Reinforced skin for amputees, and could E.T. be an AI?
In this edition of The Naked Scientists: Scientists uncover a way to help amputees toughen up their skin to make prostheses more comfortable; Covid mRNA jab pharmaceutical company Moderna turn their attention to vaccines for mpox; and the Astronomer Royal, Martin Rees, on whether ET is really out there...
In this episode

01:00 - Reinforced skin to make prosthetics more comfortable
Reinforced skin to make prosthetics more comfortable
Fiona Watt, European Molecular Biology Organization
The Paralympic runner Richard Whitehead recently told the BBC that NHS prosthetics need to improve to help produce Great Britain’s “next generation” of elite athletes. Richard - who is a double above-the-knee amputee - was referring, in part, to the abrasiveness of uncomfortable prosthetics. It’s long been a problem for amputees because limb stumps are often covered in thin skin that can be painfully abraded when they’re inserted into prostheses. But US scientists may have found a solution. A team at Johns Hopkins University School of Medicine have been injecting connective tissue producing cells called fibroblasts, which they collected from the skin on weight-bearing parts of the body like the feet, and showing that they can toughen up the tissue in the new skin site where they’re injected. It’s early days, but it does suggest that the approach could be used to reinforce the skin in places like amputation stumps, giving users a much easier ride. Fiona Watt, who’s director of the European Molecular Biology Organization, has devoted her life to studying the skin, and she’s been keenly following this development…
Fiona - Every year, unfortunately, a large number of people suffer an amputation. And as you'll know from watching the Paralympics, the quality of artificial limbs now is superb. But the trouble is, if you think about your leg, if you've had an amputation there, what remains of your leg is now in contact with the artificial limb. And that part of your skin was not designed to be weight bearing in the same way as a foot, for example. So what's interesting about this study is the goal is to see if you could convert skin that isn't specialised to bear weight, to skin that can bear weight and can fit a prosthesis. So in other words, converting the skin from like your chest or your arm into that thick skin that you see on your palms and soles. And the hope is that it would stop the pain and the breakdown that happens of the skin in amputees who have to wear a prosthetic limb for a long time.
Chris - How are they trying to do that and how does the thick weight-bearing skin of a foot, for example, differ from the skin that someone will have over an amputation site?
Fiona - The skin in all parts of our bodies has two layers. There's the outer protective covering called the epidermis, and then the underlying, what we call the connective tissue, called the dermis. And the dermis is full of specialised proteins like collagens, which provide bulk and strength if you like, to the skin. And the skin on your palms and soles is specialised for weight bearing. And if you look at your palms, you can see that you've got fingerprints. And the fingerprints represent a way in which the epidermis, the eye covering of the skin, is specialised for grip and to support weight, for example. So in these specialised bits, regions of your body, you've got a thicker epidermis than normal and also the underlying connective tissue is thicker and stronger.
Chris - Is it then a question of just reprogramming the skin on say, an amputation stump to change its characteristics so it looks more like a sole or a palm or is it more involved than that?
Fiona - No, I think you're absolutely right. If you had some way in which you could just flick a switch and change the program from arm skin to the sole of your foot, that would be fine. But of course we are talking about adults rather than a process of development. So different strategies are required. So these scientists lined up some healthy volunteers. Each volunteer agreed to have a small biopsy of skin taken from the scalp or from the sole of the foot. The scientists isolated cells from the skin. And the particular kind of cell they were interested in is a cell called a fibroblasts whose job is to make collagen. So it's a connective tissue cell. They've expanded them in the lab and then they have injected them back into the same individual, but this time injected it into the thigh. And the question is, can those fibroblasts from the different parts of the body change the nature of the thigh skin so that if it's sole fibroblasts, it looks thickened like a sole?
Chris - And did that happen? So when you put this population of foot fibroblasts, so connective tissue making cells, into the thigh, do you get a sort of surrogate big toe on your thigh <laugh> almost? Does the skin change character as you would expect it would If what you're saying is what happens?
Fiona - Well, the skin does change character, but unfortunately not as dramatically as you might have wished. The evidence that it has changed came from measurements like how resistant is the transplanted skin to different sorts of challenges. And mainly it's evidence from taking a biopsy of the transplant side and looking at molecular characteristics which distinguish foot from scalp skin. So this is absolutely not an off the shelf solution for people who have amputations, but it's very important because it's a step in the right direction.
