Hearts in the Extreme
The Naked Scientist report back from the British Cardiovascular Society's annual conference, finding out how our tickers deal with extreme exercise and environments, from deep under the sea into outer space.
In this episode

01:15 - Athletes' Hearts
Athletes' Hearts
with Sanjay Sharma, St George's Hospital of London, Dr Amanda Varnava, Hammersmith Hospital London
How does repeated exercise impact your heart? Tom Crawford spoke to St George’s University of London heart specialist Sanjay Sharma. He’s the medical director for the London Marathon and also studies how the heart copies with the demands of professional sport…
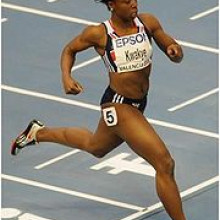
Sanjay - I’ve got a very exciting job. I look after the hearts of football players, tennis players, and most individuals involved with the English Institute of Sport. Clearly, these people push themselves to their limits on a regular basis and exercise probably 10 to 15 times more than the current recommendations and, by doing so, they do develop a constellation of changes within the heart that we sometimes call the athlete's heart. Specifically this involves a 10 to 20% increase in the thickness of the heart muscle and around a 10% increase in the cavities of the heart. The heart relaxes much, much more briskly than a normal heart and contracts more avidly than a normal heart during exercise. These people, because their hearts are very, very big they have quite a slow heart rate at rest because the heart doesn’t have to do very much to pump five litres of blood round the body.
Tom - I’m glad that’s true because I’ve heard that quite a bit and I’ve always wondered whether or not it’s a myth, but as an athlete you generally do have a bigger more powerful heart?
Sanjay - Oh yes you have to. If you think about the fact that whilst we’re sitting down here we are pumping 5 litres of blood round the body. Now when someone exercises that goes up to between 25 to 30 litres of blood round the body. That’s okay if you’re running for a bus and it’s a short dash that’s going to take 20 or 30 seconds, but when you’re running for 2 or 3 hours and you’ve got to maintain that kind of cardiac output, the only way you can do that is with the heart growing in size.
Tom - In that sense the heart really is like any other muscle in your body that by training a particular muscle it grows larger and the heart is no different?
Sanjay - Absolutely. People who train intensively at least 4 hours a week develop some of the changes I’ve just been talking about, and if they stop training things go back to normal.
Chris - The extreme physical demands that sports professionals place upon themselves can have drastic consequences if their heart isn’t working properly. There have been a few recent examples of young athletes and footballers suffering sudden death as a result of an underlying heart problem; sadly these can remain undiagnosed until it is too late. Dr Amanda Varnava is a cardiologist at Hammersmith Hospital, in London...
Amanda - About 1 in 300 of the population will harbour an inherited cardiac condition or a so-called sudden death syndrome. These can be structural problems of the heart where the heart muscle thickens, or the heart enlarges, or electrical problems of the heart where the heart’s structurally normal and the electricity becomes abnormal under certain conditions, particularly under sports and exercise.
Chris - That’s quite high - 1 in 300?
Amanda - Many of these conditions and individual can live with until they’re well into their 90s and not even discover it nor, indeed, get significant symptoms. But certain individual will be at risk with our without exercise - these high risk individuals - and as a cardiologist we see the individuals that we make this diagnosis in and assess whether they’re at high risk or not and counsel them and treat them appropriately. However, an individual who harbours one of these conditions will increase their risk of sudden death by up to 3 or 4 fold by competitive sports, and that’s the issue that we’re dealing with here.
Chris - Do they come and see you or is there a sort of framework for people who are sports professionals, because there is that 1 in 300 risk, are they referred to you just for screening?
Amanda - Individuals come through various mechanisms. One, of course, is if they have symptoms, the second is if they have family history. Certain sports disciplines screen their sportsmen, particularly in football, where the FA have been leaders in this field perhaps because they do attract more money and therefore have the resources to offer. But they certainly are the standard bearers for doing and screening, and by doing a questionnaire looking at family history and symptoms. By doing an ECG and echo we’re able to tease out those footballers who harbour one of these conditions.
Chris - You made an interesting point there because you said “sportsmen,” and football has been very much something that men have participated in for a really long time. Is there very much data on sportswomen?
Amanda - There is data. Reassuringly, as a woman, we have a far less chance of sudden death even with one of these conditions. So, overall, perhaps the risk of sudden death in a female athlete is perhaps up to ten times less than it is for a male athlete - it’s markedly reduced.
Chris - Do we know why?
Amanda - I think that men adapt to exercise in different ways, both structurally and electrically. There are certain groups of men, and certain ethnicities that for various genetic reasons will be at greater risk with a given condition. It is also the case that the sudden death that occurs in females is generally perhaps for the electrical problems and less the structural problems. So there are different conditions that affect athletes, male or female, differently and their risk accordingly.
