Getting to Grips with Gene Therapy
This week - gene therapy. We talk to researchers using DNA technology to prevent blindness, halt muscular dystrophy, and even potentially cure HIV. Plus, what climate change means for the state of the world’s oceans, a new satellite to take the Earth’s temperature, and scientists discover the world’s first baby bottles - and the milk that was in them - from thousands of years ago...
In this episode

00:59 - The state of the oceans
The state of the oceans
Andrew Meijers, British Antarctic Survey
Recently, the Intergovernmental Panel on Climate Change published a special report on changes happening to the oceans and ice sheets. They documented widespread ice loss; highlighted rates of ocean warming, which have doubled since 1993; cited rising sea levels as major on-going and future risks, as well as climate-related hazards for coastal communities; and drew attention to shifts in the geographical ranges and seasonal activities of different animal groups. Chris Smith went to see ocean scientist Andrew Meijers, from the British Antarctic Survey, to ask him why the world’s oceans went up the news agenda this week…
Andrew - It's really the release of two important reports on how the oceans relate to climate. The first report is a special report by the IPCC, it’s the Intergovernmental Panel on Climate Change, really looking at the results of the science over the last few years on how the oceans are warming, how the ice caps are increasingly melting and sea level rise is going up. The second report is looking at how we may reduce our carbon footprint through use of the ocean. They’re basically saying that the ocean will warm considerably, the sea level will rise anything up to 80 centimetres.
Chris - And over what period are they anticipating that this would kick in?
Andrew - So the usual sort of time frame they talk about is centennial. They usually have a timeframe in about 30 years, 50 years, and up to a century.
Chris - The other report which is looking at ways that we may be able to use the oceans as a mitigation strategy, what do they set out as the possibilities?
Andrew - They set out sort of five different areas. One is the renewable energies that are basically ocean based. So things like tidal, or offshore wind. Then they talk about reducing the carbon footprint of things like shipping, increasing marine protected areas like seagrass and mangroves, which actually store a lot of carbon in the silt around their bases, increasing use of seafood which is actually less carbon intensive than things like red meat.
And finally they're talking about some of the more experimental ideas of sequestration, so sort of sucking carbon out of the atmosphere and basically injecting it into the ocean soils.
Chris - And do the IPCC go a step further and say well, if these changes we're anticipating do manifest, what will be the cost to them, as in the human cost, environmental cost? Do they make any projections about that?
Andrew - This report largely focuses on the understanding of the physics, and the impacts on the biology. The impacts that they do talk about will be extremely strong consequences that we're already seeing for coral reefs, they're very sensitive to increases in carbon, both in the water, so that ocean acidification, and also warming of the surface layer. So that will cause dramatic diebacks of areas like the Australian Great Barrier Reef. They suggest that this may put increasing stress on fisheries, so many of the global fisheries are already overexploited or at their maximum capacity. The extra stress that ocean warming will be putting on food chains and ecosystems is likely to have significant impacts, and so reduce our ability to take food from the ocean.
Chris - That sounds at odds though, with one of the mitigation strategies, which was better exploitation of the oceans as a low carbon food source. So if we've got a resource that's already overexploited and one which is going to come under increasing pressure. Sounds like a double whammy for the ocean.
Andrew - Yeah absolutely, they do caveat that when they say we should be moving towards, sort of lower carbon foods, things like seafood for example, by saying that they have to be sustainably fished. So that goes hand-in-hand with things like marine protected areas, where you basically set up areas for fish to reproduce where they won't be exploited. And that basically gives them a physical area where they can reproduce safely, which then gives a population an area well effectively, where they’re not going to be fished to extinction
Chris - And you're going to go home and get an early night tonight because you're up early tomorrow. Where is it you're off to?
Andrew - Right yeah, I'm off to Birkenhead, near Liverpool, which is where the new UK polar research vessel, the Sir David Attenborough, also possibly known as the Boaty McBoatface, is going to be launched. There'll be royals there. So David Attenborough himself will be there, it will be a very exciting day for all of us.
Chris - Is the ship actually ready?
Andrew - So it's not quite ready, it's going to be named and officially “launched”, but there's still a reasonable amount of things to do, there's a bit of interior design, bit of wiring, but the ship is essentially there and ready. Sea trials will commence soon, where basically they'll drive it into the ice and see how much it can break to get its official ice class, which will be exciting. And then next season, or the next Antarctic season which is the 2021 season, it'll be down around Antarctica doing its logistics works for the British Antarctic Survey.
Chris - Who gets to break the champagne?
Andrew - I'm not sure if I'm allowed to tell you this but I believe it's William and Kate, and I think Kate gets to press the button.
05:52 - Taking Earth's temperature
Taking Earth's temperature
Helen Brindley, Imperial College London
The European Space Agency (ESA) have this week announced a new project to take the Earth’s temperature. Scheduled to launch in 2026, it’s a satellite dubbed FORUM, which stands for “Far-infrared Outgoing Radiation Understanding and Monitoring”. Its job will be to measure, for the first time, the energy emitted from Earth in the far-infra red part of the electromagnetic spectrum. The purpose is to help build better models of how the climate will change in future. Katie Haylor spoke to mission scientist Helen Brindley from Imperial College London...
Helen - We have a lot of satellites in space, and a lot of them measure the Earth's outgoing energy at wavelengths in the so-called mid-infrared. However, a lot of the energy emitted by the Earth is actually at longer wavelengths. And what we're going to do with FORUM is measure them for the first time. And these energies actually comprise about 50% of the Earth's greenhouse effect if our models are correct, and we really haven't measured in the far infrared at all. And we think that when we go and measure over there we'll actually get some surprises about what we see. The energy in the region is very strongly controlled by water vapor absorption and also by ice clouds, which we've recently realized they’re much more widespread than we originally thought, and we're not entirely sure whether they heat or cool the planet.
