we’ve been told - for the benefit of good health - to keep fat intake to a minimum. That makes the discovery, announced last week - that a diet where most of the calories come from fat makes mice live 13% longer and stay active and healthy further into old age - very surprising. Eating a high fat diet induces a state that’s called ketosis and somehow this alters metabolism into a life-prolonging state. So what should be on the menu? Chris Smith spoke to Jon Ramsey to find out more...
Jon - This is a diet that’s become increasingly popular. Breakfast, for example might be to have a couple of eggs, avocado on the side, milk with some heavy cream. Then for lunch it might be something like having a leafy green salad with some salmon on top and an oily dressing and perhaps some butter. There are a range of options that are out there that people are following to try to make this diet as palatable as possible.
Chris - What’s bizarre is that what you’ve just described sounds like, based on all of the literature that’s been put out, a heart attack waiting to happen - for want of a better phrase. Yet you’re saying, you feed this to mice with the intention of seeing if they’ll live longer?
Jon - That’s correct. There’s been a number of potential concerns with these types of diets as people have been using them and one of our goals was just to say we haven’t seen a lot of long term studies. We wanted to do a study that, frankly, we wouldn’t be able to do in humans and that was just to say if we could carefully control a diet started at middle age and continue it for the rest of life, what impact would it have on health and lifespan?
Chris - What did you actually do with these mice? Just tell me the structure of the experiment and what measurements you made and then what you found?
Jon - There were basically two groups of mice. One group was involved in lifespan portion and for those mice we didn’t do anything except feed the diet, weigh the animals weekly, and then just measure age at death and then, at death, we determined cause of death. In a separate group of animals at middle age, and then again at later life, we did a range of tests to look at basic functions, so measures of memory, muscle strength, muscle coordination, muscle endurance and formation.
Chris - And to be clear, you began these dietary interventions when these mice were already in what would the mouse equivalent of middle age, so that would be like a human 50 year old?
Jon - That’s correct. We purposely picked that age because that’s the time when many humans are thinking about changing their diet.
Chris - What happened to these mice then?
Jon - What we saw in the lifespan side is that there was an increase in lifespan and, in particular, in medium lifespan there was an increase of about 13%. In humans, a 13% increase in median lifespan would be about 7 to 10 years. As far as physiological function, I think that’s where we really saw the interesting and exciting changes. Memory was improved compared to control mice, measures of muscle strength and muscle endurance, and coordination were increased in the ketogenic diet compared to the control animals. The really striking thing was that in those older animals they were able to maintain function very similar to what we saw in middle aged animals.
Chris - So, in other words, you’ve got mice remaining at high quality function into older age, and they’re also going further into older age than animals that eat what we would regard as a normal diet?
Jon - That’s correct.
Chris - Do you know how or why? It’s extraordinary to see such a big difference in longevity.
Jon - Well, that’s the million dollar question right now - we don’t know why. We have some possible ideas and we looked at couple of possible mechanisms. But people have been studying ketogenic diets for nearly a hundred years and there’s still intense debate as to the possible mechanisms through which this diet works. I think this is an area where there just needs to be additional work in the future to try to better understand the cellular mechanisms that are driving some of these changes we see with the ketogenic diet.
Chris - Jon, you have to tell me before you go, do you eat this sort of diet off the back of what you discovered - what did you have for breakfast?
Jon - I have experimented a little bit with this diet, but I would have to say no, I have not been following it. Part of the reason that I haven’t yet is I haven’t yet answered the question that I really wanted to address, and that was to try to look at shifts in metabolism that occur with calorie restriction. With calorie restriction, the animals aren’t in continuous ketosis and so I think that’s the next step. I really would like to look at that and if I notice changes with that approach I think it would be possible to design a diet that would be much easier to follow.

06:07 - How Jupiter powers its aurora
How Jupiter powers its aurora
with Barry Mauk, Johns Hopkins University
The Northern Lights - also known as the Aurora Borealis, are a beautiful display of dancing lights in the night sky, but aurorae are not just Earthly phenomena. Similar light shows have been spotted on Saturn, Uranus, Neptune and Jupiter and the question is are these manifestations created in the same way as they are here on Earth? A new paper out in Nature has revealed what powers the Jupiter aurorae, thanks to some very high tech instruments aboard the Juno spacecraft. Barry Mauk, from Johns Hopkins University, is one of the lead investigators on the project and he spoke to Georgia Mills…
Barry - The Northern Lights are an image - a TV image if you will - of this processes that are going on in Earth’s space environment - it’s called a magnetosphere. Basically, the solar wind, the wind of ionised gases that come from the Sun blow over Earth’s magnetic field. It acts as a giant electrical generator that drive electric currents within Earth’s magnetosphere. Those electric currents, some of them flow along the magnetic fields towards the polar magnetosphere and they encounter resistances to that current flow. Whenever a current encounters a resistance, you build up an electrical potential, and it’s that electrical potential that then accelerates electrons down onto Earth’s atmosphere that generates these dramatic lights.