Chris - How do they think then you can optimise it because it shows that it might work if we could make it work a bit better and it will change the characteristic of the skin locally, which would be ideal if you could thicken and toughen up an amputation site skin. Do they suggest how we might go about achieving that?
Fiona - One of the things they showed in their study was that if they take those cells in the dish and subject them to pressure, the foot cells respond differently to the scalp cells. So one idea is that maybe if they had transplanted the cells and subjected them to pressure, which is what would happen in the stump of an amputee, that might help the foot fibroblasts to behave more like they were from the foot.
Chris - Do we have any insights into how they're sensing that and then responding? Because is it not possible, if we can work that out, we can just make cells from anywhere in the body pressure sensitive so you don't have to do the transplant at all.
Fiona - One thing that was shown many years ago, which at the time I was really surprised by, was that if you take fibroblasts from any body site, you can show that they remember where they came from. So that means that encoded in the DNA of the cell, there is a memory that they came from the foot. But I think to make skin, you need a collaboration between the epidermis and the dermis and probably stimulating the signalling molecules in the epidermis, which help, for example, make the fingerprints on the palm would help as well.
Chris - So if you were to do this practically then, would you, if you were performing an amputation on somebody, would you go to the healthy limb that you are not amputating and get the source of cells, these fibroblasts that make the tough connective tissue and have this memory that I'm a foot cell. Would you get that from the healthy site and then put that into the skin that you are fashioning the wound stump from, so that it would kind of pre endow that site with the ability to become almost like a foot. And therefore it would be a better, better match for the prosthesis?
Fiona - Yeah, I think it would be a very good idea. I mean, you can isolate the cells, you can grow them in culture and you can store them for many years so that you could give the stump time to heal and then come in and help repair it. There are many possibilities there.

09:26 - Moderna makes mRNA mpox vaccine
Moderna makes mRNA mpox vaccine
Galit Alter, Moderna
The pharmaceutical company Moderna, who were responsible for one of the mRNA-based Covid jabs developed during the pandemic have now gone on to use this same technology to develop a vaccine against the mpox virus that is causing the current outbreak of mpox in the Democratic Republic of the Congo. Yes there are already vaccines against emerging disease, but they’re in short supply, and they’re more difficult to update if the vaccine needs to change. Indeed, UNICEF - which is the UN’s children’s agency - recently issued an emergency tender for the procurement of more mpox vaccines. Galit Alter is Moderna’s vice president of immunology research…
Galit - The current vaccine that we do have that is licensed for global use, this JYNNEOS vaccine, does provide a hundred percent protection against death in the context of preclinical models and has been shown in clinical trials over the last few years to provide protection also in humans in reducing disease and pathology. And so we do have an incredibly robust tool currently out in the world that is able to curb the potential threat caused by the monkeypox virus. I think the question that we're trying to ask here is, you know, does this additional technology that we now have that can pivot and potentially create vaccines in an accelerated timeline that we know is safe and that we know is highly immunogenic and could potentially focus the response in a more deliberate way because of the way that it trains the immune system? Could this technology help fill a gap in our future response to monkeypox or to other pandemic threats? And so I think what we're trying to understand is really how do we fit in the current world where there is a particular vaccine out there where we can potentially fill those needs that might emerge with time as this virus potentially spreads more aggressively or changes with time.
Chris - How do you pick what to put into your vaccine? Because the way your vaccine works is that you are taking the genetic code that corresponds to a particular part of the virus. So how do you pick that bit of the virus we're going to put into the vaccine?
Galit - Well, that's a really important question and so I think the first thing I always try to explain is that nothing we do is done in isolation. Everything that we do in the context of these pandemic threats is done in collaboration with experts in the field that have been studying these viruses for decades throughout their careers. And so what we did really immediately upon taking on this challenge for monkeypox is to essentially create collaborations with credible figures in the pox viral world who had been studying viruses and understanding which particular components of the virus are the most important targets for protection against disease and infection. And what they had learned over those decades of research that they had been conducting in the laboratory in their animal models was that just four surface proteins that sit on the outside of the virus is really all you need to attack with an immune response in order to prevent the virus from gaining entry into human cells. And what we focused on then, for the next year or so in the laboratory, is working the design these particular proteins so they could express effectively off of our vaccine technology, this genetic code that we essentially deliver to the immune system to actually make sure that when the immune system sees these proteins, they see them in a context that is absolutely perfect to raise immune responses. So we took these designer proteins that we expressed off of our genetic vaccines, and we delivered them into mice. We then challenged these animals to the monkeypox virus. And what we're surprised and elated to see was that this novel technology was able to raise responses and essentially control the virus with an exquisite capacity, both limiting the ability of the virus that caused death, but also really helping to diminish the amount of disease that these viruses can cause within these animal models.