Chris - What about ethnicity as well because what we’re also seeing is when you go the Olympics people often say that this is in fact a trial of a person’s genetics isn’t it? it’s how genetically they’re set up because it’s always stereotypically can’t be beaten on the marathon, they’ve got the perfect genetic and evolutionary history for that but they’re not terribly good at swimming on the other hand so there’s certainly a strong genetic element. To what extent does ethnicity put you at risk of these disorders?
Amanda - Ethnicity plays a huge role in both the way that the heart adapts in a normal physiological way to exercise, but also according to ethnicity your risk will change, so black athletes, unfortunately, have up to 5 fold greater risk of sudden death due to these concealed conditions than their white peers. And, again, the exact reason for that is unknown - genetic variabilities and genetic risk markers are probably to play
07:48 - Looking inside your heart
Looking inside your heart
with Clare Ward-Jones, Phillips Healthcare
One of the tools available to doctors to see the heart in action is the echocardiogram. This uses ultrasound waves to image the heart as it beats, so the cardiologist can tell whether it’s contracting correctly and that the heart muscle is a healthy shape. Tom Crawford volunteered to be a guinea pig…
Clare - I’m Clare Ward-Jones; I work for Phillips Healthcare and my role is a cardiac ultrasound applications specialist. That means I come into hospitals and train people to use our products. We’ve got a machine the ETHIC and that is the supreme ultrasound machine for cardiology. We can do a 2D scan on you, we can also do 3D images so we can get a 3D model of the heart.
Tom - From my point of view, looking at the machine, it kind of looks like I’m going to go in for a baby scan. So is it the same kind of thing?
Clare - Correct. They’re the same machine with just a different software and a different transducer that we’d use on the machine, but they look identical.
Tom - When you say transducer - is that the bit that you’re rubbing around on me?
Clare - Yeah. The echo probe or the transducer is the bit we put the jelly on we’ll put on your chest.
Tom - What sort of signal is it that’s sent out from this probe?
Clare - They’re ultrasound beams. The ultrasound beams are sent out from the transducer and they will bounce back when they hit structures in the body. So depending on the structures they hit, they come back at different times and that’s what makes up the image on the screen when they’re received back in the transducer.
Tom - Fantastic - Shall we get cracking?
Clare - Yeah. What we need to do first of all is you need to get onto couch and you need to lie on your left side. What that does is it brings your heart closer to the front of your chest wall so there’s less distance for the ultrasound to travel so it should produce a better image on the screen.
Tom - It’s quite comfy actually.
Clare - I’m going to put three stickers on you now to monitor your heart rate while we do the scan.
Tom - Okay. These are like circular plaster with little metal clips on?
Clare - Yes. We call them electrodes.
Tom - These wires you’re clipping to me, they’re going to monitor the electric signal of my heartbeat?
Clare - Yep. You can see this line here - this is your heart rate going along the screen. It give us a number - 87 beats a minute, and each time you see this complex, that’s every time the heart beats you'll see one of those.
Tom - Is 86 normal?
Clare - Normal sinus rhythm is between 60 and 100. Something within that range is what we’d expect.
Tom - Awesome. Good to know.
Clare - This is the ultrasound probe which I’m going to put on your chest. It’s not too big and we’ll put some jelly on this bit here which is the imaging footprint and then that will go onto your chest.
Tom - Almost like a circular probe with a flat bit on the end that I assume is going to be the bit that’s going to be rub rubbed around.
Clare - This is the jelly which is also what you’d use on a baby scan; this gives us a better picture. Ultrasound doesn’t travel through air so we need to get rid of any air between the probe and your skin. It’s a bit cold…
This is where we start the scan and we have the image on the screen here.
Tom - Oh Wow!. That’s literally my heart - that’s amazing.
Rick - My name is Rick Steeds; I’m a consultant cardiologist. I’m particularly interested in cardiovascular imaging and I’m the current President of the British Society of Echocardiography.
Tom - We’re looking at images on the screen here from the echo sound that I’ve just had done of my heart, so could you tell us a little bit more about what it is I’m looking at?
Rick - It’s very good at showing the structure of the heart; how strong the muscle is; whether the valves work; whether they leak or whether they’re narrowed, and whether there’s damage to the heart, for example, from a heart attack. You’ll be glad to know that this looks entirely normal.
Tom - That is very good to hear. We can see two chambers there and there’s a valve between them that is opening and closing with my heartbeat.
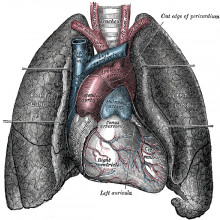
Rick - On the left hand side of the screen you see the two walls of the left ventricle. The main floppy thing in the middle is the mitral valve. Then to the right hand side of the screen you can see the left atrium. So blood comes back from the lungs into the left atrium, down the pulmonary veins having picked up oxygen, it’s passed into the main pumping chamber of the left ventricle. Then just above the mitral valve you can see two leaflets of the aortic valve and then the start of the aorta. So then the oxygenated blood is pumped through the aortic valve, out of the aorta, and then it feeds your brain, heart, and kidneys, and everything else going with it’s oxygen.