Katie - Is it too crude to say the aim is to quantify how much energy there is in this far infrared bit of the spectrum and where it is?
Helen - Pretty much, yeah. To test how much is there, what it looks like spectrally, and tying those signals to actually what is happening in the atmosphere and at the surface at the same time.
Katie - Tell us a bit about the satellite then, what kit has it got on it to allow it to get the data that you're interested in?
Helen - Two instruments. One is the interferometer - essentially moving mirrors which introduce path differences into the light beam going through the instrument and essentially allow you to measure the energy distribution that's coming into the instrument. And that gives us the actual spectrum. And then there's a second, simpler instrument on board which is an imager. So this measures across a narrow band of frequencies or wavelengths and is there really to tell us at higher spatial resolution how homogeneous the scene is underneath. So it gives you an idea of what we're looking at; are we looking at clear ocean, are we looking high ice cloud, or are we looking at a mixture of different scenes.
Katie - So once you have measurements of this far infrared energy how will that translate into us better being able to predict climate change in the future, because that's the overall aim, right?
Helen - That's right. With our climate models at the moment, when we compare them with standard metrics of what the climate is doing, like, for example, the global mean surface temperature, historically all the models do rather well. But as you go into the future, no matter what scenario you consider, whether it's one where we keep going as we are at the moment, which is what we call ‘business as usual’: pumping out quite a lot of greenhouse gases and not doing too much about it, or whether we go to a scenario where we start transitioning to a more green economy, the models diverge as they go into the future, so that there is a large spread in their predictions, and we're really not sure which one is right.
What we hope to do with these measurements is use them to help establish which models now are doing well for the right reasons. So at the moment they are essentially tuning the models to broad band measures of the energy balance, so the total amount that's being emitted. When you start looking at the energy distribution, you get a better idea of how that energy is being emitted and the processes that are going on within the climate system, which are therefore important for what's going to happen into the future.
So we think these measurements will help us understand those processes better and therefore understand which models are doing well for the right reasons, and we can have more confidence in those models moving towards the future.
Climate feedbacks, things like water vapour and whether the distribution of clouds are going to change and things like that. These are the things that we think are causing the large uncertainty in the future. And if we could pinpoint those feedbacks and understand them more, then we'll be able to reduce the uncertainty moving into the future and that's what we think what we have to do with FORUM and for some of those feedbacks.

10:59 - World Heart Day
World Heart Day
Sai Bhagra, Royal Papworth Hospital
Sunday 29th September was World Heart Day. But sadly, despite the fact that we’re better than ever at treating people with heart problems, the number of people waiting for a heart transplant has reached a record high - and doubled in a decade. Sai Bhagra is a cardiologist from Royal Papworth Hospital, one of the country’s leading transplant centres...
Sai - As you said, Chris, heart failure is becoming a growing epidemic. It is the end stage of all heart conditions. And we've got very good at treating heart attacks, and as a result you have patients who have heart pumps that are not working as well as they would have, and they've lived longer. This number is growing, there's about 60,000 new cases added in annually in the UK alone. 10% of these will progress into advanced heart failure, and transplantation is a treatment option for a select few of these.
Chris - So there's a range of different conditions which can result in heart failure, and some cases of heart failure, we just run out of road when it comes to drugs - and we only have one option, which is to put a new heart in these people.
Sai - Putting a new heart is an option for not everybody, unfortunately, because we have an organ availability and patient demand mismatch.
Chris - So how do you make that decision?
Sai - We assess the patient to see if they’re sick enough to need a transplant. Transplantation comes with its own issues: it has a mortality rate of 10-15% in the first year. So what we're looking to see: is the patient sick enough to need a transplant, but well enough to survive the operation.
Chris - And what's actually involved in doing a cardiac transplant?
Sai - What we do first is assess the patient with heart failure to see if they are suitable to go onto the transplant waiting list, and then it's a matter of making sure the patient remains stable and well enough for their operation. The waiting time on the routine transplant list in the UK is up to two and a half years, so patients can die waiting for a transplant. And the patients who get successfully transplanted end up having 14-15 years added on to their life, of good quality.
Chris - And how do you decide which heart goes in which person?
Sai - Well the heart has to be matched to the patient. So the heart has to be functionally normal - it has to have no structural disease - it has to match on blood group, it has to match on size and tissue typing. It's only then we tend to use the heart for the particular recipient.
Katie - Sai, Chris mentioned that the wait for a heart transplant has reached a record high. Why are waiting lists so long at the moment?
Sai - The waiting lists are long ‘cause we don't have enough hearts to go around.
Katie - So what can we do then?
Sai - Well, what we can do is get more people to express their intent to donate. The laws are changing, it's going to be an opt-out scenario come spring next year.
Chris - At the moment we assume someone is not a would-be donor. And we're going to start assuming, if someone is a potential candidate donor - they've got what looks like a healthy heart, something else has gone wrong with them - they’re heart donor until proven otherwise.
Sai - Unless they have explicitly said that they do not want to donate.
Katie - But is it that simple though? Because from what I understand, you also need to get the consent of the family. Is that correct?
Sai - I think the family consent is still key. So if people are wanting to donate, then the key thing for them to do is to express it, express their intention to their family so that the families can respect their wishes.
Chris - And if you have a potential donor, how do you decide that their heart is worth transplanting?
Sai - It's assessed on multiple parameters. We look at it on echocardiography, we look at it on imaging to see how it's working, we assess it haemodynamically. If it passes those tests we then look for coronary disease, and if it's still working well then we use it in our recipient.