Chris - And when you put this into the body or an experimental mouse, for example, does it make antibodies against those bits of the surface of the virus? Or does it make white blood cells, T cells, that can hit virally infected cells? Or does it do both?
Galit - The beauty of the Moderna mRNA vaccine technology is that we are able to raise both these white blood cell responses that are critically important for helping the immune system to make many, many antibodies that can both block the virus from infecting a future cell, but also to recognise the virus when it's floating around and rapidly clear it from the system, preventing it from causing any further infection or disease.
Chris - What's the longevity of the response like? Because we know that with things like the existing vaccinia based vaccines, the old fashioned way that Edward Jenner would recognise, those tend to be lifelong, those protective effects. Do you think you'll get lifelong protection with this Moderna construct or do you think we'll be going back giving people boosters?
Galit - That's a really important question. With the mRNA vaccines, what we saw in the COVID-19 pandemic is that we saw these very robust immune responses that did decline to some level. But if you look at some of these long-term studies that were done in large populations of vaccinated individuals, what we saw is that this technology really is generating immune responses that can last for a very, very long time. But also importantly, this technology also raises those white blood cells that you mentioned that essentially live for very long periods of time, constantly surveying our body for potential entry of a pathogen. And so we have this long-term immunity built in really both through these white blood cell responses as well as by antibodies that we hope that this novel vaccine technology can help to serve or to fill the gaps for other technologies that are out there.
Chris - How long is it going to take you to get this to market? So you've got something that's regulator approved that could be deployed into the field? Because obviously the crisis we're having is now and we need this sort of solution now.
Galit - Right, so it's important to just mention that this vaccine has not been approved by regulators. We're right now in the middle of a phase one, phase two trial. When in those trials, our goal is to go into healthy populations and ask, are these vaccines safe. With that data, understanding whether we are inducing robust immune responses as well as seeing that these vaccines are incredibly well tolerated at a population level, gives us the essential information that we need then to make decisions about how we can move forward in the context of a licensure trial or commercial deployment.

16:59 - 1 in 4 vegetative patients can still follow instructions
1 in 4 vegetative patients can still follow instructions
Emmanuel Stamatakis, University of Cambridge
An international study has found that one in four patients in a vegetative or minimally conscious state are actually able to follow instructions and perform cognitive tasks. The research was carried out on a large cohort of patients, including a hundred in Cambridge. Emmanuel Stamatakis from the University of Cambridge is part of the study...
Emmanuel - We put these people in an MRI scanner or we fitted what we call an EEG cap, it looks like a hair net with sensors on it on their head. And we measured activity in their brain. Now the activity was in response to something we asked them to do. So we asked them to think they're playing tennis for about 30 seconds, and then we asked them to stop and then we asked them to play tennis again or move their hand. Imagine they're moving their hands. So 30 seconds on, 30 seconds off. We then do a mathematical analysis of this data and we see which part of the brain they use to think they're moving. And if they respond to this task, it means, first of all, they understand language, they understand the instruction, they can retain the instruction, they have what we call working memory, and they can do the task, they can imagine they're moving. So a very complex set of skills is required to carry out this task.
Chris - Quite a while ago, I remember a colleague of yours, Adrian Owen, came on this program and said, to actually some dramatic fanfare, that people who were regarded as completely cut off from the world could communicate in this way. They asked people to imagine giving someone a tour around their house versus, as you say, playing tennis. And they could see the different activations in their brain and they concluded these people were responding meaningfully and that perhaps people we'd regarded as unconscious, not as unconscious as we thought. So what's the question you've asked next then? How have you built on that study from nearly 20 years ago?