At the top of the screen you can see a little bit of the right ventricle, which is the chamber that feeds deoxygenated blood back into the lungs, so that’s where it picks up all of it’s nutrients then back into the heart. This is a great picture of the engine of your body.

12:45 - Supersonic Hearts
Supersonic Hearts
with Gaz Kennedy, Nick Green, Royal Air Force Centre of Aviation Medicine
Fighter pilots shoot across the sky at supersonic speeds and this means that they’re subjected to extreme G-forces such as when they need to turn in a tight circle or rapidly change direction. So how do they handle it? Chris Smith found two people to help him out...
Gaz - Squadron Leader Gaz Kennedy; I work for the Royal Air Force Centre of Aviation Medicine and I’m the officer commanding the aviation medicine flight.
Nick - I’m Wing Commander Nick Green; I’m a defense consultant in aviation medicine. I joined the Air Force in 1990 and I also work at the Royal Air Force Centre of Aviation Medicine.
Chris - Gaz; you’re going to actually dress me up as a pilot. I don;t look like Tom Cruise - not half as good looking as him - but you’re going to give me some of the same gear…
Gaz - Oh I don’t know. We’re starting with a flying suit.
Chris - This looks a bit like a boiler suit that you’re putting me into. It’s quite lightweight material.
Gaz - It’s Nomex, so it’s flame resistant. It’s what Formula One drivers wear.
Chris - I look like I’m going to do the decorating in a bit. Zip that up.
Gaz - The next thing is some angi-G trousers. These will give you protection against pulling G. Basically, they’re a pair of inflatable trousers that connect to the aircraft engine bleed system.
Chris - You're putting a sort of belt round my waist. This is already very heavy Gaz.
Gaz - Yeah, but you get used to it.
Chris - So there’s a belt going round my waist and I look a bit like a cowboy actually with those sort of leathers they used to wear down the outside of their…
Gaz - Chaps.
Chris - Chaps yeah. Absolutely. There’s a hole in the front of it where my knee goes on each side. That’s to enable me to bend my legs presumably?
Gaz - That’s right. On the thigh there are two white plastic rectangles - they’re for writing information down on.
Chris - Now you’re just reaching between my legs and they zip up on the inside of each leg.
Gaz - That’s right. They’re a tight fit - normally, you’d have these put on and they’d be specifically your size and then some safety equipment fitters would tighten up some strings at the back of the trousers and pull them really so they’ve very tight fitting.
Chris - So it’s almost like a victorian corset? There’s a tube emerging at waist height out of these trousers - what’s that?
Gaz - That tubes connect to the aircraft bleed air system that comes from the engine. There’s a spring loaded system there and every time you pull more than about 3G, that opens a valve air comes in the trousers, inflates the trousers, and that stops the blood from pooling your legs to prevent you from going unconscious.
Chris - It’s amazing that you’re actually connected to the jet engine. What are you giving me now?
Gaz - This is a life jacket which we wear every time we go flying, because as well as giving you support over the water, it also contains all the survival aids as well, such as a beacon to locate you, flares, heliograph mirror, first aid kits, spare water. So quite a lot of stuff for carrying around with you.
Chris - I’m now fit to fly?
Gaz - Almost. There a helmet to go on yet.
Chris - Okay. Got the helmet and some gloves, of course. I can't possibly take to the air without my gloves. Just get the helmet on…
Gaz - The oxygen mask on. You won’t be able to speak now but still be able to breath. And you’ve got a visor as well that you can put down that we fly with all the time in case we get a bird strike through the front of the aircraft, and it also gives you protection against the sun as well.
Chris - Nick; why am I wearing all this?
Nick - Exposure to high G-force runs a risk for pilots of loss of consciousness, which we call G-LOC, or G induced loss of consciousness and that’s really because of the effect that the G-force has on your blood. Under increased G, the weight of your blood is effectively increased, and as it gets heavier it has a couple of effects. One of them is to cause the blood to pool in the lower limbs, and the other is to reduce the amount of blood pressure at head level. Basically, anything above heart level we see a reduction in blood pressure, and anything below heart level we see an increase in blood pressure due to the increased hydrostatic gradient caused by the G-force.
Chris - So as the Gs make the blood heavier and effectively fling the blood into my legs, there’s less blood coming back up to my heart, my heart’s got less to pump out into my head and it’s facing a bigger upward struggle to get it into my brain, so my brain basically suffers a lack of oxygen for a while?
Nick - Exactly. And it’s all about the delivery of oxygen to the brain. So we’re not interested in the blood pressure by itself, what we’re really interested in is the flow of blood carrying that vital oxygen to keep you conscious. Around about 4 seconds after the oxygen delivery is stopped you lose consciousness.
Chris - Gaz, you’ve flown some of the most powerful aircraft that the RAF has. Say you’re going to pull a very high load of G, what do you do personally to make sure that you don’t pass out?