We see this phenomena at Earth, Jupiter, Saturn, Uranus, and Neptune so far. I’ve described to you one process that generates aurorae on Earth, there are several other processes that can also generate aurorae on Earth. For these other planets, we don’t quite know which of the processes are involved in generating the aurorae. We can guess that they’re generated by similar processes, but we do not know for sure.
Georgia - You were interested in the aurorae on Jupiter. What did you want to find out and how did you go about investigating?
Barry - The Juno mission has multiple science goals. One of the major science goals is to understand Jupiter’s polar space environment, and particularly to understand Jupiter’s aurorae. So we went to Jupiter and we built instruments; there are maybe five instruments on Juno that are directed towards understanding Jupiter’s aurorae.
The instrument that I’m the lead investigator for is the Jupiter Energetic Particle Detector Instrument, which we call JEDI for short, and it is the one that was able to see this specific phenomena that we report in our recent paper.
Georgia - JEDI, so it was detecting the force I suppose?
Barry - Something like that, yes.
Georgia - What did JEDI find then? How was Jupiter’s aurorae created, is it the same way as on Earth?
Barry - We see some similar features. What we are reporting in this recent paper is the observations; we saw what we call these inverted V structures. What these inverted V’s indicate when we fly over an auroral form is that there are large electrical potentials that are along the magnetic field lines that are accelerating electrons down onto Jupiter’s atmosphere and are helping to create the aurorae.
Georgia - So you found these incredibly high electric potentials. Much higher than Earth, but it is a similar process?
Barry - At Earth the potentials are much lower; they are typically several thousand volts. The other major difference between Earth and Jupiter is that the power source is different. We talked about the solar wind blows over the magnetic field of Earth and acts as an electrical generator - that’s the power source. At Jupiter, the power source is Jupiter’s rotation. The rotation of Jupiter within it’s own large magnetic field acts as an electrical generator, and it is that process that generates the electrical currents.
Georgia - Why have you done this? Why is it important to know about the aurorae on Jupiter?
Barry - Our research is curiosity driven. We are trying to understand what processes operate in the universe and so it is curiosity driven. There are practical implications. One of things that we are finding is that the auroral processes are energising electrons to immense energies, to much higher energies that we see at Earth. These high energy electrons have energies comparable to the energies of Jupiter’s radiation belt. So, on that basis, we’re trying to understand how Jupiter’s radiation belt is created so that we can better engineer future missions to Jupiter, because high radiation is such an engineering technical challenge to missions that go to Jupiter.

11:07 - Chuckling cuckoos have the last laugh
Chuckling cuckoos have the last laugh
with Jenny York, University of Cambridge
When it comes to deception, cuckoos are the masterminds of the avian world. But, researchers at The University of Cambridge have discovered that these birds may be even cheekier than we previously thought. Stevie Bain caught up with Jenny York at her Madingley Wood field site to find out how cuckoos have the last laugh over their favourite host species, the reed warbler…
Jenny - Cuckoos are probably the most famous example of a brood parasite. They lay their eggs in the nests of other species, so they don’t rear their own offspring, they foist this parental care onto other species. They are incredibly secretive and rapid, so they hide away in a perch up in a tree observing the hosts building their nests. And they wait for this perfect moment to glide down and can, within ten seconds, lay an egg and leave the nest which is just incredibly fast. It’s really important that they do it quickly because they want to avoid the hosts noticing them.
But, after laying their egg in the nest, they give this bizarre chuckling call that’s very conspicuous. It seems, at first glance, a bit of a bizarre thing to do because you’ve gone to all this effort to be secretive and get in and out as quickly as you can so why announce it to everybody as soon as you’ve done your job?
We notice that the female cuckoo’s call is similar to a sparrow hawk call; they’ve both got this sort of high pitch, rapidly repeated, call formation. We wondered whether maybe this acoustic resemblance is useful and beneficial for the female cuckoo because it might distract the host’s attention as they’re returning to the nest. So instead of worrying about the contents of their nest, their defences are misdirected to concerns about their own safety.
Stevie - I’m guessing then you went on a mission to find out what this call was all about?
Jenny - We tried to investigate the reed warbler vigilance, so how worried they are in response to hearing four different call types: the female cuckoos call, the sparrow hawk call, and the male cuckoos call, and the collared dove as a harmless control. We found that reed warblers were much more likely to become vigilant when they heard a female cuckoo call or a sparrow hawk call. This shows that it worries them to hear both of these calls.
So we did an experiment out here up at Madingley in the botanical gardens to investigate whether using the same four calls on great tits and blue tits, which are not hosts of cuckoos in the UK, whether they respond the same way to female cuckoos and sparrow hawks. We found that the great tits and blue tits responded in a similar way to female cuckoo calls and the hawk calls, so that really suggests that there’s something about the call itself that is similar to a sparrow hawk call that triggers vigilance and wariness in small birds.
Stevie - I find that really interesting to think that these animals are so sneaky as to develop these traits.