Emmanuel - So that original study was carried out in a handful of patients. Now we're having a group of 350 patients. The data from which was acquired from all over the world, mostly northeast US, Paris, Liege in Belgium, Cambridge. So this is the biggest group of patients we have ever looked at to understand whether there is residual cognitive function.
Chris - And what fraction of people who are in that state have this residual cognitive function, then, based on these big numbers you've now looked at.
Emmanuel - So, so far studies with a lot smaller numbers suggested 10% to 20% could respond to these tasks. For the first time with this group of 350 people, we found out that a quarter can respond to these tasks.
Chris - That's a big number. And it's alarming in a number of ways because what this means is that people who we had looked after but perhaps regarded as not really there with us, are probably listening to a lot of what's being said around them and they're thinking, and they would probably love to communicate, but they can't.
Emmanuel - Absolutely. This discovery, this research presents us with a huge number of ethical considerations. You mentioned one of them yourself. Should we have these discussions around these patients? Should we try to perhaps harness what we've discovered and work towards some means of communication?
Chris - Because you can use this almost like a yes no answer system, can't you? Nod for yes, shake your head for no. Because you can ask them questions, look at the brain response, and this means you can have a, albeit limited, but a conversation with these people for the first time.
Emmanuel - Absolutely. The task you mentioned earlier, if one imagines one is playing tennis, the area of the brain you use is quite high in the brain. If you imagine you wandering around the rooms of your house, the area of the brain that responds to this is quite low in the brain. So we have two distinct areas. So yes, in a way we can use that kind of task to respond yes or no. At the same time, with functional imaging, what we can do these days is we decode pictures we look at. So we can look at brainwaves and decide, well, a computer can decide what kind of picture you're looking at. So I don't think it's going to be very far before we can advance this to speech and language.
Chris - Have you had some meaningful conversations with people in this study? The participants as in, apart from just asking them yes or no type things, have you begun to elicit information from them that gives you some kind of insight into what it's like to be in their situation?
Emmanuel - No. At Cambridge, we haven't. I think we will need to, again, going back to the ethical implications of this request, ethical approval before we start doing something like this, but this kind of result may open the way to that kind of study.
Chris - Does it also open the door to better rehabilitation? Because when someone hurts their leg, we give them physiotherapy, we exercise the damaged leg and we restore movement and so on. If someone is regarded as in a persistent vegetative state, there's nothing happening neurologically, we thought, therefore we didn't exercise the brain. Have we missed an opportunity to rehabilitate them? Could we now reopen that door and restore better function for those people?
Emmanuel - There are two directions that research is going on that particular front. We have published work two years ago using, again, functional MRI, suggesting that dopaminergic drugs may be a way forward with this kind of patient.
Chris - These are the same drugs that we give to people with Parkinson's disease. They mimic the action of dopamine.
Emmanuel - Absolutely. At the same time, there's a huge revolution in a way happening with what we call neurostimulation, stimulating the brain with ultrasound or with magnetic waves, non-invasive techniques and invasive techniques where neurosurgeons implant electrodes and we started understanding better what unconsciousness means. So I think the future is bright for this kind of patient.
Chris - You've dwelled on the ethics a couple of times. One of the things that's immediately coming to the front of my mind is that we sometimes, unfortunately in medicine, find ourselves in a situation where we have to make a decision about whether to carry on treating someone. And very often people look at a person who's in a position like this and they say, well, we don't think there's any prospect of recovery. And that influences the decision. Is that going to change then off the back of what you've found?
Emmanuel - I think it should change. I think we have established that we have technology that at least in cases where patients are responsive, can give us additional information than what we have currently, than what medics who take those decisions consider. I think again, in the very near future, we should see changes in this kind of consideration.
23:56 - Why first contact could be with artificial life
Why first contact could be with artificial life
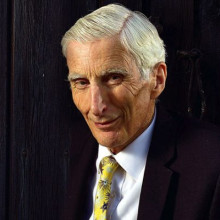
Martin Rees
Earlier this summer, the Astronomer Royal, Martin Rees, delivered a wonderful virtual lecturer to the Starmus science conference in Bratislava. It was about whether we are alone in the Universe. It was so good that we thought you’d like to hear it too, so we got him to record it. Here’s Lord Rees…
We’re all aware that our natural world is the outcome of about 4 billion years of Darwinian evolution. Most people think of humans as the culmination—the top of the tree, but no astronomer can believe that. The Sun’s not even halfway through its life; the cosmos will go on for far longer, maybe forever. Humans may not even be the half-way stage in the emergence of ever more wonderful complexity in the cosmos..