Chris - Because in recent years the liver doctors who are doing transplants have been able to enormously widen the pool of livers they can use, because they've been able to rescue organs that they previously would have discarded by, for instance, putting them in an organ bath and perfusing them and giving them some recovery time before they chuck them into a new patient. Is there anything similar for cardiac transplantation that could be used to widen the pool of organs you have there?
Sai - So we are attempting to widen our pool. At Papworth we have the world's leading experience in using hearts that have been taken from donors whose hearts have stopped beating. Conventionally hearts are from people whose hearts are still beating and they are ... brain stem dead, but using a DCD heart - where the heart’s obtained after the heart stopped beating - we recondition the heart on the OCS machine…
Chris - What’s OCS?
Sai - It’s the organ care system, it’s similar to what the liver and the kidney teams are using. And we find that at Papworth, we have roughly increased our transplant numbers by 40%.
Katie - What is the outlook for somebody who's had a successful heart transplant? How long could they expect to be around for?
Sai - So what we state is, if you have survived the first year - which is where the mortality rates are the highest - then you're looking at an average of 14-15 years post-transplant, half of our patients will be alive at that stage. Our longest survivors, out at 35 years post-transplant now.
Chris - I think, was that a lady? Because I think she...
Sai - A man.
Chris - Oh, a man. There was definitely someone I saw give a talk, and they were inspiring.
Sai - It's 40 years since we started transplantation at Papworth.

15:54 - See bike say bike
See bike say bike
Peter Chapman, University of Nottingham
Have you ever had a SMIDSY, or even a near-SMIDSY? To explain, Chris Smith spoke to Peter Chapman, from the University of Nottingham, who has been looking at the cause of one of the commonest types of road accident...
Peter - One of the nastiest types of crash on the road, is when you're driving up to a junction in a car, you look right, look left, look ahead, pull out, and then smack, you're hit by a vehicle from the side that you hadn't seen. Typically it's a motorbike that hits you. And they were just driving along minding their own business and you'd pulled out in front of them. This happens so often that motorcyclists have a special name for them. SMIDSY crashes; “Sorry mate I didn't see you.” Which is what the driver says iIf they've got someone to talk to, very often the motorcyclist doesn't survive that kind of crash. About 90 motorcyclists in the UK die in that kind of crash every year. But it's also a real psychological mystery what's gone on here.
Chris - Indeed, why has the driver, despite looking right and left, by and large missed them? How did you try and get underneath why this is happening?
Peter - Well we started using a high resolution driving simulator, where we could really put people in just the right sort of situation, and we recorded their eye movements, so we could see exactly where they were looking around as they came up to junctions, and we got people driving through hundreds of junctions, looking around, making decisions as when it's safe to go. And then every now and again, we just stopped the simulator, just as they pulled out and we asked them, “what's around you, describe the vehicles.” But a weird thing that happened is quite often, there'd be two vehicles coming, one from the left, one from the right, and the person would say, “I remember a car on the left it was a blue car it was about there.” Then we’d say, “anything else.” No, they'd say. That was weird because we used the eye tracker. We could see them, just four or five seconds earlier looking straight at a motorbike coming from the other direction but they'd forgotten it.
Chris - Now we know there is this phenomenon of inattentional blindness. People do various demonstrations of this, where they ask you to count someone bouncing a ball and in the background there's a gorilla skipping through the picture, and they don't even notice it. Is it just a manifestation of that that's going on? The motorbike is quite small, there's lots of other distractions, so they just ignore it?
Peter - We're very used to that kind of explanation, that you haven't taken in the motorbike. But the surprise for us is, when we looked at what predicts whether you do remember the motorbike, it's not whether you looked at it, or how long you looked at it for, it's what you do afterwards. So the more things you look at after the motorbike, the more likely you are to forget it. Now that looks like forgetting, not a failure to attend to it in the first place.
Chris - Does this mean then, that when people say there's too much roadside furniture, too many distractions, too many things to look at, actually they've got a point? We are potentially making the roads more dangerous by cautioning people about everything.
Peter - Well the issue there is how selective the driver is. If the driver looks at the right things, and attends to the right things, then there isn't a problem. If however, you make the junction so complex that they need to look at lots and lots of different things, that is going to be more than they can remember.
Chris - Does the research highlight any interventions that we could meaningfully make though? Because when you're with your driving instructor, they dutifully say to you, “mirror, signal, manoeuvre.” Should that be, “mirror, signal, motorbike, manoeuvre”, or something like that? Is there any kind of thing we can drill into people that would reduce the likelihood of this sort of accident happening?
Peter - Well I do have one suggestion. So it looks as though this error is a limitation in short term memory. Now what we do know about short term memory, and we've known since the 1960s, is that you've got two types of short term memory that are essentially independent systems. You've got visuospatial working memory, for the things you look at and you've got phonological short term memory. That's a verbal form of store for things you say. The two are separate. So I've suggested that if you're at a junction and you see a motorbike or a pedal cycle coming, you just say aloud or under your breath, “bike”, that will automatically encode it in phonological working memory. That gives you extra capacity, essentially doubling the amount of stuff you can remember. See bike, say bike could be a simple intervention that might make a big difference.
Chris - So the bottom line then would be; motorcyclists should do their best to be as obvious and eye catching as possible, which most of them do, don't they? Drivers should be drilled to not just say, “I'm approaching a junction”, but to call out, “I've seen a bike”, and remind themselves they've seen a bike, and perhaps also not just look right and look left, but do it again.
Peter - The key thing I think drivers have to realise, is that their short term memory isn't as good as they think. We all have the idea that we can remember everything around us, but you only have to trust your memory for something you're not looking directly at to realise that you don't actually have that memory. And that's what's going on at junctions. People assume that they would have remembered something if it were there. So they pull out. I think drivers need to realise that actually, it's harder than that. If you want to remember something you've got to work at it, and saying bike is a good way of working at it, that guarantees you will remember it.