Jenny - It’s all very well showing that there are similarities between the calls and that host species respond to these with vigilance, but what we wanted to know is whether the cuckoo is better off having created this diversion in terms of successfully parasitising the hosts. So, what we did was we found lots of reed warbler nests and we painted one of their eggs at random to simulate a cuckoo parasitising their clutch.
We found that they were much more likely to accept a cuckoo egg if they’d heard a female cuckoo call or a sparrow hawk call. And this is amazing because this means that by giving this call as she leaves the scene of the crime, she can divert their attention enough that they are paying attention to themselves and their own safety rather than inspecting the contents of their nest, and this distraction might mean that the hosts are more likely to end up rearing her offspring than rearing their own.

15:59 - James Clerk Maxwell Telescope: 30 years later
James Clerk Maxwell Telescope: 30 years later
with Wayne Holland, UK Astronomy Technology Centre
Now what do you remember about the 1980s? Brick-sized mobile phones? The ability of the world to function without facebook? Apart from those more trivial things, the 1980s also marked the birth of one of a telescope that has helped to us to see our place in the Universe much more clearly. The James Clerk Maxwell Telescope is now celebrating 30 years of gazing skywards, and, beginning in the 1980s, Izzie Clarke’s been hearing what it’s helped scientists to see...
Izzie - In 1987, the Bangles had us Walking Like an Egyptian, we were Living on a Prayer with Bon Jovi, and Star Trek: Next Generation set out on their own mission to boldly go where no-one has gone before… and they weren’t the only ones...
Wayne - This is one of the very first telescopes that was ever built for this particular wavelength. The technology was difficult, and we were borrowing ideas from the optical and the radio, and almost like pushing them together to try and make the technology work.
Izzie - That’s Wayne Holland. He’s a Professor and astronomer for the UK Astronomy Technology Centre in Edinburgh. And this year, scientists are celebrating 30 years of the James Clerk Maxwell Telescope.
Wayne - It doesn’t look like a conventional telescope. It’s almost like sitting in a large hut on top of a mountaintop on the big island of Hawaii. The instruments that we had on the back of the telescope were very simplistic. We would painstakingly move this one pixel from point to point on the sky and then we would try and basically build up an image. It was almost like joining up the dots almost of the actual signals that we were seeing. It would take an incredibly long amount of time just to build up a very small image of a fairly compact source like a nearby star or something like that.
Izzie - The James Clerk Maxwell Telescope, known as JCMT for short, became the world’s most successful single dish telescope working at submillimetre wavelengths. This is a region that’s roughly between the infrared and the radio part of the electromagnetic spectrum.
Wayne - It allows us to basically study light that’s emitted from very cold regions of space. Regions, for example, where galaxies, stars and planets may be forming.
Izzie - Stars form in these dense clouds of dust and gas, and this was one of the key investigations for JCMT in the 80s and 90s. This project called UKT 14 set out to explore these star formations, mapping the sky one pixel at a time.
Wayne - We found a what became known as protostars. It’s a term that was coined in the late 70s, but protostars were never really observed until the late 1980s, early 1990s, and they just look like blobs on the sky. You can work out their characteristic temperature and, in some cases, some of the constituent chemical elements they’re made of so you can produce a spectrum.
As time went on we learnt more and more about these objects. What were able to do is to place them in an evolutionary sequence, so some of the very earliest star forming regions were called starless cores, and then they became protostars, and then more evolved stars and then, eventually, stars like our own Sun are called main sequence stars. These early observations made a real inroad into understanding the whole star formation process.
Izzie - But, after a while, it was time for upgrade and, in 1997 came SCUBA, the world’s first submillimetre camera. And whilst this camera created images with just 100 pixels, SCUBA brought about the submillimetre revolution in astronomy…
Wayne - It was necessary to really push the sensitivity limits beyond our own galaxy. The Hubble Space Telescope had been launched and it produced a wonderful picture called the Hubble Deep Field of some very early galaxies. So what we did, we pointed out telescope with a SCUBA camera on the back at this particular point of sky and what we found was another population of galaxies, so the galaxies that we were seeing didn’t coincide with the ones that Hubble was seeing.
What SCUBA and JMT discovered was a completely new population of distant luminous galaxies that were completely invisible to the optical telescopes. The stars in these galaxies are, again, are enshrouded in cold gas and dust, but they shine brightly, again, at longer wavelengths as a result of heating this material up. What we believed we were seeing at the time has gone on to be proved correct. We’re seeing these galaxies something like 10 billion years ago and so looking at these very early galaxies, again, tells us a great deal about galaxy evolution and how these galaxies evolved to be the galaxies that we can see today. The giant electrical galaxies that Hubble and other optical telescopes see.
Izzie - This was one of JCMT’s biggest discoveries, and these young active galaxies are now known as SCUBA galaxies. Although SCUBA has made so many pioneering findings, it was obvious that by the turn of the century an even-more-sensitive camera was required, something that could look at wider parts of the sky - SCUBA 2...