There are chemical and metabolic limits to the size and processing power of flesh and blood brains. Maybe we’re close to these already. But no such limits constrain electronic computers. We are perhaps near the end of Darwinian evolution, but technological evolution of intelligent beings is only just beginning.
Their evolution will be ultra-rapid compared to the timescales of the Darwinian selection that led to humanity’s emergence – but even more billions of years lie ahead. So the outcomes of future technological evolution could surpass humans by as much as we (intellectually) surpass slime mould.
We humans thrive on a planetary surface; but if posthumans make the transition to fully inorganic intelligences, they won’t need an atmosphere. And they may prefer zero-g, especially for constructing massive artifacts. So it’s in deep space – not on Earth, nor even on Mars -- that non-biological ‘brains’ may develop powers that humans can’t even imagine.
Thanks to Prof Mayor and his successors, we know that there are millions of earth-like planets spread through the Galaxy.
Does this aggravate the Fermi paradox? Not necessarily. Some who address this imagine that alien civilsations will be expansionist and aggressive. But even though Darwinian selection has favoured intelligence and aggression, post-human evolution, occurring via ‘secular intelligent design’, need not be aggressive or expansionist. Needing neither gravity nor an atmosphere they would not be on planets. A ‘flesh and blood’ civilization may be detectable for a few thousand years, but its electronic progeny and artifacts could survive for far longer.
The history of human technological civilization is measured in millennia (at most) – and it may be only one or two more centuries before humans are overtaken or transcended by inorganic intelligence, which will then persist, continuing to evolve on a faster-than-Darwinian
timescale, for billions of years. ‘Organic’ human-level intelligence is, generically, just a brief interlude before the machines take over.
Were we to detect ET, it would be far more likely to be electronic where the dominant creatures aren’t flesh and blood -- and aren’t on planets.
Conjectures about advanced intelligence are far more shaky than those about simple life. If it’s evolved on other worlds, with a head-start, I’d conjecture three things about the entities that SETI searches could reveal.
They will not be ‘organic’ or biological.
They won't remain on the planet where their biological precursors lived.
But we won’t be able to fathom their intentions. Maybe it’s the science fiction writers who can teach us most.

What is the shutter speed of the eye?
As you will know, astrophotographers like you make use of slower shutter speeds - literally the time it takes for the shutter of the camera to close across the lens - because it allows more light to reach the camera’s sensor when taking pictures of the dark sky. Otherwise, the stars you’re interested in wouldn’t show up in the photographs. But photographers seeking to capture rapid actions on the other hand opt for faster shutter speeds. Otherwise the light from the moving object would smear across the camera sensor, or, back in the day - the film - blurring the image.
But while they have some similarities to a camera - the lens and cornea focus light to a point on a light-sensitive detector at the back – the retina – and the pupil is the aperture that opens and closes to admit more or less light – eyes work differently.
For a start, the retina itself is not equally light sensitive across its surface; at the centre, it detects colours and picks out images with exquisitely high resolution, but it needs a lot of light to do it, and movement tends to be detected more slowly. Towards the edges, though, where it sees mainly in black and white and with lower acuity, movement is picked up and processed extremely rapidly. That’s why we tend to “catch sight” of things “out of the corners of our eyes”.
The brain, which receives the signals from the retina as a barrage of nerve impulses firing down our optic nerves, also differs in how it responds to the different sorts of signals: movement information is relayed via a faster system so a tennis player can get their racquet in front of an incoming ball faster than they can actually consciously “see” the ball arriving.
Other information though, like faces, objects and words, take longer to be processed and assembled into a picture of the world that can be presented to our consciousness. This happens up to a third of a second after our eyes actually “saw” the scene our brains are now telling us about!
Most scientists agree that the eyes are sensitive to things changing at a rate of up to about 75 frames per second. But because the rest of the visual system is much slower than this, we generally don’t notice, which is why videos playing on youTube at 30 frames per second largely look smooth to us.
So the eye doesn’t really have a “shutter speed” to speak of, but the fastest movement or change you might be able to spot would be in that ballpark, of about one seventy-fifth of a second…










Comments
Add a comment