21:49 - Prehistoric baby bottles
Prehistoric baby bottles
Julie Dunne, University of Bristol
Time to wind the clock back thousands of years, because scientists have found what they believe are the world’s oldest baby bottles. These tiny clay pots with spouts have been found all over Europe, and some date back over 7000 years ago. But no one was really sure what they were for. Now, archaeologists have managed to analyse the residues left by the material they once contained, helping to solve the puzzle. Phil Sansom heard from the study’s author Julie Dunne what their results say about ancient human societies...
Julie - So what we've discovered is essentially the first and the only evidence for the types of foods that prehistoric mothers were feeding their infants. And we discovered this in lovely little evocative baby bottles. Archaeologists have been coming across them firstly in the Neolithic in Europe, so that's about 7000 years ago, and then in the Bronze Age and Iron Age, and they’ve become a bit more common then.
Phil - And what do they look like? Are they like small teapots?
Julie - They're normally around about 10 centimetres wide and they have a spout, but they vary enormously. Quite a few of them are made in the shape of mythical animals.
Phil - Did you find a particular two or three that you wanted to look at?
Julie - Yes we did find three. So they actually were dug up some 20 or 30 years ago from a site in Germany and Austria.
Phil - What did you do to actually figure out what these are being used for?
Julie - Essentially how we find out whether they were to feed children was to go and look in children's graves, and they are very unusual to find. We had quite a search to find a few graves and find the vessels that had been contained within them. So just to explain, if you think of an unglazed ceramic pot, and if you were to put some water in it, and then some meat and boil that up, you would literally see fat floating on the top. It's these fats that absorb into the ceramic matrix of the pot. And very luckily for us, they sit in this pot for thousands of years, over archaeological timescales. So what we do is we use a technique called organic residue analysis. And normally we take broken pot shells from archaeological sites and grind them to a powder, but we couldn't do that in this case because they're so small and so precious so we couldn't half destroy them. So we make clean a little bit of the surface of them, just to remove any contamination from handling. And then I drill down enough powder to sample. I have to say it's quite nerve wracking when you're doing that to something you know is that old and that precious.
Phil - Then what do you do once you drill down a piece?
Julie - What we do is we use a methanolic acid extraction and this releases the molecules which are called lipids, and these are the fats and oils and waxes of the natural world. We then put them on what we call a gas chromatogram. And that tells us whether there's anything there. Once we've done that, they go on to a mass spectrometer and that tells us what the compounds we found are.
Phil - To clarify, you weigh it effectively in that mass spectrometer.
Helen - Essentially.
Phil - And what you get out matches what these animal fats should look like.
Helen - There's actually another step to that. What we need to do is look at the stable carbon isotope values of these particular fatty acids, and it's that that allows us to differentiate between types of fats. We can differentiate firstly between ruminants. So that would be cattle, sheep and goat. We can identify the difference between their meat and their milk. Other techniques enable us to find the processing of aquatic products, we can identify plants, and also the presence of beeswax which denotes honey processing. It's really based on the physiology of the animal.
Phil - And so when you looked at the fats that you found on these clay pots, what did you find?
Helen - Fascinatingly, all three pots contained ruminant milk.
Phil - That's cow or …
Helen - Cow, sheep or goat, yeah
Phil - You can't tell which one?
Helen - No, because their physiology is basically the same.
Phil - Okay, but it means that these kids from 7000 or so years ago were getting fed cow or sheep milk.
Helen - Yeah which is amazing.
Phil - What does that say about society back then?
Helen - So this all ties in to what begins to happen in the Neolithic at about 10000 years ago. People start to settle down, they domesticate animals and they also start to grow crops. This changes the way prehistoric mothers could feed their babies. Hunter-gatherer mothers tend to give birth every five years, but Neolithic mothers have much shorter inter-birth intervals, they tend to give birth every two years. And that's because of the availability of these foods. They're on these people's doorsteps, they’re on tap, and you're having more babies, the population increases dramatically. We call this the Neolithic Demographic Transition. People start moving out across Europe. This leads to larger settlements and eventually to the growth of cities.
Phil - So it's like, if you've got milk from other animals you can have more babies. This is like the missing link to humans growing.
Helen - Essentially, yeah. In a way, that's why we're here today.
Phil - What about the fact that they've spent so much time making these pots, what does that say?
Helen - When a prehistoric mother or father perhaps is giving their infant this little pot, they're not just giving the child a pot to drink from, they're giving them some little object that's probably going to make the baby smile or laugh, they're incredibly cute. And I think it tells us an enormous amount about the love and the care and the attention that these prehistoric parents would have had for their babies.

29:41 - What is gene therapy?
What is gene therapy?
Phil Sansom
This week, we’re looking at the enormous medical potential now being realised by gene therapy. We’ll be hearing how these approaches can battle blindness, halt Duchenne Muscular Dystrophy, and even cure HIV... but first, what do we actually mean by “gene therapy”? Phil Sansom is here with the quick-fire science...
Phil - Most diseases that you can get have their roots in your DNA, but ever since medicine began, treating those diseases hasn't actually involve tackling those root problems. That is until 40 years ago when doctors successfully inserted new DNA into five people to help treat their melanoma. Welcome to a new type of medicine; gene therapy. So how does it work? Well a gene is a bit of DNA, and there are different ways a gene can malfunction to give you a disease. So different types of gene therapy might do different things.