Wayne - Since the commissioning of SCUBA 2, which was about 6 or 7 years ago now, this new wide field camera, it’s mainly been carrying out surveys, so large areas of sky. The first generation surveys that ran from 2012 till 2015 were surveying galaxy clusters, star formation regions. Also, a survey that I was involved in was looking at discs around nearby stars and looking for evidence of whether solar systems similar to our own are actually present around nearby stars. The range of astronomy that we can do with this telescope is immense.
Izzie - Potentially, do you think you could see the beginning of another solar system similar to our own forming?
Wayne - There’s been lots of work recently over the last decade on extrasolar planets. But what I’m interested in is actually seeing if the architecture of our own solar system: the 8 planets, the comets, asteroids, and that kind of thing, whether that kind of architecture can exist around other stars other than our own sun, and answer the question just how typical is our solar system around other stars.
You can do that by looking at evidence of discs and belts, and we’ve detected and imaged a number of these around nearby stars, some quite famous stars like Vega for example. And that gives you an idea as to what kind of environments there are around these stars. You can’t see the planets directly by any means, but you can infer their presence by looking at structures within the discs that we see as well. So it’s quite an exciting area of astronomy that’s been developing over the last few years.

24:22 - A potted guide to medicines
A potted guide to medicines
with Richard Gant, Institute of Continuing Education
From aspirin through to antimalarials, as many as half of the drugs in a modern-day doctor’s bag owe their origins to plants. To find out how, Georgia Mills took a turn around the gardens at Madingley Hall, with the head gardener Richard Gant, for a potted guide to drugs...
Richard - We call this the medicinal border which we’ve divided up in a contemporary way into different sections. So we’ve got culinary with various culinary plants that the chefs use, and then we’ve herbal medicine here in front of where we’re standing, and then we go into dye plants, and finally, we then move into aromatherapy/perfumery plants.
Georgia - I can see a lot of bright colours over there in the dye section. But looking here at the herbal medicines section, so these are all plants which have some contribution to human medicine in the past or currently. Could you give me some examples?
Richard - If we start with this Chinese or Southern Wormwood. I’ll give you a chance to smell… So what do you reckon that smells like?
Georgia - Oh, it’s quite potent. It’s a bit like lemon sherbet or something.
Richard - It’s quite repellent like, isn’t it? This is Artemisia annua; it’s from China. The Chinese have used it for centuries for treating fevers and high temperatures.
Georgia - And it’s still useful today. A compound from the unassuming green plant is an important ally in our fight against malaria…
Richard - It’s not really particularly pretty.
Georgia - It doesn’t smell great.
Richard - And it doesn’t smell great. But, by gum, does it have a use.
Georgia - There are lots of quite exotic looking plants here that I don’t recognise, but I recognise that one. That’s the tomato, so what does the tomato cure?
Richard - We’ve got the tomato here because increasingly it’s being recognised that tomato contains the active ingredient lycopene. And cooked tomato, where the lycopene is released, they’re finding it’s a particularly good, strong antioxidant, particularly for the treatment of prostate cancer and so forth.
Georgia - Right. How long have plants been used in medicine?
Richard - Every since really man came on this Earth, plants have been used for medicinal purposes. Obviously, a science has developed; increasingly we’ve been able to understand it more. I think there was an awful lot of trial and error, and I would imagine there were some poor people who probably succumbed through the trial and error.
But Cambridge has a very strong record because William Turner, who published the first herbal, was a fellow of Pembroke around about the time Madingley Hall was built, so we’re talking about the mid sixteenth century. Then a little bit later Culpepper the famous apothecary was at Cambridge. His father was the Queen’s man, although his son eloped before he graduated. But, of course, he went on to have a practice in East London.
Georgia - So from ye olde apothecaries to today’s chemist, we have plants and their diverse chemistries to thank for so many of our modern medicines…
Richard - We just don’t know what’s out there and one of the things is, as deforestation takes place, we don’t know what we’re losing. It might be the ultimate cure to the biggest disease that man has ever known.

27:53 - Big Pharma: How drugs get made
Big Pharma: How drugs get made
with Mene Pangalos, AstraZeneca
Drugs are mainly mass produced by pharmaceutical companies based on very detailed knowledge of the mechanisms of diseases and how our bodies work. AstraZeneca, one of the world’s largest pharmaceutical companies has just moved to Cambridge. So Chris Smith took the opportunity to ask Mene Pangalos, Executive Vice-President of AstraZeneca’s Innovative Medicines and Early Development Biotech Unit, about how a company like his invents and markets medicines in the modern era...
Mene - Turning science into medicine is probably the hardest journey we go on in our careers, and what actually gets us out of bed every morning. If we take a disease like heart failure where we’re trying to regenerate the heart, or reduce the damage in the heart after a heart attack, we'll take a cell from the heart and we’ll try and understand how that cell works, how it survives, and how we can try and affect its survival in a positive way.