Gaz - If you’re aware of it you can perform an anti-G straining maneuver, which is basically muscle tensing just as the Gs about to come on in your legs, buttocks, abdomen. You also take a deep breath, you then hold the breath for between 3 and 4 seconds, and then you exhale and inhale as rapidly as you can within about a second. You want to do probably 2 or 3 of those and then you’re at a level where you can then judge greyout, which is a slight loss of vision and you can relax slightly until you start to greyout and you can retense to get rid of the greyout - the loss of vision.
Chris - Nick; why does that work - the muscle tensing in the legs and then the deep breaths sequence?
Nick - The problem is all about not enough blood pressure and all of these maneuvers are designed to increase blood pressure. The leg tensing has two effects: it acts on the arterial system and squeezes the arteries, particularly the smaller vessels (the arterioles), which increased the peripheral resistance, and it’s actually the peripheral resistance that's the main determinant of your circulation’s blood pressure. So, if you can squeeze those vessels, make them narrow, pressure goes up and that’s what we want. The other convenient benefit of squeezing your legs is blood tends to pool in the veins - they’re floppy elastic vessels, and if you squeeze your muscles hard you can empty that blood out of the veins back up into the chest and then it can be pumped upwards to the heart and to the brain.
Chris - What is Gaz talking about when he mentions greyout?
Nick - Greyout is an interesting phenomenon useful for pilots because it gives them warning that there is a loss of consciousness impending. The reasons that you get greyout is through a failure of blood supply to the retina. The globe of the eye is actually pressurised just to keep the eye in the right shape, but what that means is you need an extra 10 or 20 mm of mercury of blood pressure to perfuse the retina rather than perfuse the brain. In practical terms, if your blood pressure’s falling, your eye stops working before your brain does.
Chris - The first time you were doing all this, Gaz, did you just take to it like a duck to water? Are there people to whom this comes naturally or have you had to learn this and train yourself to become resistant to these effects?
Gaz - There are some people whose anatomy makes them more resistant to G, so short, squat people. I’m not suggesting that I’m molded in that manner. But tall, thin people usually have more difficulty pulling G than shorter, squatter people.
Chris - Have you ever passed out?
Gaz - No. But I’ve flown with quite a few people who have, but it’s nothing to do with my bad flying. That's why we do the training and why it's in a training environment. Because they could go off and do them by themselves next time so at least we’ve discovered that nice and early and realise that they have to then work on their anti-G strain maneuver.
Chris - When people pass out like this Nick, how long do they stay unconscious for ?
Nick - In a study done by the Americans when they went back and looked at their video records from centrifuge training they found it was around about 10 seconds on average, although that did include the time to stop the centrifuge. So in the aircraft it may be a little bit quicker than that you would wake up. But the problem with G-LOC is once you’ve woken up, there’s a period of around about 30 seconds where you’re dazed and confused. You can’t necessarily operate the aircraft. One pilot told me when he was waking up, he looked ahead of him and saw a load of alarm clocks and thought gosh, why did I set all those alarm clocks in front of me? And then suddenly realised it was actually the aircraft instruments and he was in an aircraft travelling at 500 miles and hour, and needed to do something about it. So the confusion is a really important, and yet dangerous, part of the experience.

20:47 - Simulating Operations
Simulating Operations
with Gareth Wills, Vascular Perspectives
Doctors need to practise for years to get good at performing often very tricky procedures. But rather than make mistakes on real patients, modern technology means it’s now possible to rehearse complicated procedures using simulators first. And it can be very realistic, and very stressful, as Tom Crawford found out when Gareth Wills from Vascular Perspectives got him threading a tube into a pretend coronary artery, one of the blood vessels that can become blocked and cause a heart attack...
Gareth - What we’re going to do in a couple of minutes is insert an 035 wire into the radial artery. It’s called an 035 wire because it’s 35 thousandths of an inch in diameter. The radial artery is in the wrist. What we’ll do is we’ll push this wire, which has got a very soft tip, up the radial artery to the forearm where it joins to the brachial artery in the elbow. Up to the top of the shoulder and across the top of the chest where you have the brachiocephalic artery, and then down the descending aorta, which is where it joins to the heart at the aortic root. From that we then push a catheter, which is essentially just a tube, that joins the outside world to the inside world, push that over the wire all the way round to the heart and then we connect a radiopaque dye to the end at the wrist. Using this radiopaque dye, we can inject that into the heart and look at it under live X ray and see the coronary arteries.
And your wire is in the arm…
Tom - I can see it inside the…
Gareth - This is the forearm here so if you start pushing that forward you’ll see it travel up the elbow. It goes very quickly…
Tom - It does wow.
Gareth - You’re up to the shoulder now.
Tom - There’s a huge difference there between how hard I was pushing it initially. Oh God, I can see the heart on the screen.
Gareth - It’s beating which is a good sign.
Tom - So it’s a case of using this wire and the catheter (the tube) to put this dye on the heart so that then when you do an X ray you can see the heart. Because, of course, when you do an X ray normally you just see bones - is that correct?