One treatment might replace a harmful mutated gene with the non-mutated healthy version, or if the mutated gene isn't vital the treatment might want to stop it from working altogether. That's called knocking it out. In other cases your body might be totally missing a gene that you need. Gene therapy in this case could just add it back in. Here's the problem though; to efficiently add bits of DNA into your cells, you usually need some kind of vector.
Certain viruses are really good vectors because that's how they infect you anyway, by inserting their genes into your cells to hijack them and make more of themselves. Gene therapy can exploit that by modifying the virus, stripping out the viral genes, and replacing them with useful gene therapy ones instead. But putting foreign material like viruses into your body can be risky. It can trigger your immune system to attack, potentially leading to lethal inflammation. Plus there are other risks too. With some therapies, there's a chance that messing with your body's genetic code could cause cancer. That's why right now, doctors are moving cautiously and they usually prioritise diseases with a bad prognosis and no other cures. But for those diseases it can be a lifeline.
And as it gets safer gene therapy looks to become a pretty powerful tool.

31:40 - Gene therapy for Duchenne Muscular Dystrophy
Gene therapy for Duchenne Muscular Dystrophy
Sue Fletcher and Steve Wilton, Murdoch University
One very promising area for gene therapy is in the muscle-wasting disease Duchenne Muscular Dystrophy, which affects about one in every three thousand males. It targets boys because the affected “dystrophin” gene is on the X chromosome, and boys have only one copy of that. If their version of the gene doesn’t work properly, their muscles fail. Previously, there was no way to treat the condition. But now, working at Murdoch University in Western Australia, Sue Fletcher and Steve Wilton have developed a genetic therapy that can “cover up” the damaged part of the gene so the muscle cells can still read the rest of the message and produce a working form of dystrophin. Chris Smith spoke to them...
Sue - Duchenne M.D. is an inherited muscle wasting disease that is usually evident in affected boys around two to five years of age. They walk late, over the age of two, and they have difficulty climbing stairs. They often walk with a little bit of a waddle and they struggle to keep up with their peers.
Chris - And what is actually going wrong in them to make that happen?
Sue - So these boys have a mutation in the dystrophin gene that is located on the X chromosome. Girls have two copies of the X chromosome while boys have only one, and therefore if the single dystrophin gene is non-functional, the essential muscle protein dystrophin is missing. The muscles become very prone to damage and although the kids appear healthy at birth they have these delayed motor milestones and they lose the ability to walk by twelve years of age.
Chris - And what's the ultimate end point for these kids?
Sue - Well all muscles are affected, including the heart, and they usually will succumb to either respiratory failure or cardiac failure in their 20s, sometimes in their 30s, DMD a life limiting disease, it's fatal.
Chris - And Steve, what's the intervention that you and Sue have pioneered here to try to intervene in the process?
Steve - As you mentioned, the problem is a mutation or a spelling error in the genetic instructions for a gene called dystrophin, and the actual gene product acts like a little shock absorber. The ends of it give strength and stability to the muscle fiber. As you can imagine, any spelling error that stops the synthesis of this protein, you end up with a one-ended shock absorber and it can't work. Our approach is to design a drug that acts as a genetic white-out, or a correcting fluid for the gene message. We cover the disease causing part, so we can make a shock absorber that's a bit shorter in the middle. But the ends are intact, then the gene can be translated into a protein that is going to be functional.
Chris - So in essence then, it's almost like a genetic sticking plaster, you can actually put this into cells and when the gene is read, the cells don't see the broken bit of the gene they just see your sticking plaster, which is the correct message, and it skips over or jumps over the broken bit fooling the cell into just reading the whole thing almost, and you get a healthy protein or nearly healthy protein.
Steve - That's right. It's like a genetic Tipp-Ex.
Chris - And Sue, how do you get this treatment into the body?
Sue - The treatment is not the most convenient of treatments. It is delivered by a once weekly intravenous infusion and it's quite a long slow infusion.
Chris - And does that mean then, that when you inject this drug it goes to every cell in the body even though it's only the muscles which are affected, and does that have any consequence?
Sue - You're correct. It goes into the bloodstream so it's distributed throughout the body. But the beauty of this kind of treatment is it can only have an effect where that gene is being expressed. So if the gene is not working in a cell, like in a skin cell or a liver cell, the drug won't do anything. It can only work in muscle where the dystrophin gene message is active.
Chris - And when you do this Steve, what actually is the consequence for the muscle cells that pick up your drug?
Steve - One of the problems is that only a little bit of the drug gets into the cells. The uptake at the moment is a real problem, but the little bit of protein that's being made is making a very substantial difference. Boys, young men now, who should be in a wheelchair, are still walking, respiratory functions have stabilised, and declining much slower than they would in untreated boys. So it is working, but we have to make it work a little more efficiently, and that's why we’re improving delivery or increasing the potency of the drug. And these studies are ongoing.
Chris - And Sue, how many patients have you treated so far?
Sue - The trials and the drug now is on sale in the USA. I don't have a number of patients who have been treated overall, but the original trial involved twelve boys aged between 9 and 11, and that's kind of the time when most of them would be expected to be slow, their walking ability would be declining pretty rapidly, and they'd be mostly expected to be off their feet by 12 years of age. We never expected that the drug would reverse the disease. We did hope it would slow the decline or partially stabilise it. And Billy who is the star of trial, or one of the stars of the trial, he's over 18 years, so he's been treated for over nine years now and he walked to the stage at his graduation. This is unprecedented in a boy with Duchenne.
Chris - Indeed because I've actually met Billy, because you brought him to Western Australia to a conference you were presenting at. And this is a few years ago now. He actually ran into the room
Sue - Yes, that's Billy
Steve - With his type of mutation, He should have stopped walking at eleven point one years of age. According to statistics.
Chris - So how does that make the pair of you feel then, I mean you must be delighted?