We may find a receptor on the surface of that cell. I would think about it like a lock that we can open with a key, the key being the drug. If we can find a molecule that’s able to turn that lock open so the receptor gets switch on and, as a consequence of switching it on, we’re able to keep that cell alive, that’s how you start to think about generating a therapy that can regenerate the heart.
Chris - So what do you do then? You think we know what that receptor looks like, so then you go to your chemist and say I want you to design me just umpteem molecules that might engage with that lock, and then we’ll try them - what’s the process?
Mene - It’s long and arduous and, of course, we’re simplifying it to the ‘nth’ degree but that’s exactly right. You say I understand the shape of that lock, find me some keys that fit it, but when you find those keys please make sure they don’t fit any other locks that are on the cell, which are the other receptors that you don’t want to hit. Because, if you hit them you have side effects, you have toxicities, so this is why the process is complicated and difficult.
Then if you add the complexity on top of that of - and by the way, the key has to be able to penetrate the stomach and not be dissolved by all the acid in the stomach. It has to get just to the heart and not to the liver and the kidneys. It’s got to be available for 24 hours during the day so that you only have to take it once a day. That adds the complexity to what our magical chemists have to do in terms of designing those molecules that unpick that particular lock, and only that particular lock, but also do it in a way that doesn’t cause you lots of side effects when you take it.
Chris - At what stage do you actually start putting it into a living thing, whether that’s an animal or a person?
Mene - It takes quite a long time because the keys or the molecules have be stable, they have to be selective, and so that can take years before you get it into an animal. Then optimising that key to make it suitable for going into people, that can take probably another two to three years. Then you have to do all the toxicology experiments, which will take you another year or so. So you can see how very, very quickly you get to a journey that’s somewhere between five and ten years.
Chris - What fraction actually make it?
Mene - Less than 5%. So from when you’ve created the key to the lock and it’s ready to go into people, less than 5% if those keys ever become medicines.
Chris - So there must be a big price tag if we’re talking ten years plus of investment to get to that state, the amount you must spend for that 5% success rate must be humongous?
Mene - Our industry invests billions. AstraZeneca invests over 6 billion dollars a year just on research and development. So it’s a huge, huge investment and, of course, the risks are incredibly high, so when we do get a drug that’s successful we get very, very excited.
Chris - How long do you have in order to recoup what you’ve had to spend and then have enough of a war chest, effectively, to invest in the next arsenal of chemicals that are going to become the next blockbusters - we hope?
Mene - From the time we identify that key, we generally file a patent. And given how long it takes us to move that molecule into clinical trials, and then develop it through the clinical trials and ultimately get it approved as a medicine. I would say, on average we’re probably in the region of around ten years of patent exclusivity when you have that molecule, that key to yourself and no-one else can copy it. But once the patent expires, ten years down the road for example, then anyone else can make that key. And, of course, once that happens you get what’s called generic erosion and the price for the molecule goes down very, very steeply, and it become pretty much free for the rest of eternity.
Chris - It’s the 5th September today, and in Brussels this European initiative called DRIVE-AB is having it’s final meeting. DRIVE-AB is this initiative which is designed to drive reinvestment in research and development and responsible use of antibiotics because antibiotic resistance is a massive problem. But to cite DRIVE-AB’s statistics, they say there are just four pharmaceutical companies that have maintained investment in the development of new antibiotics. Why has the industry shifted away from what is clearly a massive demand area?
Mene - For us, it’s was an area we can’t spread ourselves too thin, so one of the areas where we think we can compete globally and do very, very well. I think one of the dangers that we have in our industry is that you could try and do everything and then you don’t do anything particularly well. So, for us, it was a decision that in oncology, cardiovascular, respiratory disease, we can compete globally.And the antimicrobial space, it’s a very, very challenging area. If you think about how antibiotics are used today in the terms of the fact that new antibiotics tend to be reserved as a last resort which means that, therefore, your medicines are not adopted early and, therefore it become difficult to justify any returns on your investment. But, ultimately, companies have to make the choice of where they think they can compete and actually be successful.
34:22 - The antibiotics argument
The antibiotics argument
with Professor Dame Sally Davies, Chief Medical Officer
There is a key issue in drug discovery. New antibiotics. Or rather, the lack of new antibiotics. England’s Chief Medical Officer, Professor Dame Sally Davies spoke to Chris Smith about the issue.
Sally - We’ve had no new classes of antibiotics since the late 80s. It’s difficult work, the low hanging fruit has been found, and people have disinvested because, as a world, we thought we’d cracked infection. We’re in this situation because we let across the world infection prevention and control, things like washing hands slip all too often. We don’t look after our antibiotics in the health system as effectively a we should, which is called stewardship.
And then, of course, we have to remember the rest of the system, and more than 70% of antibiotics across the world are used in agriculture and the food chain. So it’s not surprising that drug resistant infections can occur in the food chain and then be transmitted to humans.
Chris - You’ve said, rather shockingly, that we haven’t invented anything new in this space since the 1980s - whyever not?