Gareth - Exactly. X ray only picks up hard tissues and not soft tissues. You’re exactly right, you can see bones, you can see a faint outline of muscle, but what we want to see is the vessels that supply the blood to the muscle. So we use the blood vessels as a conduit to inject the radiopaque dye. The patients who’ll be getting this procedure done generally have angina, which is chest pain at rest or after exertion. If they have chest pain it’s usually because they have a narrowing in one of these coronary arteries, and the coronary artery feeds the blood to the cardiac muscle. If you have chest pain it’s because your heart isn’t getting enough blood to the cardiac muscle. So what we do is we put this catheter in, inject the dye and look for the narrowing.
Now what you need to do is manipulate the catheter to get into this little bubble here.
Tom - It’s like a game. Can I put the syringe down?
Gareth - You can. You can relax as well.
Tom - It’s intense.
Gareth - As you say, in the past, doctors would train on live patients. They would learn at the right hand side of an experienced consultant, generally just by watching, and then they would go through the whole see one, do one, teach one. But nowadays you’ve got systems like the mentes where there is zero risk to a patient, and this is live, or real patient data, so learning with a zero risk strategy seems to make much more sense.
The problem is doctors generally don’t have a lot of time to do simulation on top of everything else that they do so that’s where we try and help out at conferences like BCS where we can offer training like this in an enclosed environment where the doctors have time to do this. But generally, we feel that simulation is obviously the safest, lowest risk way of learning the way to do a proper coronary angiography.
Tom - I know you were telling me to chill out but it feel real, which is good, right?
Gareth - Yeah.
Tom - Because you’re trying to recreate the real world environment that the cardiologist could be in.
Gareth - It’s called immersive simulation. As close to real life as possible.
Tom - I know that was…. I’m terrified.

Crocodile hearts
with Craig Franklin, University of Queensland
Ever wondered how some animals stay submerged underwater for hours at a time? University of Queensland zoologist Craig Franklin studies saltwater crocodiles - the Earth’s largest living reptiles and owners of the most complex heart in the animal kingdom…
Craig - Crocodiles are mostly aquatic. They spend the majority of their life in river systems or sometimes out in the ocean and they are divers. They can spend periods of time underwater, they can catch food underwater like fish, but they can also remain submerged at the water’s edge and ambush prey that come down to drink. Our recent research has shown that they can spend many hours on a single lungful of air, and the record is round about 7 hours.
Chris - That’s a long, long time isn’t it? How do you think they’re doing that?
Craig - The key to diving is how to manage oxygen. For the crocodiles we think a large part of it is their cardiovascular system and their heart is, I think, the most sophisticated, most complex heart in the animal kingdom.
Chris - Quite surprising given they’re quite ancient beings, aren’t they - they’ve been around for hundreds of millions of years?
Craig - Yeah. We can track back to the jurassic and protosuchus is what’s regarded as the first crocodilian. We can jump forward in time into a hundred million years, and in Queensland, Australia a discovery was made of a crocodile that essentially is what we have today in shape and appearance.
Chris - So they're clearly well adapted and very successful. So when you look inside one what is the anatomy that you think gives them this ability?
Craig - Imagine a four chambered heart, just like a human heart - two atria, two ventricles. Blood returns from the body deoxygenated and it enters the right atrium. It then gets ejected into the right ventricle and, as that ventricle contracts, that ejects that blood to the lungs.
Chris - So far that's just like you and me?
Craig - Just like you and me. That blood then returns to the left atrium, then to the left ventricle, and then it’s ejected out to the body, so to the head and to the lungs.
Chris - That’s still just like you and me?
Craig - Exactly. Just like you and me. But this is when it gets a bit more complicated. If we just focus on the right side of the heart, that side of the heart typically ejects blood to the lungs through the pulmonary arteries but, in the crocodile, there’s an extra vessel. It’s called the left aorta, and that vessel allows blood to be pumped to the body so the right ventricle almost has a choice. It can either send blood to the lungs or it can send blood to the body.
Chris - Why would that help?
Craig - Our hypothesis is that if the crocodile can control the amount of blood that goes to the lungs, and perhaps limit it and re-divert it to the body, it can save the oxygen in the lungs. So it kind of meters the amount of blood that goes to the lungs, a little bit like a reservoir, a scuba tank in the crocodiles that it can use from time to time.
Chris - Your theory would be then that the crocodile is going to dive so it gets a lung full of air, then submerges. And then periodically diverts the blood, instead of round its body, through the lungs, grabs a bit of that oxygen, shoves that oxygenated blood round the body for a while until it needs another taste of oxygen and then it opens and closes this choice in the right side of the heart? Is that born out by observation though - do we know that crocodiles do go down with a big lungful of air because diving mammals like whales classically and characteristically breath out before they submerge?