Steve - Chuffed, and also overwhelmed because we want to make this work for so many other kids. The treatment is designed for one type of mutation. We've got treatments for many, many different types of spelling errors in the gene. And we really want to see that out there.
Sue - As a researcher, it's an extraordinary position to be in, to actually see somebody whose life has been changed by the work that our group have done.
Chris - And any side effects of using this therapy?
Sue - All drugs have side effects, so the pain at the injection is a side effect of the treatment. But to date, there have been no drug related serious side effects which is really quite as extraordinary, it’s largely to do with the chemistry. It's neutral, so it doesn't stick to things very well, which is why it's not efficiently taken up by cells. But to date, there is no evidence that this drug causes any adverse effects on the cells. These boys are being treated for nine years with no side effects.
Steve - The most serious side effect I've heard of so far is a broken ankle, he was running!

38:51 - Gene therapy for blindness
Gene therapy for blindness
Imran Yusuf, Oxford University
If the eye is a camera, then the retina at the back of the eye is the light-sensitive “film”. It contains the crucial light-sensitive “photoreceptor” cells - known as “rods” and “cones” - that convert the light hitting the retina into electrical impulses the brain can interpret. If we lose the rods and cones, we can go blind. And this is what happens to people with a genetic condition called retinitis pigmentosa. Katie Haylor caught up with Oxford University’s Imran Yusuf who told her more about the disease and how he’s working on gene therapy treatments to stop it...
Imran - Initially it causes the rods, which allow us to see at night, to die off mostly. Peripheral vision often becomes affected too. And in the later stages it also affects central vision, which means that their ability to read and to recognise people becomes affected.
Katie - I've heard that there's a recycling issue going on in the eye.
Imran - Absolutely. So when light creates a chemical change within the eye, the eye then has to recycle that chemical so that it can receive light again. That's why when you look at a bright light and you look away, you get this black blob in your sight. That's because the eye is recycling these pigments so that it's then ready to receive more light. Any errors in these particular visual cycle chemicals are a prominent cause of retinal degeneration because they're so important for sight. And in particular, the first gene therapy treatment is available on the NHS now for a gene which encodes one of these visual cycle proteins, the recycling as you mentioned. Because it's a common cause of visual loss in children, often very severe loss of sight, and so it's very encouraging that there is a gene therapy treatment available on the NHS for these patients in the very near future.
Katie - What are you putting into the eye?
Imran - In the particular case that I mentioned... that's caused by a gene called RPE65 and the protein that it produces. So this protein is involved in the visual cycle and the recycling. So the gene therapy virus that we create in order to deliver genes to cells, we inject it underneath the retina. What that allows the virus to do is to enter the cells which we want it to enter into, which are either the light sensitive cells or the retinal pigment epithelium, and it delivers the copy of the gene that we've programmed it to express.
Katie - What kind of viruses are they?
Imran - A cousin of the common cold virus. These are viruses which generally are not disease-causing in humans. Viruses normally work by entering cells and reproduce copies of themselves, but we re-engineer that virus to instead produce a healthy copy of the gene that the cell is lacking. And the elegance of gene therapy is that it should only require a single treatment because we’re programming their cells to produce what those cells are lacking.
Katie - Does this cure or does it prevent further damage or both?
Imran - For gene therapy, the hope traditionally has been that we would stop the degeneration happening at the point at which that therapy was given. But in the clinical trial that's been taking place in Oxford under Professor Robert MacLaren, in the initial group of 18 patients who were treated with gene therapy, six out of the 18 showed an improvement in their visual function. That's at one month after treatment. And this is something really quite new for Retinitis pigmentosa. If it can be shown to be sustained in the later parts of the trial this is hugely encouraging.
Katie - You said the cells are dying. Does it work if they've died?
Imran - It's difficult to say that. I think the perception is once the cells have died, we can't replace them, at least not with gene therapy but we can intervene in cells that are, as you say, dying. So cells that would otherwise die, had there not been an intervention.
Katie - You are putting foreign material and a virus into the eye. Is there a danger of the immune system reacting to that or indeed that people could become immune to the treatment?
Imran - There are a couple of things which are in our favour in retinal gene therapy. The first is that the immune system doesn't see foreign material in the eye in the same way as it would if you injected it into the blood for example. That’s one big advantage. The second is that we try to make the genetic material within the virus as efficient as possible so that we can reduce the amount of virus that goes into the eye. The third thing is that we can inject the virus underneath the retina which is more hidden than injecting virus inside the ball of the eye, which is another approach for gene therapy that other people use. And the fourth thing is that we can use anti-inflammatory agents at the time of giving the injection which we then can stop in the weeks afterwards, which will dampen down the immune system just in that period in which the virus is doing what it needs to do. But you're right, the inflammatory reaction could be a concern particularly when very high doses of the virus are needed.
Katie - Could this same kind of approach be used for other eye conditions?
Imran - Absolutely. Really the floodgates have now opened. Now that we've shown that you can use a virus in this way to deliver a gene product, now the possibilities are very wide, not only for treating diseases caused by a single gene problem - they’re often good ones to work with because it's very obvious what gene needs replacing. But then you have other genes which are faulty in more complex ways and those need very specific approaches. In the era of gene therapy the possibilities are so wide for so many conditions. It really is an exciting time to be in the field.