Sally - I would argue that people thought we’d cracked infection. We had vaccines, we had infection prevention control and antibiotics. I think HIV should have woken us up to the fact that we hadn’t. And you know, it’s difficult science, even when you think you've got a candidate antibiotic, you’ve then got to take it into humans and the failure rate of antibiotics is much higher in that development period. It’s said to be one in five compared with a failure rate of one in three for other drugs, and it’s a very slow process
Find a new antibiotic - it takes a minimum of 15 and generally 20 years to get it into practice and we haven’t funded it effectively. There’s a market failure. The companies that invest in this don’t make any money. They all argue that they’re doing it at a loss if they’re still in the business. Even in academia, we’ve disinvested in having a critical mass of experts who can really drive this forward.
Chris - So, given that problem, how big is the threat facing the world because of the dwindling supply of antibiotics that still work?
Sally - We already know that the young, the old, the pregnant, the immunocompromised - think people on cancer treatments - are prone to getting infections. I can imagine the day where the cancer doctor says well Sally, I could give you something which would probably cure your cancer, but you’re sure to get an infection and I’m not sure we’ll be able to treat it. And yet, we pay billions for new cancer drugs and we haven’t invested in new anti-infection treatments.
Chris - Many of the people who are in the position to invent these drugs are arguing it’s just not financially viable for them to do so. What do you think governments could do to try and help them because this is, obviously, not going to be a problem where you just wield a big stick and say to pharmaceutical companies go an make us some more antibiotics because they’re not going to do that?
Sally - I think Europe has really led the way with the IMI programme DRIVE-AB. They’ve done some very nice work about what needs doing and how and that’s a private/public partnership, and we need to go on with private/public partnerships. Clearly, if you look at the work of Lord O’Neal and his special review for our Prime Minister, you can see that there are arguments from many people. I think DRIVE-AB support this that you need to de-link doing the research and making a profit. No-one wants drug companies to make a loss, but do they need to make a massive profit? And if we can find a way of reimbursing for the R & D then maybe we don’t have to use the drugs, we can keep them for when they’re truly needed. All of this needs working out further; it needs pilots and experimentation. I think people are beginning to move, but we’ve got to keep the pressure up and that’s the value of this UN inter-agency coordination group.
Chris - Do we have time or are we running out of time?
Sally - Well, with at least 25,000 dying each year in Europe, and a similar number or more in the States, for them we’ve run out of time and that goes on year after year. But, there is no shirking it that if we do it now, then we can make a difference.

39:16 - Little Pharma: Off the beaten track
Little Pharma: Off the beaten track
with Heather Fairhead, Phico Therapeutics
There are hundreds of small, and medium-sized enterprises exploring drug and antibiotic discovery. Chris Smith spoke to Heather Fairhead is a Founder and the CEO of Cambridge startup Phico Therapeutics, about the drugs they are trying to develop.
Heather - We’re trying to develop a new approach to antibiotics, and particularly focussed on infections which are serious and occur in hospital patients, so we have a two pronged approach to this. The first component of our technology are bacterial viruses, so in the way that humans get viral infections, colds or flu, bacteria have their own viruses that can attack them. What viruses are designed to do is to latch onto their target cell, so in the nose it would be a nose cell for example. They inject their DNA and their function really is to make more copies of themselves and burst out of that cell and infect other cells and just escalate an infection.
We take these bacterial viruses and we strip out the genes in there that we don’t want, and we insert a gene which encodes our antibacterial protein. The beauty of our protein is that it’s a naturally occurring protein, so it’s evolved over millions of years to do what it does. It actually targets the DNA inside the bacteria and it changes the conformation or the shape of the DNA and it completely inactivates it.
Chris - This is in the bacteria you target, so it’s almost like you’re doing gene therapy on a bacterium?
Heather - Inside the bacteria themselves.
Chris - So you’re using a virus to deliver a genetic message that then distorts the DNA of the bacterial cell?
Heather - It’s a sort of anti-gene therapy if you like because gene therapy, of course, is used for good purposes, but they’re actually killing the bacteria. Or I should say really, the bacteria are actually killing themselves because they are making this protein which disables their DNA but they’re programmed to do that. The beauty of this really is that it doesn’t matter even if the bacterium mutate, which is how most antibiotic resistance arises, our protein will stick to and inactivate that DNA. So, for the antibacterial components, it’s very difficult to see how resistance would arise although, of course, in nature you can never say never.
Chris - When you say these are serious infections, what class of infection are you going for - what bugs is this targeting?
Heather - Our lead product is targeting a bacterium called pseudomonas aeruginosa, and that is really a problem in patients in hospitals. It can commonly cause hospital acquired pneumonia. But it’s really a major problem in patients on ventilators, so in ICU, and that can be a whole range of people, not just people that have gone into hospital because they’re already sick. But it could be young people who have had an accident or whatever and they end up on a ventilator and these infections are really difficult to treat, and pseudomonas is a really tough bug. It has a quite a high mortality rate so that’s our lead focus.
Chris - How would this be administered? Would it be squirted into someone’s lung or onto the skin infection, whatever the target is where the bug is growing, or would it be given via the bloodstream?