Craig - There’s been experimental studies to show that crocodiles will go down with a lungful of air and use that as a key source of oxygen. But really the trick to this heart, and this flow pattern is how that blood can either go to the lungs or to the body. And what we have discovered is a very special type of valve that sits at the base of the vessel that goes to the lungs. We call it cog teeth because it looks like cog teeth or two sets of knuckles that come together. What we have shown is that when it does close it diverts the blood to the body.
Chris - But have you been able to go in and look at an awake behaving crocodile in order to see if what you think is happening is true because these are not small animals! It’s not like a mouse to study, it’s pretty challenging.
Craig - We have. The great thing these days is that physiologists like myself used to bring the animal into the lab; now we take the lab to the animal. This is the field of telemetry where things like physiological devices are being miniaturised to such an extent that you can implant them in animals and you can actually measure their physiology while they're just going about their daily business.
Chris - So you’ve done that - you’ve got devices you’re implanting in crocodiles to measure these heart functions?
Craig - Yes. We’ve implanted a number of animals and we’ve been recording flows and pressures and there is evidence to say that during diving they do divert blood away from the lungs back into the body.
Chris - It’s ingenious, isn’t it? One quick question I can’t resist though - how on earth do you get the croc to cooperate with the implantation of a device?
Craig - Carefully! Of importance to us is the welfare of the animal. The whole thing is that we want to observe natural behaviours. And so we look after the animal and we make sure that there’s little impact and that way we can record these natural behaviours.
Chris - How do you catch them?
Craig - Catching’s easy. Catchings reasonably easy if you have a very experienced team and I’ve been very lucky in that Australia Zoo, Steve Irwin originally and Terri Irwin now, provides the capacity, the capability to capture these animals and for us to put tracking devices on.

Hearts in space
with Ben Levine, University of Texas
Getting objects like satellites into orbit is relatively easy these days, but living things are a different matter. For instance, what happens to the hearts and blood vessels of the people who go there? That’s what University of Texas researcher Ben Levine has devoted his career to finding out, as he explained to Chris Smith…
Ben - It turns out there was one of the big surprises in the early space years that when astronauts came back down to earth and tried to stand up - they couldn’t, they'd faint. It’s important because many people faint on earth. In fact, 1 or 2% of all emergency room visits are because of fainting. So understanding what the effect of gravity is on fainting was really important clinically on earth, and very important for the astronauts. As we’ve extended the human presence in space on to the International Space Station, we become more interested in long duration space flight and that’s important as you think about what the future of space medicine, or really space science is. The ultimate goal is to get to Mars - that’s a long trip. So understanding what happens to the human body over long duration space flight has been our focus for the past 10 years or so.
Chris What have you learnt?
Ben - There are many things that cause fainting. The most common is what we call neurally mediated fainting. That’s fainting that happens when someone stands up and gravity sucks blood into your feet and so you have to constrict the blood vessels. Think about it like putting your thumb over the edge of a hose to squirt the blood back up to your head. And then you also have to speed up the heart rate - if you want to pump more you’ve just got to pump it faster. It turns out that there are sensors located just at the base of your brain which tell your body oh no, not enough blood getting to the brain. Let’s speed up the heart, constrict those blood vessels and deal with all that blood. Now sometimes the body’s just overwhelmed, and we see that, for example, in a soldier who’s very hot and tries to stand at attention, or someone who’s become compromised because they’ve lost a lot of blood. Even the best of reflexes can’t handle that.
Chris - But, that doesn‘t explain what’s going on in the astronaut because they ought to have a normal volume of blood, so why should they get this drop when they stand up?
Ben - Well that’s a wonderful question. And, in fact, nobody faints in space. Just like nobody faints when they’re lying down in bed except in unusual circumstances. But when astronauts go into space, all the blood that’s normally in the lower part of the body rushes up into the chest. It’s so dramatic the astronauts call that “the puffy face, bird leg syndrome.” The legs get skinny and the face gets puffy. But, just like you and I when you lay down at night, the body doesn’t like all that fluid in the upper body so it gets rid of it . That’s why the first thing you have to do when you get up in the morning is go to the toilet - you get rid of that fluid.
Chris - So you’ve shunted a lot of fluid centrally. This is detected and the body interprets that as I must have too much fluid so it throws it away. The astronauts don’t have too much fluid but the body thinks they do, they throw the excess away so they’ve actually got too little circulating volume.
Ben - That’s right. It’s enough circulating volume in space. It only becomes too little when the stand up on earth, as if they’ve lost a pint or two pints of blood.
Chris - So you put the volume back into your astronaut back on earth. They’ve got the right level of blood now, but does the symptoms resolve?
Ben - After the volume has been restored they quickly return back to normal function. The most frequent time that an astronaut might faint is when they first come down and by two or three days afterwards most of that’s back to normal. For a longer duration flight, it may be more severe and that’s because the heart actually gets smaller. We call it the “couch potato’s heart.” If you don’t do anything to prevent this from happening, the heart will shrink it’s muscle mass by about 1% per week.