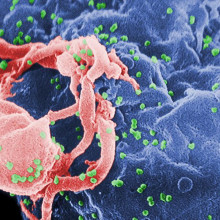
44:28 - Gene therapy for HIV
Gene therapy for HIV
Ravi Gupta, Cambridge University; Michael Pepper, University of Pretoria
Around the world, almost 40 million people are living with HIV. It grows in and progressively destroys the immune system, leaving victims highly susceptible to what would normally be trivial infections. Now, after decades of effort, scientists are finally beginning to cautiously use the C word: “cure” - and gene therapy is likely to be central to the approach they’re taking. Infectious diseases specialist Ravi Gupta from Cambridge University and University of Pretoria physician and molecular cell biologist Michael Pepper told Chris Smith and Katie Haylor about their research in this area. First up, Katie asked Ravi, what does HIV actually target when it gets into the body...
Ravi - So HIV is what we call a retrovirus which means that it infects cells, as many other viruses do, except this time rather than just making copies of itself, it actually integrates into the genes or chromosomes of the individual so it's there permanently.
So this is why HIV is a disease that doesn't go away and could not be cured until recently because of this latent phase that we refer to. Now this happens primarily in white blood cells that are there to protect you. They're called lymphocytes and they have a protein called CD4 and this is a protein that HIV absolutely requires to gain entry to a cell. So that's why it's only able to infect a CD4 positive T cell.
Chris - And by growing in those cells and destroying them in the process, it's going to leave that person with a dwindling population of the cells that are a lynchpin part of the immune system?
Ravi - That's right, CD4 cells orchestrate the entire immune system and so once they start disappearing you get susceptibility to not only infections but cancers.
Chris - And how did you cure, in inverted commas, your patient?
Ravi - We were able to identify an individual who unfortunately due to advanced HIV infection developed Hodgkin's lymphoma which is a recognized complication, because our immune systems defend us against cancer in our everyday lives.
And so this individual had end-stage cancer that was not responsive to any chemotherapy that we used and the only option left for him was a transplant using cells from a donor who was already immune to HIV. And we know that certain individuals are immune.
Chris - Why was that person immune to HIV, the donor person?
Ravi - Around two decades ago, we identified a second receptor or protein that HIV absolutely requires. This is called CCR5. So you need both CCR5 and CD4 for the virus to enter cells.
Chris - So that's sitting on the outside of the cell. It's almost like a stepping stone for the virus to be able to grab hold of and then get into the cell and if that's not there the virus can't invade.
Ravi - Absolutely. And so we realized that around 1 percent of individuals have two mutated copies of CCR5 in their genes and therefore they cannot be infected.
Chris - And hence if you put that bone marrow into your patient and they then build a new immune system from that person's HIV resistant cells, they can't then mount an ongoing HIV infection.
Ravi - Absolutely.
Chris - And that's what you believe has occurred in this patient?
Ravi - That's right. There was a patient who needed a transplant from a donor and for that to work you need to give high doses of chemotherapy to clear the patient's own cells, to allow the incoming cells that are resistant to HIV to then take hold and to populate the blood.
Chris - I suppose Michael that the problem with the strategy that Ravi is outlined here, is that, as he says, only a tiny minority of people naturally have a bone marrow with that particular genetic configuration that's resistant to HIV. So this wouldn't be a practical solution for the 40 million or so people who are currently infected with HIV.
Michael - Absolutely Chris. The problem is amplified here in sub-Saharan Africa where we have a huge genetic diversity. And to find somebody who has an adequate match and is also deficient in CCR5 is really very very difficult. So our approach is to try and engineer cells that we're going to give to patients in order to make them resistant to the virus.
Chris - So it's a similar sort of strategy in the sense that Ravi is putting into a patient a set of cells that are resistant to HIV, albeit from a donor. You're saying “can I take a person's own cells or even get donor cells and change them in some way to make them resistant, so when they go in that person's immune system can be rebuilt from those cells and their own virus can attack them.”
Michael - The idea is to take the person's own cells, engineer them outside of the body so that they don't express CCR5, and then create space in the bone marrow so that when you give them back to the patient they can take up residence and start producing an immune system which is resistant to HIV.
There are many techniques that are being used to do this. One of probably the most topical at the moment is gene editing, to edit out CCR5 from the cells that you're going to give back to the patient. And then there are other techniques, such as the one that we're using, which is to try and prevent the protein from being expressed and therefore the docking element on the surface of the cell would be absent.
Chris - So you're saying you manipulate the cells in a dish, having collected them from the patient. So you've got HIV uninfected cells and you manipulate them to remove from the cell that lynchpin protein that Ravi was talking about, the CCR5 that the virus would normally need to get in, and then you can put those cells back into the person and they then become the source of their immune system?
Michael - That's correct Chris. I think that's the technique that everybody is working on at the moment all over the world. In sub-Saharan Africa the question is going to be one of capacity and of course cost. So it was very exciting to hear Sue and Steve speaking earlier about their approach, which is to directly introduce the material that is going to do the gene therapy into the patient's bloodstream and that either the virus or the DNA would then have its effect on the target cells. And the hope is that in the long run, particularly in this part of the world, that we'll be able to do away with engineering the cells outside of the patient's body, and simply add the virus which is carrying the machinery necessary to engineer the cells or the DNA directly into the bloodstream of the patient.
Chris - Have you got evidence that this will actually work in a patient yet though?
Michael - So we have evidence in mice that have a human immune system, and we can achieve a functional cure in these mice. There are people working in other parts of the world that have done the same thing and there have recently been some publications from other people who've showed that gene engineered cells do persist in the body of people in whom CCR5 has been removed from the target cells.
Chris - Ravi what do you think? Does this sound plausible to you?
Ravi - Certainly I think that the theory is there. The problem that is going to emerge is that without use of chemotherapy to essentially remove existing cells, it's a question of a relatively small number of engineered cells being introduced or being modified. The problem is that HIV can then just go into the cells that have not been modified. And so that's the big problem we have.