Heather - We can deliver this drug in a whole range of ways. We’ve developed a topical antibiotic for decolonising MRSA in the nose. That’s on hold at the moment while we focus on this higher clinical need area of pseudomonas aeruginosa. We are developing an IV drug, but initially we’re going for, as you say, direct delivery into the lung. This would be inhaled because people on ventilators obviously already have delivery into the lungs. We find that we can dose a lot lower amounts if we’re delivering directly into the lung and, of course, that plays into how much the drug eventually costs.
Chris - When you say that it’s very difficult for you to get resistance to this drug, because antibiotic resistance is a major, major problem. At the same time the bugs could, nonetheless, mutate so that the phage, the virus you’re delivering the chemical with can’t bind to them any more, couldn’t they?
Heather - Absolutely they can, and no technology is perfect. The fact is that, if you like, in our technology, which is called SASPject, the phage could be seen as the weak part of the technology. However, people understand bacteriophages; they’ve worked on them for many, many years. So we understand all of the weaknesses of the phage going into developing our product which means that we can actually influence its behaviour before we go forward into the clinic. That means that we suffer less losses later on because we can address those upfront during the development process.
Chris - Considering the business side of this, what’s your game plan? Is the idea that you will get this to a stage when a very big company that has the capacity to do the really big trials you need to do, and do the marketing that you need to do, and take the drug to market that you need to do will do that, or is the intention that you will get it all the way to market yourself?
Heather - No, we won’t take drugs to market. That’s incredibly expensive and very time consuming as your earlier guest said. We will take the drugs through the early clinical stages and then expect to licence that product to a bigger pharmaceutical company.
Chris - How far away are we?
Heather - From having a drug on the market? Several years.
Chris - Okay, but that still sounds optimistic. So you’ve got something that’s working?
Heather - Absolutely, and that’s the point, isn’t it? That we know the bacterial viruses can target bacterials so we don’t have the risk there later on that it won’t work. We know that our protein is designed to disable DNA so we know that works, and we’re just bringing together those two components. And, hopefully, in the end will have a drug that saves lives and that’s what keeps us all focused really.
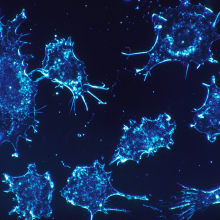
45:19 - 'Game changer' cancer therapy approved
'Game changer' cancer therapy approved
with Madga Papadaki, Institute of British Pharmaceuticals Industry
When you think of drugs you probably imagine pills in a packet. But last week there was a landmark ruling - the FDA (American Food and Drug Administration) approved a new type of treatment for one form of blood cancer. And it could be a game changer. To tell us about it, Chris Smith was joined by Magda Papadaki of the Association of the British Pharmaceutical Industry.
Magda - We had the most exciting piece of news in the war against cancer we’ve had for quite some time. The FDA approved Kymriah for the treatment of pediatric (that’s children) and young adult patients below 25 years of age in a rare and very aggressive form of beta cell lymphoblastic leukemia (B-cell ALL), which is a very aggressive and rare form of cancer. The treatment would be given to children that are either refractory or relapsed, which means that they’ve stopped responding to any other treatment or that their cancer has returned after everything else has been tried.
Chris - This sort of tumour, ALL, is the most common pediatric cancer isn’t it? About 25% of children who get cancer have this. At the moment, we can treat that and about 80% of people get better, don’t they, but for the 20% who don’t, it’s a pretty grim prognosis. But now we’ve got this drug, how does it work?
Magda - The immune system is the first line of defence our system has against viruses and against diseases like cancer, and the t-cells are it’s primary soldiers. The goal is to target and kill infected or abnormal cells and what cancers try to do is stop or make these soldiers less effective, which is what inspired the scientists to pursue this new line of treatment.
The scientific description of Kymriah is a long chain of buzz words. It’s autologous gene modified t-cell therapy. What this means: autologous means that every dose of Kymriah is a bespoke patient-tailored therapy that uses its own cells, its own immune system to seek and destroy cancer cells.
Chris - So you’re saying you take the patient’s own white blood cells, their own t-cells out of them?
Magada - Exactly. The story starts like that. In the hospital where a safe amount of blood is taken from the patient, and the white blood cells that include t-cells and other types of cells are taken out. These are moved to another research and manufacturing facility where they undergo gene therapy using viruses that have been rendered safe - that means they can’t lead to any further disease.
What the viruses do is that they have the genetic instructions for the t-cells to start encoding an artificial receptor. It’s what Mene Pangalos, to use his analogy, described as a key. This key is fundamental in the ability of these t-cells to identify the leukemic cells in the body and start destroying them. Once this change has taken place, the t-cells are cultured in millions and infused back to the patients where they are released to the blood stream and start their fight against cancer.
Chris - Right. So you take cells that naturally in the patient’s own body are the killers that go out and destroy cells anyway. You reprogramme them by adding a piece of genetic information, which is the instructions this is how to attack your own cancer, put those cells back in and they then go round the body hunting down that person’s cancer?