Chris - We often see pictures sent down from space of astronauts exercising religiously. If you put them on an exercise regime, can you prevent those losses?
Ben - Fortunately you can, and the astronauts do a pretty good job. Most of them may exercise up to 2 hours a day in space, primarily to protect their bones and skeletal muscle, but exercise works for all the body and it protects the heart as well. There’s much less fainting now than there was in the early days of the space programme.
Chris - What about things like heart disease? We know that when we expose people to doses of radiation for things like cancer treatment it does have a bad effect on blood vessels. There is more radiation exposure from cosmic rays in space - does that accelerate the risk of heart disease?
Ben - That’s one of our biggest concerns. Once you’re outside the protective effect of the Earth’s atmosphere, the radiation exposure is quite dramatic, particularly with solar flares and solar events. It can be extraordinary and we worry about accelerating atherosclerosis. Right now, the best that we can do is to identify those individuals at highest risk and try to avoid flying them, so we’ve introduced coronary calcium scanning. Coronary calcium is a way of measuring the footprint of atherosclerosis in the blood vessels. You take a CAT scan and you measure the amount of calcium which signifies that the atherosclrotic process has progressed. Most of the astronauts that have it right now have a coronary calcium score of zero. There are some legacy astronauts though who have been in the programme before the selection who have a fair amount of atherosclerosis. So figuring out ways to protect them from radiation as they go outside the Van Allen belts will be critical because they’re middle aged men and women. And what is it that kills middle aged men and women? It’s cardiovascular disease.
Chris - A lot of the prediction algorithms we have - when you go to your GP and they measure your blood pressure, they take your cholesterol level - they’re good for older people, but they always say they’re notoriously noisy and bad for younger people. So how good is your NASA algorithm for looking at my coronary arteries and giving me a risk at my age (early 40s) of having a heart attack?
Ben - We were unhappy with the quality of the algorithms and that they weren't very good at identifying risk in younger people. So we’ve combined data from three major databases, some of which include a focus more on younger people to look and to see how much better can we do if we include coronary calcium? And we do a lot better.
Chris - Really? So could this be extrapolated into wider clinical care then so we can start using a measure made for astronauts down here on Earth?
Ben - I certainly hope so. We need to get it accepted by the wider clinical audience and published in the medical literature, and then I hope we’ll have an algorithm app that people can use in their GP’s office.

Scanning your heart
with Michelle Williams, Edinburgh University
What's the best way to look inside your heart? Chris Smith tracked down Michelle Williams, a member of the team at Edinburgh University that have just won the British Medical Journal “imaging team of the year” award for their work on a project called the Scot-Heart study, which could cut heart attacks deaths by half in certain groups of patients....
Michelle - We’ve been doing CT scans - that’s a non-invasive type of scan where you go into a doughnut shaped scanner, lie on your back, and we inject some contrast, some dye, to light up the blood vessels around the heart in order to look for any narrowings or any plaque in those blood vessels that might be causing symptoms of heart disease, or put people at risk of having a heart attack in the future.
We recruited 4,000 people throughout Scotland. Half had CT scans and half didn’t and we followed them up to see what happened to them. We showed that the group that had the CT scans, and the results of the changes in treatment based on the information from those CT scans, had half as many heart attacks or death due to heart attacks than the other group. So that’s a really big difference between the two groups of people.
Chris - Yes indeed; you can be very proud. What were these CT scans showing you that enabled the cardiologist to then make changes to the way those patients were handled to get that dramatic reduction in heart attack risk.
Michelle - CT scans showing us narrowings in the blood vessels and the heart. Previously, in order to identify these things we had to do a test involving a wire being put into a blood vessel in the wrist, fed in towards the heart, and then dye injected around the heart, whereas a CT scan doesn’t involve any of that. There’s a small drip, a venflon, in the arm and then we can use that to put some dye and get the CT pictures, which are kind of like X ray pictures in a 3 dimensional way so that we can see all of the heart and all of the blood vessels.
The Scott heart study looked at narrowings in the blood vessels and what that told us about what happened later on to the patients. But we’re now realising we can actually get more information from the CT scan rather than just about the narrowings because the CT can show the plaque itself that’s causing the narrowings. There’s different types of plaque and some are more high risk and, potentially, people with these high risk plaques might need different treatment or better treatment. That’s what we’re going on to look at next to see if we can identify the highest risk people to make sure they get the best treatment.
Chris - How do the plaques differ?
Michelle - CT scans use X rays and that tells us about the density of the material. We can use that to identify very dense areas that might have calcium in it, or very low density areas that might have fat, or dead cells, or lots of inflammation in them. That can tell us a bit more about what’s going on in the wall of the blood vessel rather than just what narrowing it’s causing.
Chris - Now you’re beginning to ask if we look at enough people, and we’ve got enough of these different types of plaques, we can see which ones are likely to be the high risk ones, which are the lower risk ones, and that gives us even more information about who we need to treat?