Chris - So I guess what you're alluding to is what Michael was saying about making space in the bone marrow. So Michael presumably you've got to give patients bone marrow toxic drugs to wipe out some of their normal bone marrow, to make space for your modified cells to come in. And I should say it's probably a bit of an ethical dilemma isn't it? Because we're quite good at treating HIV with drugs at the moment. And you're saying give people more poisonous drugs and a risky procedure, when they're not actually ill at the moment.
Michael - Hopefully there are agents other than toxic chemotherapeutic agents that will be useful in the future, to open up a niche in the bone marrow. There is work going on in several areas around the world.
But there is an alternative. And that is to use T cells. So you may have heard about CAR T cells which have been used very successfully for the treatment of leukemia and lymphoma. And people are now moving in the direction of creating CAR T cells that would be used for HIV.
Chris - This is the Chimeric Antigen Receptor T cells it isn't. It's where we modify the cells to endow them with a very specific, targeted, receptor that recognizes one thing we've programmed them to go after.
Michael - That's correct. Should this be successful, it would no longer be necessary to open up a niche in the bone marrow. One would simply remove the T cells from the patient, engineer them and give them back. And these cells are pretty long lasting.
Chris - Ravi? Your thoughts?
Ravi - Yes I think there is huge amounts of effort going into different approaches for modification and of course knocking out various populations of cells. So I think it is a very exciting field at the moment. I think what's incredible is that infectious diseases and cancer, for example, are sharing a lot of technologies and there are more similarities than we ever really appreciated in the past. I think that's a wonderful thing.
Chris - Ravi, we've talked a lot about deleting this CCR5 gene that HIV uses to clamber inside the cells it wants to hit. If you take that away, does that not render a person at any kind of disadvantage or less healthy than people who have that gene? Presumably it's there for a reason.
Ravi - That's a really good question. I think that it's been uncertain for a long time. We postulate that this mutation emerged as a natural or a process of natural selection, potentially because of infectious diseases such as smallpox or one of the other postulated things was the plague.
But for whatever reason this mutation has persisted in the population without apparent deleterious or harmful effects. On the other hand, a recent study published in Nature Medicine suggested that people with the double deletion in both copies of the gene lived on average a year and a half less than those who didn't have it. Which throws into question whether it's going to be safe or not.
Chris - And Michael, returning to the therapies that you're alluding to, both doing these genetic manipulations and putting stem cells in, and also using these CAR T cells, these modified T cells to go after HIV. It sounds wonderful and we know that we can do this for certain diseases, but can we afford it? Because there are 40 million people with HIV. They're not rich people. They're not in rich countries.
Michael - Chris that's the key question for this part of the world, where a large part of health budgets go towards providing antiretrovirals for the 7 million or so people in South Africa that are affected.
Gene therapy is expensive. If you do a health economics analysis though, the cost of HIV is enormous. And I'm not including the cost of the antiretrovirals, I’m including the cost of the complications that arise such as cancer and infectious diseases. The cost to society where we have child-headed households in South Africa, and all of the social complications that come as a result of that.
I think as the procedures become refined, and as we can move to cheaper alternatives, such as for example not having to engineer cells but giving vectors or DNA directly to patients, the cost will come down. And of course the more we do, there'll be economies of scale. And so hopefully that this will bring the cost down.
But I think a case can be made for a once off, fairly costly, form of treatment as opposed to the lifelong cost of someone who is HIV positive.
Ravi - Yes I would echo those opinions because there was a time when people thought antiretrovirals were too expensive for Africa. And things change. So I think that not pursuing certain things in medical science, because of cost, is a mistake. We need to do the best science, to show we can do it, and then deal with the cost.

56:17 - QotW: Should you cool down cooked chicken?
QotW: Should you cool down cooked chicken?
Mariana Marasiou has been tucking into this tasty and hot conundrum, from listener Julie. She got in touch with avian infection and immunity scientist Paul Wigley...
Mariana - I reached out to Paul Wigley from the University of Liverpool, who studies food poisoning organisms from chickens, to help me answer Julie’s question.
Paul, what’s the official recommendation for storing food and leftovers?
Paul - As a rule of thumb, cooked food should be refrigerated within 2 hours and eaten within 2 days. Providing that the chicken is thoroughly cooked, it is no riskier to store in terms of food safety than any other meat.
Mariana - Hmm… looks like you’re having a bit of a sore throat. Maybe the next gene therapy should be for laryngitis… While Paul is off to suck a Strepsil, I’ll try to fill in for him.
This food safety tip applies to all cooked food, including takeaway food. This is because the bacteria that can cause food poisoning can form spores, which are resistant to cooking and can germinate to form new bacterial cells when the food is not chilled. While refrigeration doesn’t completely stop the bacteria from growing, it slows it down, which prolongs the freshness of the food, making it safe to eat for a couple more days.
But what about putting the cooked food in the fridge without cooling it down?
Putting very hot food in the fridge raises the temperature inside the fridge and makes it a bit less effective. But you should still aim to refrigerate food within 2 hours of cooking it, even if it’s still a bit warm.
To help food cool down faster, you can split it in smaller containers, and as soon as they’ve cooled to room temperature, they can then go in the fridge.
Related Content
- Previous Quickfire Science of Gene Therapy
- Next A certain uncertainty










Comments
Hi.
Hi.
I am a General Practitioner in South Africa and have a "special needs" child at home, aged 24 years. She was born with her Umbilical Cord wrapped around her neck 3x and probably contributed to her impairment. However she is always asking me questions and listen to almost all I say wrt patients and therapy.
Having heard about Gene Therapy and Stem Cell therapy, on radio Podcasts, she asked me if Medicine will be able to correct her disability with either or both.
I need The Naked Scientist's opinion and assistance.
Rgds and thnx.
GP in South Africa.
Add a comment