Magda - Exactly.
Chris - And is it successful?
Magda - Yes. Again, that was the most exciting in terms of the results. The clinical trial that the FDA assessed and gave the green light included 63 children, and the results are that for 83% of them there was complete remission that continued for three months after the initial dosing.
Chris - To put that into perspective, we mentioned at the beginning that these are the 20% of individuals that would not previously have had any option open to them. They would have failed the primary therapy, the prognosis was grim, and so 80% plus of these individuals are being potentially saved by this?
Magda - These were the children that had no other option; they were dying. The medicine they were taking in our arsenal does not work and the cancer had returned.
Chris - Novartis did get a bit of backlash because when people heard the price - because this is estimated to be costing in the region of half a million dollars to treat each individual - people said that’s too expensive. What do you think?
Magda - These are totally new discussions and the approach that we are hearing that Novartis is taking with the US payers is the value based one. Again new in terms of pricing and reimbursement. The other alternative that these children had, and for some a treatment that had also stopped working was bone marrow transplantations which costs along the lines of 800,000. So again Novartis is offering about half the price but we are yet to see where those negotiations and discussions will lead.
Chris - It’s interesting, isn't it, because your industry started off look at bags of pills and it’s actually going to end up looking at therapies which include cell therapies in future, increasingly probably?
Magda - This is very right and, hopefully, it’s the wave of innovation that came out of the deciphering, the decoding of the human genome about 14 years ago in 2003, so I hope we’re just seeing the tip of the iceberg.

The Phuture of Pharma
with Mene Pangalos, AstraZeneca
What does the future hold for the Pharmaceutical Industry? Perhaps it could be a pill that’s linked to your smartphone? Mene Pangalos, from AstraZeneca, explains where he sees his industry heading in the future...
Mene - Technology is going to have a huge impact in our future, and one of the things that we have been thinking about is what’s next in terms of the things that will continue to improve our productivity. I think technology such as machine learning and artificial intelligence will help us in our laboratories in terms of how we optimise molecules, how we understand interactions of pathways in the cell. I think there’s going to be a huge influx of genomic data that will help us stratify disease into subsets that are going to be more amenable to drug discovery.
Then, when you look at how people use their mobile phones and their devices, you think about how you tie a medicine, to a device, to an illness where you can improve adherence to the medicine where you can improve behaviours to the illness as well as how you respond to the therapy. I think you’ll see devices becoming much more intertwined with our medicines in a way that improves both their outcome, but also adherence.

52:40 - QotW: Why does washing dry below boiling point?
QotW: Why does washing dry below boiling point?
Alex Ashcroft asked Thomas Ouldridge from the Imperial College London to hang Norm’s question out to dry…
Thomas - It is true that pure water will normally be a gas called water vapour only above 100 degrees celsius, but temperature isn’t the only factor at play here. The surrounding pressure also impacts when a substance like water can be a gas. The higher the pressure, the higher the temperature required for the gas to be stable.
Alex - Gases, like overfilled balloons, often can’t handle the pressure. But why is this?
Thomas - To exist as a gas, water molecules have to be widely spaced out. High enough pressure will tend to squeeze them back into their more compact liquid form. The more you heat water, the more energy you give to the individual molecules and the harder they can push back against their surroundings. Above 100 degrees celsius, but not below, water molecules can push back hard enough against the pressure of the atmosphere for pure water to stay as a gas of widely spaced molecules.
Alex - It’s all about the pressure then. So what’s going on when our clothes dry?
Thomas - Well, let’s consider a puddle for example. You might think it it should stay as a liquid because the temperature is below 100 degrees and the atmosphere is pushing down on it. However, we don’t only have water molecules involved; the system isn’t pure. The air above the surface of the puddle contains many other molecules such as nitrogen and oxygen. These extra molecules can actually help to push back against the surrounding atmosphere effectively lowering the pressure that must be supported by the water molecules themselves if they form a gas. It’s like many people helping to lift a weight rather than rather than just one.
In fact, there’s so much more nitrogen and oxygen they take almost all of the burden of the atmospheric pressure, and this is important. It means that any water molecules that have enough energy to escape from the puddle don’t face the full might of the atmospheric pressure so they don’t immediately liquidise. This is why some water vapour can survive in the atmosphere thanks to the hard work of the other gases, and thus we can explain why evaporation happens, and why puddles or clothes dry under normal conditions. Of course, only a certain amount of water vapour can actually be supported by the other gases, which is why things don’t evaporate immediately, and why movement of air is important if you want things to dry faster.
Alex - If you want to see this in action for yourself, like your wrist and blow on it. It dries almost immediately compared to if you don’t blow.
Thanks to Thomas Ouldridge for ironing that out. Next time we’ll answer David’s question...
Science has attempted to try and measure the intelligence of other primates, dolphins, birds, and many other species of animals. My question is: how does your averege ordinary, average, pet dog measure up in comparison?










Comments
Add a comment