Michelle - Yeah, that’s exactly right. That’s our current theory and that’s what we’re going to be working on next so I’ve very excited about finding out what that shows.
Chris - is this cost effective though, Michelle, because that’s a big group of people to be scanning? So what fraction of them might you be able to save from having a heart attack at all and, therefore, what’s the cost of scanning that huge number of people?
Michelle - The beauty of the CT scan is that all of the tests that we do to look at the heart, it’s one of the cheapest. So if it can give us lots of information then that’s a really good one to go for rather than the more expensive, fancier tests. It’s also one with very few side effects - it’s a low radiation dose test. Many people can have it particularly if they can’t go into other different types of scanners for a variety of reasons. In our study we showed that we halve the rates of having a heart attack, or dying from having a heart attack and that really is a big difference so we'll see this increasingly coming into more and more guidelines. The number of CT scans we’re going to do is going to go up and we are going to need more CT scans, more people to look at the CT scans, and more people that can do the CT scans, and that’s going to be a challenge. But it’s not going to be an impossible one because it is going to make a big difference.
Chris - What’s been the reception to your findings and you getting this award? Aee people embracing this - are they going for it, not just in the UK, but internationally: Australia, US, and so on?
Michelle - The reception’s been absolutely fantastic. In the UK it’s already changed national guidelines. In the rest of the world they’re very excited about it as well, particularly in America. At the same time as we did our study there was an American study called “Promise” that was going on at the same time, and the combination of these two studies have shown us really interesting and important things about this population. So around the world it’s been the recipient of quite a number of awards so far and it’s only just getting started I think.
Your heart loves exercise
with Sanjay Sharma, St George's Hospital of London
Could exercise be the best therapy for your heart? Sanjay Sharma spoke to Chris Smith about the wonderful benefits of getting out of the house...
Sanjay - People who exercise are less likely to be obese, less likely to have diabetes, they’re more likely to have a good blood pressure and lipid profile. By controlling all of these acquired risk factors for atherosclerosis, people who exercise moderately reduce the risk of an adverse event from a coronary event by about 50% when they hit their fifth and sixth decade. They live around 3 to 7 years longer than people who don’t exercise. They are less likely to get cancer of the prostate, the breast, the uterus and the colon. Less likely to be depressed and less likely to develop dementia.
Therefore, if you were going to bottle exercise into some sort of pharmacological pill, it would be considered as the miracle pill - something that is free of charge, that can be taken at any time, that’s devoid of side effects, that will reduce consultations with the General Practitioner, outpatient clinics, and reduce bed occupancy. Therefore I believe that every physician in this country should be prescribing some sort of exercise to every single patient.
Chris - It’s quite challenging though, when someone says you should take more exercise it’s quite hard to quantify what constitutes therapy for that particular person. Because it’s clear that taking some exercise has got to be better than no exercise, but is a brisk walk as good as going jogging?
Sanjay - A good point. Again, our Chief Medical Officer recommends that we perform 30 minutes of moderate exercise five times a week. Now that’s a brisk walk or a gentle jog at a 15 minute mile pace. Clearly that data bears fruit and that has been shown but there is also data that if you do a little bit less than that that you will do better than someone who does nothing. But the question is what is the actual ideal dose to prevent things like diabetes, and heart attacks, and stroke?
Now some of the studies that have been published, these are large meta analyses involving thousands and thousands of patients, have shown that to get the best benefit you probably have to do five times the current recommended limit. Now clearly, not everybody can do that. We’ve got people who’ve got musculoskeletal problems, problems with their hearts, and their lungs; they're just not capable of doing that sort of exercise. So the good news for those individuals is that some exercise is certainly better than none. But for those individuals who are able and can exercise, I do not think that just 30 minutes five times a week is enough. They should be trying to do a little bit more than that.
Chris - There’s no risk, if a person does take up exercise, they’re not putting themselves at increased risk through exercise? Because there are some people say don’t overdo it, you don’t want to give yourself a heart attack through sudden, unaccustomed, severe exercise.
Sanjay - Another good point. There is one thing being an accustomed exerciser, someone who’s run most of their lives, or jogged most of their lives, or been a very active individual. And there’s another thing where someone has looked in the mirror in their fifth decade and noticed that their belly is bulging over their belt and decides I need to go to the gym, and I am going to start on day 1 and go on the treadmill and run at an 8 minute mile pace. I don’t think that’s a very good idea.
I think in those people, they need to ask themselves three questions. The first question is do I experience chest pain, am I more breathless than my peers when I walk with them? Have I got a family history of premature cardiovascular disease? And do I have obvious risk factors - am I a smoker, have I got high blood pressure, am I taking tablets for hypercholesterolemia? I think if you’re doing all of that then I would certainly exercise cautiously, gently, to the point that you can hold a conversation but are unable to sing - that would be a good point. I think if you’re going to be trying to do any more than that, I do believe it’s probably worth seeing a specialist to make sure that it’s safe to do so.










Comments
Add a comment